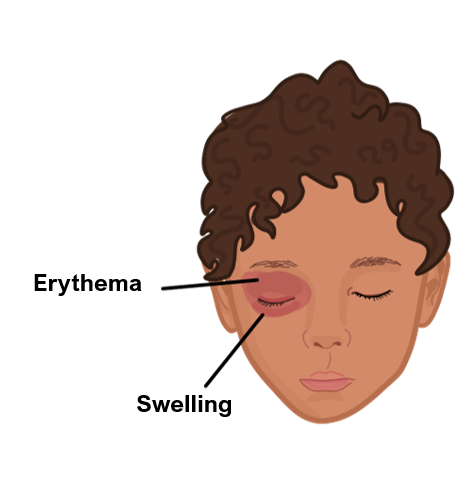
Orbital Cellulitis
This is an infection of the structures which lie behind the orbital septum.
It is usually seen in young children. It is more severe than pre-septal cellulitis and will have worse symptoms (e.g., proptosis, ophthalmoplegia).
Patients usually have a history of an URTI (e.g., sinusitis) or pre-septal cellulitis.
Symptoms
Redness and swelling around eye with pain
Painful eye movements
Proptosis (bulging of the eye)
In preseptal cellulitis, you do not get reduced visual acuity or painful eye movements
Key tests
Bloods show raised inflammatory markers
Blood cultures to assess for bacteremia
CT with contrast of the orbit
Management
IV antibiotics
Cataract
This refers to clouding of the lens which leads to a progressive reduction in vision.
It is a significant cause of blindness worldwide.
It mostly occurs due to age, but can be accelerated by factors such as trauma, smoking, diabetes and steroids.
Symptoms
Progressive reduction of vision with increased glare and halos around lights
Faded colour vision, but there is not usually pain or severe irritation to the eyes
Absent red reflex – cataracts prevent light from getting to the retina, so red light is not reflected back
Key tests
Slit lamp examination shows visible cataract
Fundoscopy will show normal retina and optic disc
Management
Surgery (e.g., phacoemulsification uses ultrasound to break up the cataract)
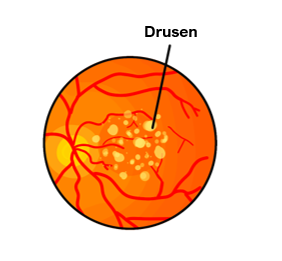
AMD (age-related macular degeneration)
This is the most common cause of blindness in adults in the UK, which is due to progressive damage to the macula cells in the eye.
There is accumulation of drusen, small yellow deposits of lipids, between the retina and choroid, which damages the retina over time. This is known as dry AMD.
In addition, there can be abnormal vessel growth on the retina causing leakage of fluid/blood that further damages the retina. This is known as wet AMD.
Risk Factors
Age
Smoking
Positive family history
Symptoms
Blurred vision in the centre of the visual field, making it harder to see nearby objects
Difficulties in dark adaptation
Increased glare around objects
Key tests
Slit-lamp microscopy – identifies changes affecting the retina
If wet AMD is suspected – angiography is used to see new abnormal vessel growth
Management
For dry AMD – no curative treatment available
For wet AMD – VEGF inhibitors e.g., bevacizumab is used to prevent vessel growth
Anterior Uveitis
This is a condition which describes inflammation of the uvea, the vascular middle layer of the eye that separates the outer fibrous sclera from inner neural retina layer.
It results in the accumulation of inflammatory cells and debris which appear as a fluid level (hypopyon) in the anterior chamber of the eye.
Risk factors
HLA-B27 arthropathies
Inflammatory bowel disease
Behcet’s disease
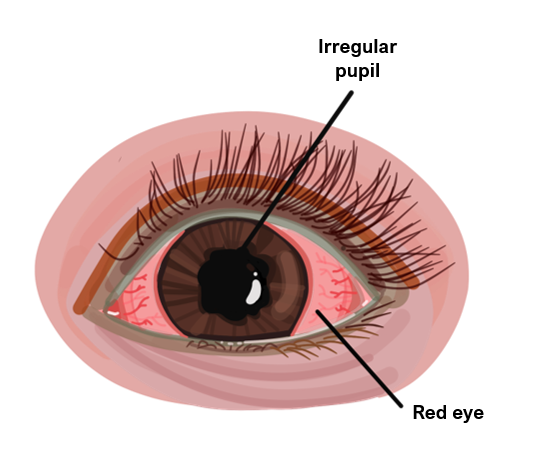
Symptoms
Acute onset of red eye with ocular pain and lacrimation
Pupil is small and irregular
Blurred visual acuity with photophobia and hypopyon
Management
Urgent referral to ophthalmology
Steroid eye drops and mydriatic eye drops (e.g., cyclopentolate)
Glaucoma
This is a group of diseases characterized by raised intraocular pressure which damage the optic nerve:
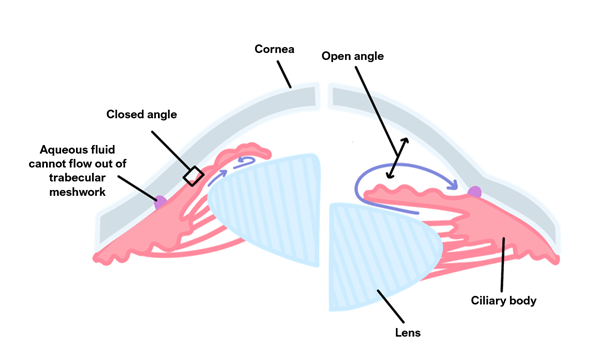
Open-angle (chronic) glaucoma
This is the commonest form of glaucoma due to clogging of the drainage canals.
The iridocorneal angle between the iris and cornea remains open but the trabecular network is obstructed raising intraocular pressure.
