The thorax is divided by a transverse plane at the angle of Louis (T4/5) into the superior and inferior mediastinum. The latter can be subdivided into the anterior, middle and posterior compartments.
Ribs
There are a total of 12 ribs:
– Ribs 1 to 7 attached to sternum by costal cartilage – “true ribs”
– Ribs 8 to 10 attached to the rib above by costal cartilage – “false ribs”
– Ribs 11 and 12 are so-called “floating ribs,” as do not articulate with the sternum anteriorly
Airways
The airway starts with the trachea which begins, beneath the cricoid cartilage (C6).
Trachea –> main bronchi –> lobar bronchi –> segmental bronchi –> conducting bronchiole –> terminal bronchiole –> respiratory bronchiole

| Structure | Anatomy |
| Trachea | Bifurcates at T4/T5 The bifurcation is known as the carina |
| Main Bronchus | These are referred to as primary RMB = wider, shorter and more vertical LMB = narrower, longer and more horizontal |
| Lobar Bronchi | These are referred to as secondary |
| Segmental bronchi | These are referred to as tertiary They go to bronchopulmonary segments |
Lungs:
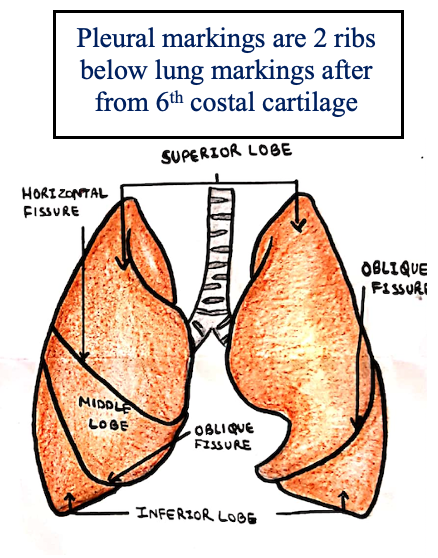
The lungs sit in the thoracic cavity and are split into different lobes by fissures.
– The right lung is shorter, wider and more vertical – hence a foreign body is more likely to pass down this way.
The lungs have specific surface markings which are useful when auscultating the different parts.
– Apex –> 2.5cm above medial third of clavicle
– 2nd costal cartilage –> lungs from both sides meet
– 4th costal cartilage –> left lung diverges to accommodate the heart
– 6th costal cartilage –> lungs lie opposite mid-clavicular line
– 8th costal cartilage –> lungs cross mid-axillary line
– 10th rib –> lungs reach posteriorly on both sides.
Fissures
Oblique fissure: Starts at spine of T3 –> ends at 6th costal cartilage
Transverse fissure (right lung): Parallel to 4th costal cartilage
– The oblique and transverse fissure meet at the 5th rib in the mid-axillary line
– On the left, the middle lobe is replaced by a small lingula
Bronchopulmonary Segments
Each lung is split into 10 bronchopulmonary segments
– Upper lobe – S1-3
– Middle lobe – S4-5
– Lower lobe – S6-10
– In a supine patient, a foreign body is more likely to enter right apical lower lobe segment
– In standing patient, a foreign body is more likely to enter a basal segment of lower lobe
Pleura
Both lungs are covered by 2 pleural layers which have a closed intrapleural space, needed for breathing
– Visceral layer – this is the layer that lines the lungs
– Parietal layer – lines the thoracic wall, upper diaphragm and sides of the mediastinum.
