Oesophagus
This is the start of the gut tube, which carries food from the pharynx to the stomach.
– Squamous epithelium lines the oesophagus and provides a protective barrier against wear and tear.
– At the bottom is circular smooth muscle, the lower oesophageal sphincter, supplied by vagus nerve
– The oesophagus has several adaptations to prevent the reflux of acid from the stomach, including an aute entry angle into the stomach (Angle of His), mucus folds and the left crus of the diaphragm
Blood supply:
Inferior thyroid artery (top third), aortic branches (middle third), left gastric artery (bottom)
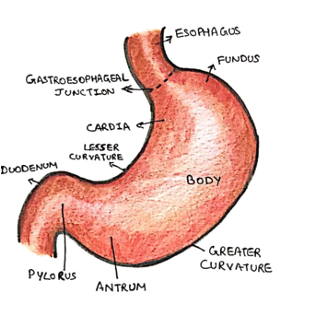
Stomach
This organ stores food, digests it and controls its passage into the intestines.
– Divided into the top fundus, middle body and antrum which continues onto the pylorus
– Parasympathetics (vagus) increase motor activity and secretions and opens sphincter
– Sympathetic supply (greater splanchnic nerve) reduces activity and closes sphincter
Blood supply:
Left gastric (lesser curvature), short gastric (fundus), right gastric artery
The stomach is attached to three layers of peritoneum:
i) Greater omentum:
This is made of 4 layers and attaches to greater curvature to cover bowel
– Known as the policeman and contains a lot of fat
ii) Lesser omentum:
This is a double fold of peritoneum which extends from the liver attach to the lesser curvature of the stomach.
– Contains the foramen of Winslow (containing the portal vein, common bile duct and hepatic artery).
iii) Gastrosplenic ligament:
This attaches the stomach to the spleen
Small Intestine
This is sub-divided into the duodenum, jejunum and the ilium
– The primary role is absorption of nutrients via the villi
– Jejunum forms upper 2/5 of small bowel – it has few lymphoid follicles, thick red walls and wider lumen
– Ileum is terminal 3/5 – it has Peyer’s patches, less vascular mucosa and narrower walls
Blood supply:
Branches of the superior mesenteric artery
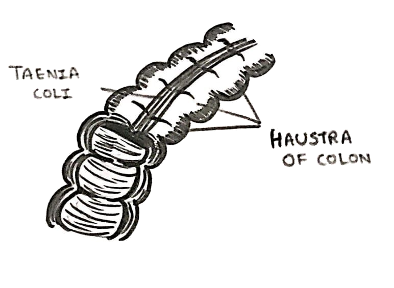
Large Intestine
This runs from the caecum to the anus and has 3 main features:
– Taenia coli = condensations of the longitudinal muscle into 3 bands
– Sacculations/Haustra = folds which do not travel whole width of tube
– Appendices epiploicae = small tags of fat projecting form the wall
– The terminal ileum opens onto caecum and ascending colon.
– This is lined by the ileocecal valve, which is made of circular muscle
Blood supply:
Branches of the superior mesenteric and inferior mesenteric artery
Hepato-biliary
Understanding the liver anatomy is essential to understanding the pathologies, and their associated symptoms.
– From the liver, bile is secreted into left and right hepatic ducts, which unite to form the common hepatic duct.
– It can also be secreted via canaliculi and stored in the gallbladder.
– This is made of fundus, body and neck and contains a pocket called Hartmann’s pouch
– Bile leaves gallbladder via the cystic duct to join common hepatic duct, forming the common bile duct
– This joins with the pancreatic duct to join 2nd part of the duodenum

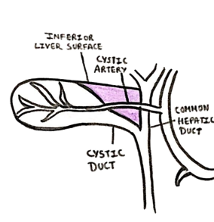
An important landmark regarding the gallbladder is Calot’s triangle:
– Inferior Border = Cystic duct
– Medial Border = Common hepatic duct
= Superior Border = Inferior edge of liver
Calot’s triangle contains the cystic artery which is clamped off during cholecystectomy and lymph nodes
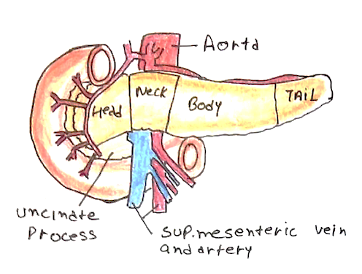
Pancreas
The pancreas is a mainly a retroperitoneal organ lying across vertebral column.