It develops slowly and is a lifelong chronic condition which progresses with age.
It is associated with a positive family history, diabetes, steroids and hypertension.
Symptoms
Decreased visual acuity over time with optic disc cupping
Peripheral visual field loss leading to “tunnel vision”
Management
Refer to ophthalmology
1st line medication is prostaglandin eye drops (e.g., latanoprost)
If unsuccessful, can use topical beta-blockers (timolol), carbonic anhydrase inhibitors (e.g., dorzolamide) or sympathomimetic eye drops
If uncontrolled, options include laser (trabeculoplasty) or surgery (trabeculectomy)
Angle-closure (acute) glaucoma
This occurs due to the acute blockage of drainage canals, causing an acute increase in intraocular pressure over a very short time frame.
There is a closed or narrow iridocorneal angle.
The disease progresses quickly and visual acuity decreases very noticeably.
Symptoms
Severe pain around the eye giving a hard red-eye
Decreased visual acuity with halos around lights
Semi-dilated non-reactive pupil and hazy cornea
Symptoms are more noticeable when the eye is dilated (in the dark)
Management
Urgent referral to ophthalmology
IV acetazolamide and pilocarpine drops (to constrict the pupil)
Painless Loss of Vision
There are a group of conditions which are characterised by a sudden painless loss of vision:
Retinal Detachment
This is where the retina detaches leading to an acute, painless loss of vision. It is usually due to a break in the retina which allows the eye fluid to get behind the retina.
It can be preceded by posterior vitreous detachment which is the separation of the vitreous membrane from the retina.
This can give rise to blurred vision, floaters and flashes of light in the visual field.
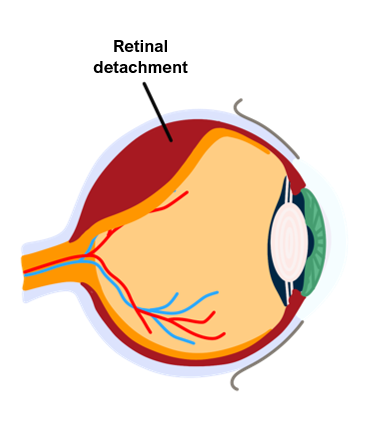
Symptoms
May have symptoms of vitreous detachment, e.g., floaters and flashes of light
Presents as a shadow that starts on the edge of the visual field moving inwards like a dark veil
Painless loss of vision
Straight lines may appear curved
Management
Surgery to restore the retina
Central Retinal Vein occlusion
This is a blockage of the central retinal vein (more common than arterial occlusion).
The incidence increases with age, but it also occurs secondary to conditions like glaucoma, hypertension and polycythaemia.
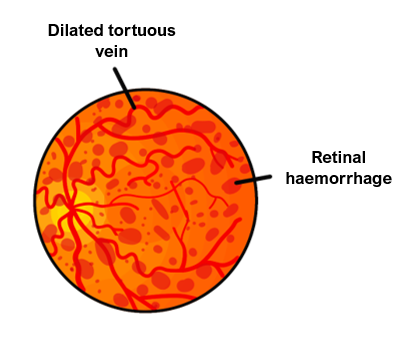
Symptoms
Acute, painless loss of vision
It can be preceded by blurring of vision, worse on waking, which improves duringthe day
Key tests
Fundoscopy shows retinal haemorrhages
Management
Includes laser treatment and anti-VEGF injections
Central Retinal Artery Occlusion
This is a condition which occurs due to a blockage of the retinal artery, which originates from the ophthalmic artery and supplies the inner retina and optic nerve.
It is due to conditions which disrupt vascular structures, e.g., carotid artery disease, atherosclerosis, diabetes and giant cell arteritis.
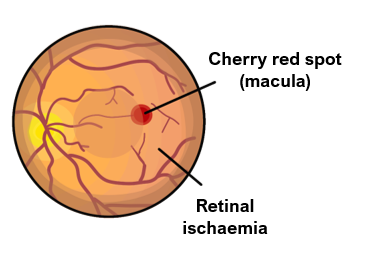
Symptoms
Acute, painless loss of vision
Afferent pupillary defect (pupil constricts less in response to light)
Key tests
Fundoscopy shows an apparent red lesion amidst a pale surround retina (“cherry red spot”)
Management
Options include fluid removal to lower pressure, hyperbaric oxygen, ocular massage
Vitreous Haemorrhage
This is a caused by bleeding into the eye, which causes painless loss of vision.
The most common underlying cause is diabetes, which causes abnormal blood vessel growth on the retina. These vessels are much weaker and are prone to tearing.
It can also occur secondary to trauma, retinal tears or detachment.
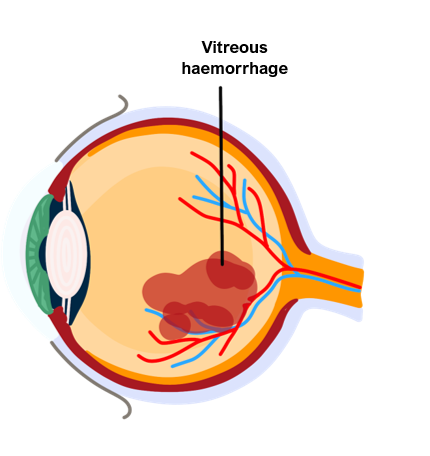
Symptoms
Acute, painless loss of vision or blurry vision
May experience floaters, faint cobweb-like apparitions in the field of vision
Flashes of light in the peripheral vision
Key tests
Fundoscopy – inability to visualise the retina due to blood blocking the light
Management
If the haemorrhage is small, treatment may not be required
In severe cases, options include vitrectomy, cryotherapy and laser photocoagulation