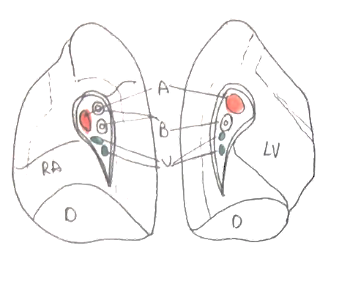
Hilum
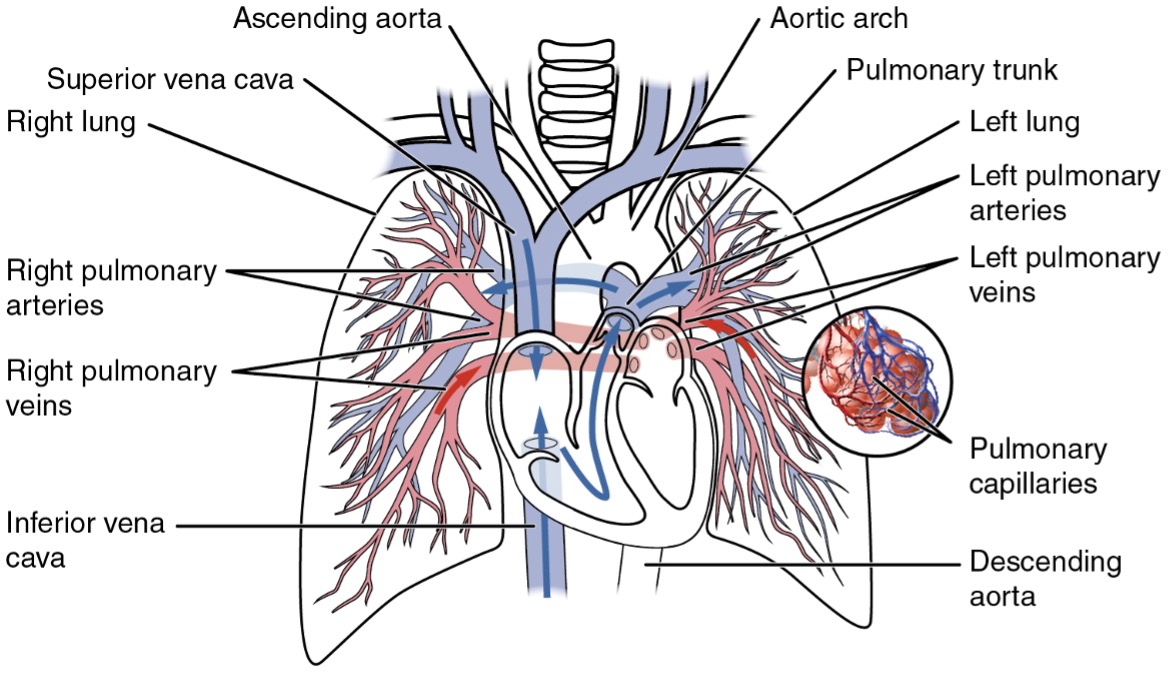
One of the most important structures of the lung is the lung hilum. This has a variety of structures which are needed for respiration.
– Arteries (pulmonary + bronchial) lie superiorly
– Veins lie anteroinferior
– Bronchi lie posteriorly
Neurovascular supply and lymphatics
Blood supply
– Pulmonary arteries -> supply deoxygenated blood for gas exchange
– Bronchial arteries -> supply oxygenated blood to the bronchial tree
Nervous supply
– Vagus -> cause bronchoconstriction: ACh on M3 receptor – Gq coupled (parasympathetic)
– Thoracic sympathetic chain -> cause bronchodilation – Na on B2 receptor – Gs coupled (sympathetic)
Lymphatic supply
The lymph drainage of the lungs runs along the bronchi and under the pleurae.
– These converge on lymph nodes at the lung hila (bronchopulmonary nodes)
– These then drain to nodes around the carina (tracheobronchial nodes)
– This drains to mediastinal nodes –> terminate into the thoracic duct/right lymphatic duct
In the superior mediastinum, the key features are the major blood vessels and thoracic duct.
Aortic arch:
This gives off three major branches:
– On the right -> brachiocephalic trunk (divided into right subclavian and right common carotid artery)
– On the left -> left common carotid and subclavian arteries
SVC:
The subclavian and internal jugular vein unite forming the brachiocephalic vein at sternoclavicular joint
– The SVC is then formed by the union of the brachiocephalic veins behind the first costal cartilage
– This drains into the right atrium at level of 3rd costal cartilage
Thoracic duct:
This enters the junction of the left subclavian and left internal jugular vein