Tumours of the brain can be primary or metastases from other origins.
Metastases usually present as numerous, well demarcated lesions.
They are typically seen at the grey-white matter junction and originate from lung, breast, kidney cancer and malignant melanomas.
The classification of primary tumours can be divided according to type of cell: e.g., astrocytes, oligodendrocytes.
In adults, the most common primary tumours are glioblastoma multiforme, meningiomas and schwannomas.
In children, the most common primary tumour is a pilocytic astrocytoma.
Symptoms
Initially painless as the brain lacks nociceptors (meninges have nociceptors)
Pressure symptoms – headaches (worse on waking, bending over), nausea/vomiting
Seizures (often first sign) and focal neurological deficits
Can affect memory and cause changes to personality/mood/concentrati
Key tests
Imaging e.g., CT/MRI with contrast visualises tumour
Definitive diagnosis requires a biopsy
Management
Involves neurosurgery (if possible/single lesion) +/- chemo/radiotherapy
Glioblastoma Multiforme (GBM)
This is a high-grade tumour of astrocytes which is the commonest primary malignant brain tumour in adults.
Astrocytes are a subtype of glial cells and have a characteristic star shape.
They form the physical structure of brain and perform functions like secretion, maintenance of the blood-brain-barrier and regulation of neurotransmitters.
This tumour is usually caused by mutations causing upregulated epidermal growth factor receptor (EGFR).
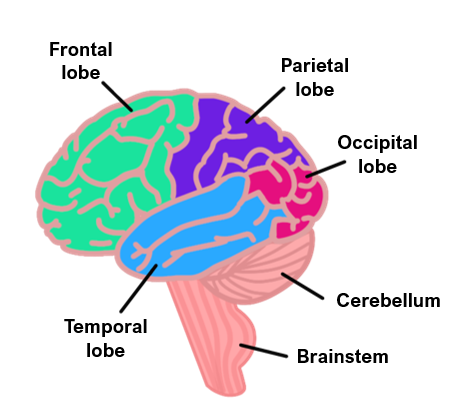
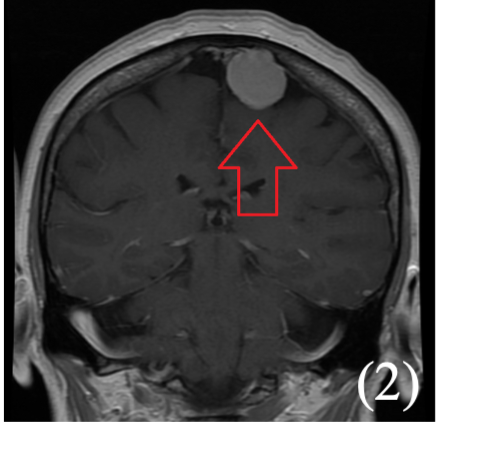
It usually arises in the cerebral hemispheres near the corpus collosum.
It is very difficult to treat due to chemotherapy resistance.

Key tests
CT/MRI shows a classic “butterfly lesion” across the corpus callosum
Histology – central regions of necrosis surrounded by tumour cells. Cells are GFAP protein positive and have tumour markers EGFR and isocitrate dehydrogenase
Management
Mainly supportive for symptomatic relief (anticonvulsants and corticosteroids)
Surgical resection if suitable
Meningioma
A benign slow growing tumour of the arachnoid cells which make up the meninges.
It is the commonest benign CNS tumour in adults.
They have a higher prevalence in women and are considered rare in children.
The tumour can compress the tissue but does not invade the brain.
It is associated with increasing age, radiation therapy, positive family history and neurofibromatosis type 2.
Causes
Radiation therapy
Family history
Neurofibromatosis type 2
Symptoms
The tumour can compress the tissue, but never invades the brain
Many cases are asymptomatic and are incidental findings on autopsy
Commonly present as focal seizures
Can give focal deficits e.g. visual problems, muscle weakness, loss of bladder (depending on location)
Key tests
CT/MRI shows well demarcated mass attached to the dura mater
Histology – psammoma bodies (collections of Ca2+) may be present
Management
Surgical Resection
Acoustic Neuroma (Schwannoma)
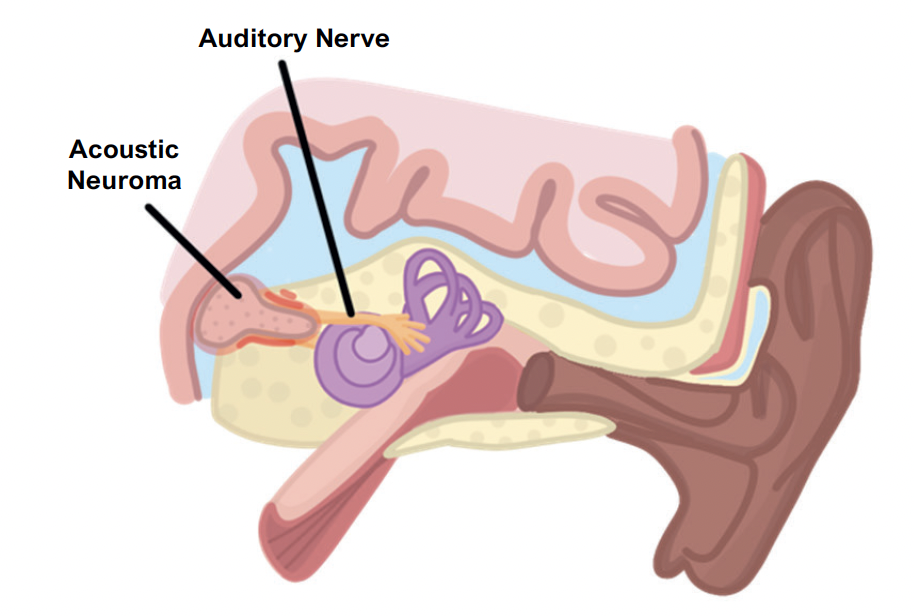
This is a vestibular schwannoma, a tumour of the myelin producing cells of the vestibulocochlear nerve
Associated with neurofibromatosis type 2 (gives bilateral neuromas) and the cells are S-100 positive.
Symptoms
The tumour causes symptoms due to compression of local nerves
CN V – loss of the corneal reflex
CN VII – Facial nerve Palsy (paralysis)
CN VIII – Vertigo, unilateral sensorineural hearing loss and tinnitus
Key tests
MRI of the cerebellopontine angle (shows a vestibular “tail”)
Biopsy shows hypercellular areas of spindle cells with hypocellular myxoid areas
Management
Surgery (although can lead to irreversible hearing loss and facial palsy)
Oligodendroglioma
This is a tumour which originates from the oligodendroctyes (myelin producing cells) of the brain
Can be grade 2 (growing very slowly and benign) which occurs in adults around the age of 40.
Can be grade 3 (malignant) which are called anaplastic and more common in elderly patients.
Most commonly in the frontal lobe giving general symptoms of raised ICP, with seizure often first sign
Key tests
CT/MRI imaging shows calcifications in the white matter
Histology –shows “fried-egg” appearance of cells

