What is a posterior prolapse?
A posterior prolapse is a bulge in the back wall of your vagina. It is caused by weakness of the support tissues between your vagina and your bowel.
What are the benefits of surgery?
A posterior prolapse can cause the following problems.
- A sensation of ‘something coming down’.
- A bulge in your vagina, which can cause discomfort when having sex and difficulty keeping a tampon in.
- The feeling of not having fully emptied your bowel.
- The need to press on the back wall of your vagina to fully empty your bowel.
The aim is to tighten the support tissues between your vagina and bowel, and remove any bulge in your vagina.
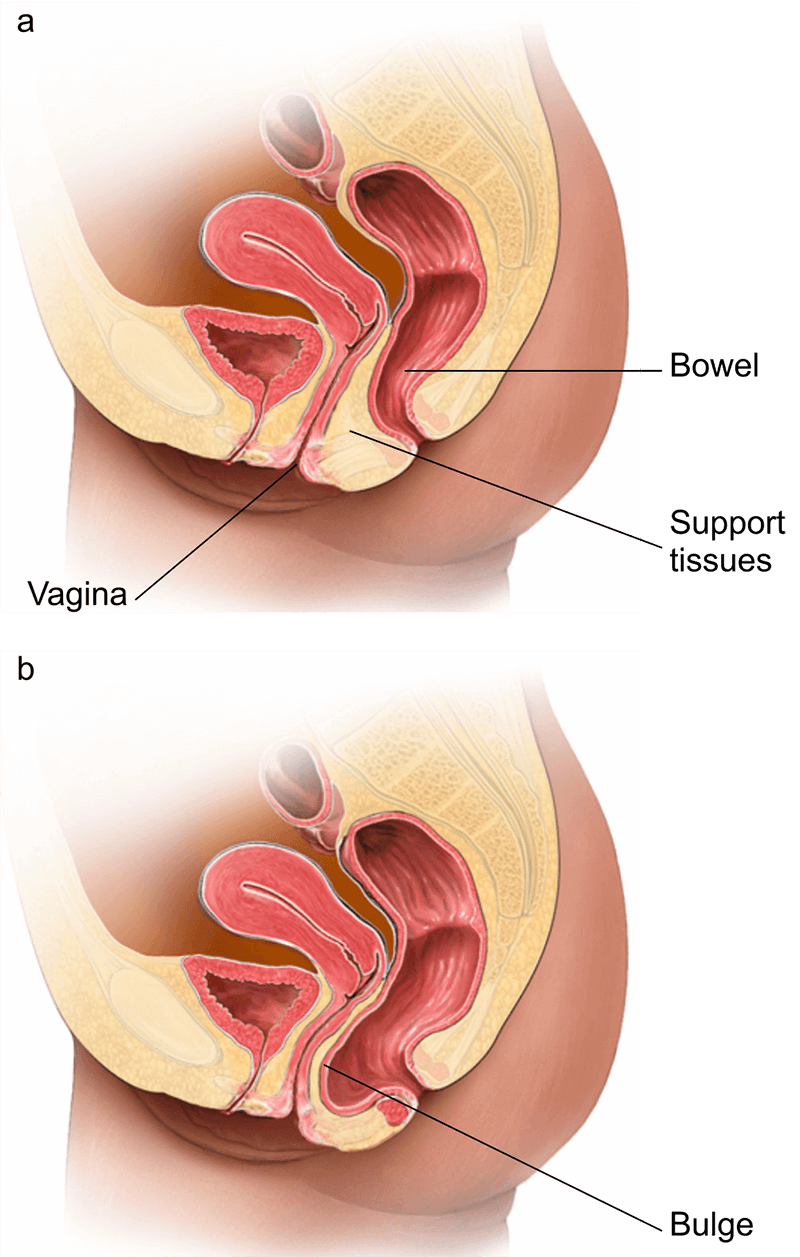
b) A posterior prolapse
Are there any alternatives to a posterior repair?
If you have only a mild prolapse, your doctor will usually recommend that you have a posterior repair only after you have tried simple treatments.
- pelvic-floor exercises
- treating any constipation
- vaginal estrogen cream
- placing a pessary
Alternatively, you can choose to have no treatment and monitor your symptoms.
What will happen if I decide not to have the operation or the operation is delayed?
A prolapse can seriously affect your quality of life but is not life-threatening. A prolapse may slowly get larger, eventually appearing at the entrance of your vagina.
If you have only a mild prolapse, your doctor may be able to recommend an alternative treatment for you.
If you experience any of the following symptoms, contact your healthcare team.
- Unusual bleeding.
- The prolapse becoming more prominent.
- A change in your bladder or bowel control.
What does the operation involve?
The operation is usually performed under a general anaesthetic but various anaesthetic techniques are possible. The operation usually takes about 30 minutes.
Your doctor will examine your vagina. They will make a cut on the back (posterior) wall of your vagina so they can push your bowel back into place.They will use stitches to tighten the support tissues along the length of the back wall of your vagina. Your doctor will need to cut away a small part of your vaginal wall so they can remove excess tissue.
How can I prepare myself for the operation?
If you smoke, stopping smoking now may reduce your risk of developing complications and will improve your long-term health.
Try to maintain a healthy weight. You have a higher risk of developing complications if you are overweight.
Regular exercise should help to prepare you for the operation, help you to recover and improve your long-term health. Before you start exercising, ask the healthcare team or your GP for advice.
Speak to the healthcare team about any vaccinations you might need to reduce your risk of serious illness while you recover. When you come into hospital, practise hand washing and wear a face covering when asked.
What complications can happen?
Some complications can be serious and can even cause death.
General complications of any operation
- feeling or being sick
- infection of the surgical site (wound)
- allergic reaction to the equipment, materials or medication
- bleeding
- venous thromboembolism
- chest infection
Specific complications of this operation
- damage to your bowel and surrounding structures
- difficulty opening your bowels
- developing a collection of blood (haematoma) between your vagina and your bowel
- difficulty having sex
- recurrent prolapse
- new prolapse
- heavy bleeding which requires a blood transfusion or another operation
Consequences of this procedure
- pain
- unsightly scarring of the skin
How soon will I recover?
You should be able to go home the same day. However, if you have a drip, pack or catheter in place, you may need to stay overnight.
Rest for 2 weeks and continue to do the exercises that you were shown in hospital.
Do not have sex, use tampons, or go in the bath, swimming pool or hot tub for at least 6 weeks and not until heavy bleeding and discharge have stopped.
Do not stand for too long or lift anything heavy. You can return to work once your doctor has said you are well enough to do so (usually after 6 to 8 weeks). You should be feeling more or less back to normal after 3 months.
Regular exercise should help you to return to normal activities as soon as possible. Before you start exercising, ask the healthcare team or your GP for advice.
Continue your pelvic-floor exercises as soon as possible and keep doing them for life.



