ADHD
This is a disorder which is characterised by inattention, hyperactivity and impulsivity
– It is much more common in boys than girls and diagnosed in the primary school years
– In order to distinguish this condition from simply bad behaviour, there are 3 key things that must be present in order to satisfy the diagnostic criteria:

–> Persistent – This means that the disruptive behaviour must be constant
– If behaviour does fluctuate, then this could simply be an acute reaction to a change in the environment of the child.
–> Pervasive – This means that the disruptive behaviour must be seen across multiple environments
– If the behaviour was simply concentrated at home, this might suggest that child is not engaging with their parents
– If the behaviour solely exists at school, this might suggest an alternate cause such as bullying which is preventing the child from concentrating and focussing in class
–> Developmental delay – similar to many paediatric conditions, this is a key theme
Symptoms:
– Inattention –> Easily distracted, forgets daily activities, loses possessions, does not listen etc.
– Hyperactivity –> Unable to play quietly, restless
– Impulsive –> Cannot wait their turn, interruptive in class
Diagnosis:
– Clinical history –> For children < 16, must display 6 symptoms. For those > 17, must display 5 or more
– School observation –> This is needed to show that the behaviour is pervasive across different environments
– QB test –> This test measures impulsivity, attention and concentration (key traits affected in ADHD
Management – First is 10-week watch and wait period to see if symptoms resolve
– If symptoms persist –> refer to paediatrician or Child and Adolescent Psychiatrics
– 1st line = parent education and training programme
– 2nd line = Methylphenidate for 6-week trial. Monitor height + weight every 6 months
– 3rd line = Lisdexamphetamine
– 4th line = Dexamphetamine
– If these drugs are not tolerated or the patient has social anxiety give Atomoxetine (SNRI)
– In adults, Methylphenidate and lisdexamfetamine are both used 1st line
N.B. All these drugs are cardiotoxic so must perform a baseline ECG prior to starting treatment.
Encopresis
This is the voluntary or involuntary soiling of undergarments in children older than 4, without an organic cause.
– Whilst it may be due to a serious physical cause, the majority of cases are behavioural
– For example, it could be due to anger (children soil themselves to spite parents) or regression in childhood who are unable to cope with the increasing independence they get, or not learning how to use the toilet properly.
– There are two types: With constipation or without constipation
Diagnosis – Age > 4 years
– Repeated passage of faeces in an inappropriate place (underwear/floor)
– At least one event a month for 3 months
– Behaviour not due to drugs or other medical condition except constipation.
Management – The first thing to do is the exclude a serious biological cause (e.g. Hirschsprung’s disease)
– Put in place regular “toilet times” e.g. try and go after ever meal
– If constipated –> also give stool softening agents and osmotic laxatives to help make egestion easier
– With this combination, you can help push out stool and also train child to go at appropriate times
Prognosis – 90% of cases resolve in a year and almost all resolve by adolescence
Autism Spectrum Disorder (ASD)
A developmental disorder which is more common in males with onset before the age of 3
– It represents a spectrum ranging from mild impairment to severe dependency
– It is thought that children exhibit extreme “male” brains with higher level of systemizing than empathizing.

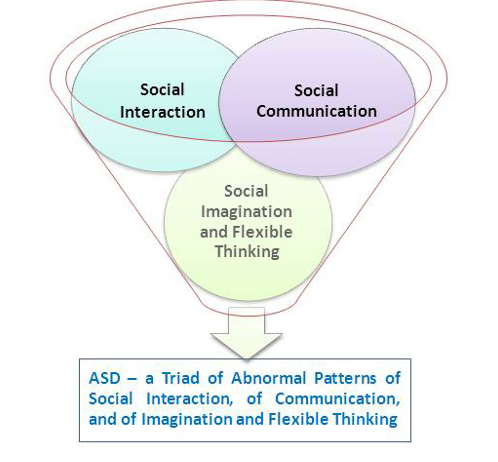
Diagnosis – All 3 should be present for a diagnosis to be made
i) Global impairment of language and communication
ii) Impairment of social relationships
iii) Ritualistic and compulsive features
– In addition, 95% have a low IQ <95
– Also associated with ADHD, epilepsy and other neurological abnormalities
– Some may have isolated skills e.g. (memory, computation) but this is the minority
Management – Multidisciplinary approach to aide education, give independence and improve social skills
– This uses a mixture of behaviour treatments, special education, family counselling
– Medication maybe used to treat comorbidities (e.g. methylphenidate for ADHD) but no primary role
Asperger’s Syndrome
This is thought to be a less severe form than autism which is characterised by more minor functional impairment.
– The diagnosis is only in the ICD-10 and not the DSM-5, and many clinicians do not like the term.
– It typically is diagnosed after the age of 3, whereas autism is diagnosed really early on, marked by the developmental delay especially in social communication.
Symptoms – The main feature is the schizoid personality trait
– Patient is more indifferent to praise or criticism and acts aloof
– They prefer solitary activities and have few interests
– Lack desire for companionship and sexual interactions, with few friends or confidants
– Pedantic speech and pre-occupation with obscure facts
– However, they will usually have normal intelligence and language development
Breath holding attacks
These are short periods of episodic apnoea in children which can lead to a temporary loss of consciousness
– They often occur after a child has got upset or startled – e.g. had a minor bump or a fright
– They occur as part of toddler tantrums as an automatic reaction to something unpleasant
– Unlike seizures, there is no post-ictal phase, no incontinence and the EEG will be normal.
Types:
i) Blue spells (cyanotic) – these are usually precipitated by anger or frustration after a painful experience
– The child cries and then expires forcefully leading to cyanosis, loss of muscle tone and consciousness
– Leads to hypocapnia and hypoxia –> but the child recovers within a minute or two
ii) Pale spells (pallid) – these occur after a painful event and the child turns pale and loses consciousness
– Unlike cyanotic spells, there is little to no crying and these are much rarer
Management – No definitive treatment as the child will eventually outgrow the spells.