– Has head, uncinate process, neck, body and tail (only intraperitoneal portion)
– The superior mesenteric vessels lie between uncinate process and the neck, making surgery to remove the pancreatic head very difficult
– It functions as an endocrine and exocrine organ. The pancreatic duct joins common bile duct to secrete pro-enzymes into the duodenum
Blood supply:
Splenic and Pancreaticoduodenal arteries
Inguinal Canal
This is an oblique canal which contains important structures
– It is important as it is a natural opening in the abdominal wall, and so a common site for hernias
Anterior wall –> Transversalis fascia, conjoint tendon and the deep inguinal ring
Anterior wall –> External oblique
Roof –> conjoint tendon (the common aponeurosis of internal oblique and transversus abdominis)
Floor –> inguinal ligament and medially the lacunar ligament
Entrance of canal:
– Deep ring, an opening in transversalis fascia above midpoint of inguinal ligament.
Exit of canal:
– The superficial ring, anopening in external oblique, which is protected posteriorly by conjoint tendon
GI Vasculature
The arterial supply of the gut comes from the descending abdominal aorta:
ARTERIAL – This is from the 3 anterior trunks of the abdominal aorta.
a) Coeliac Trunk (divides into 3 main branches):
i) Left gastric artery:
This supplies the lower oesophagus and the lesser curvature of stomach
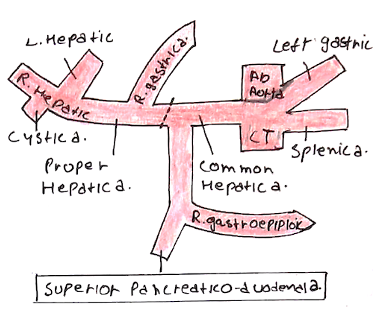
ii) Splenic artery:
This gives short gastrics (supply fundus of stomach) and left gastroepiploic (supplies greater curvature of stomach)
iii) Common hepatic artery. Gives off:
– Right gastric artery
– Gastroduodenal artery –> superior pancreatico-duodenal (1st half duodenum) + right gastroepiploic
– Hepatic Artery Proper –> left hepatic artery + right hepatic artery (gives cystic artery)
b) Superior Mesenteric Artery (has many branches):
i) Inferior pancreaticoduodenal artery:
This supplies 2nd half of duodenum
ii) Middle and right colic artery:
This supplies transverse and ascending colon
iii) Jejunal and ileal branches:
These supply the jejunum and ileum
iv) Ileocolic artery:
This divides into anterior and posterior caecal arteries (gives appendicular artery).
c) Inferior Mesenteric Artery (3 main branches):
i) Left colic artery:
This supplies distal transverse and descending colon
ii) Sigmoid branches
These supply sigmoid colon
iii) Superior rectal artery
This supply the rectum. It forms anastomoses with the other rectal arteries including the middle rectal artery from the internal iliac artery and the inferior rectal artery from the internal pudendal artery.
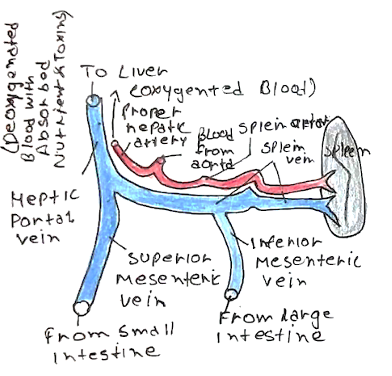
VENOUS:
The venous drainage of the GI system is via the portal vein to the liver.
– The splenic vein and superior mesenteric vein combine to form the portal vein behind the pancreas
– Inferior mesenteric vein joins onto the splenic vein
There are some points of portosystemic anastomoses.
– This is where blood draining into the systemic circulation (which goes directly back to the heart) can mix with blood draining to the liver (for detoxification).
– If portal pressure is raised, then this can push toxic substances into the systemic circulation bypassing the liver
– These substances can lead to encephalopathy, seen in liver failure:
Key sites of anastomoses:
i) Lower third of oesophagus (left gastric vein and azygos vein)
ii) Umbilicus
iii) Lower rectum
iv) Bare area liver
v) Flanks