What is peripheral vascular disease?
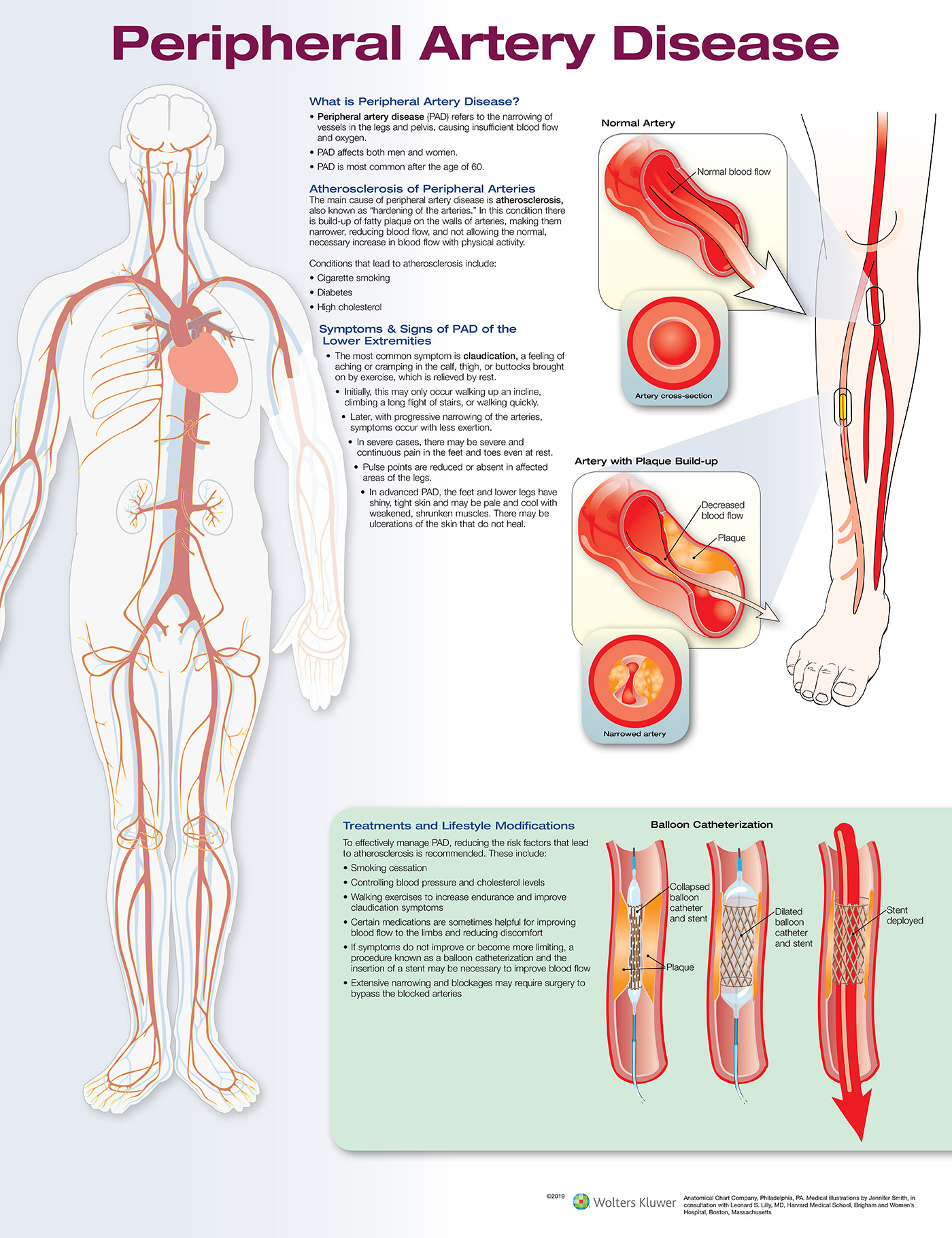
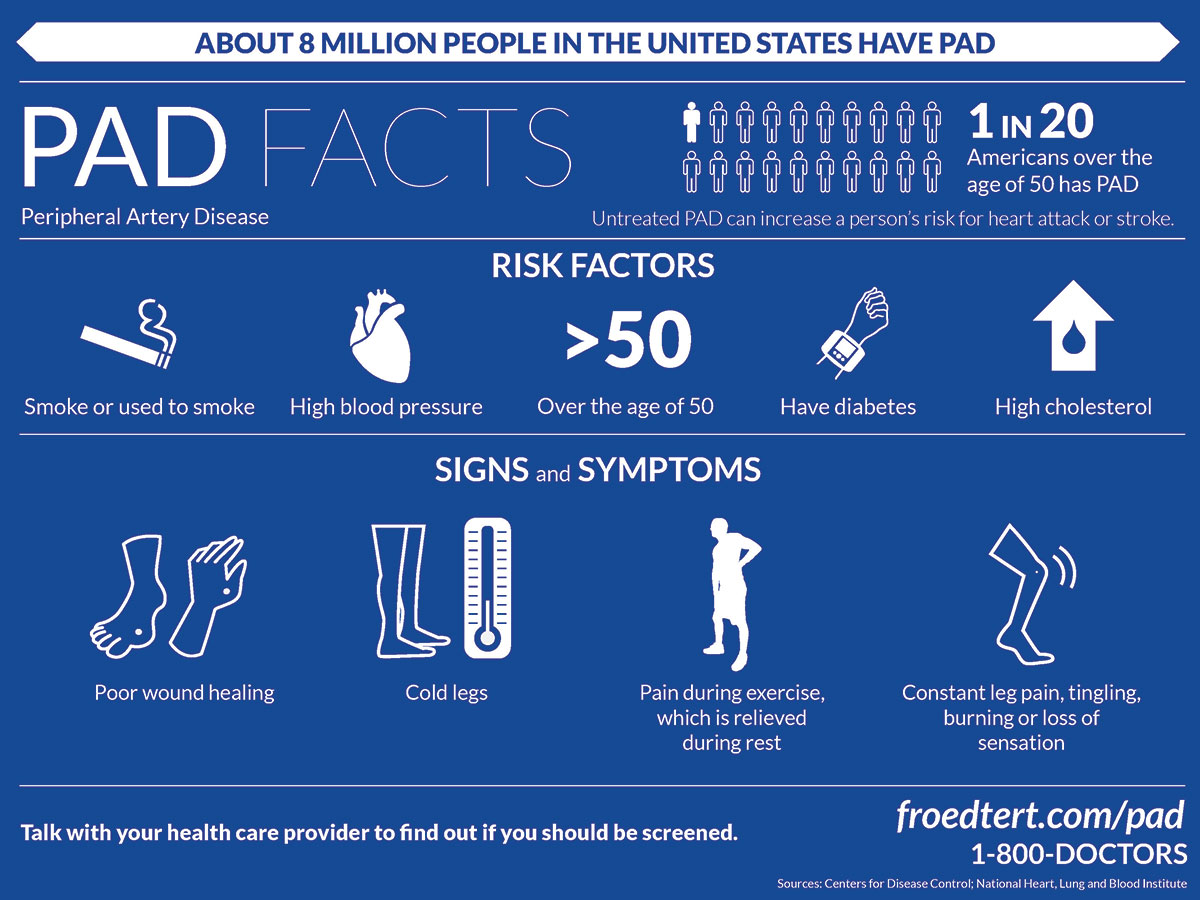
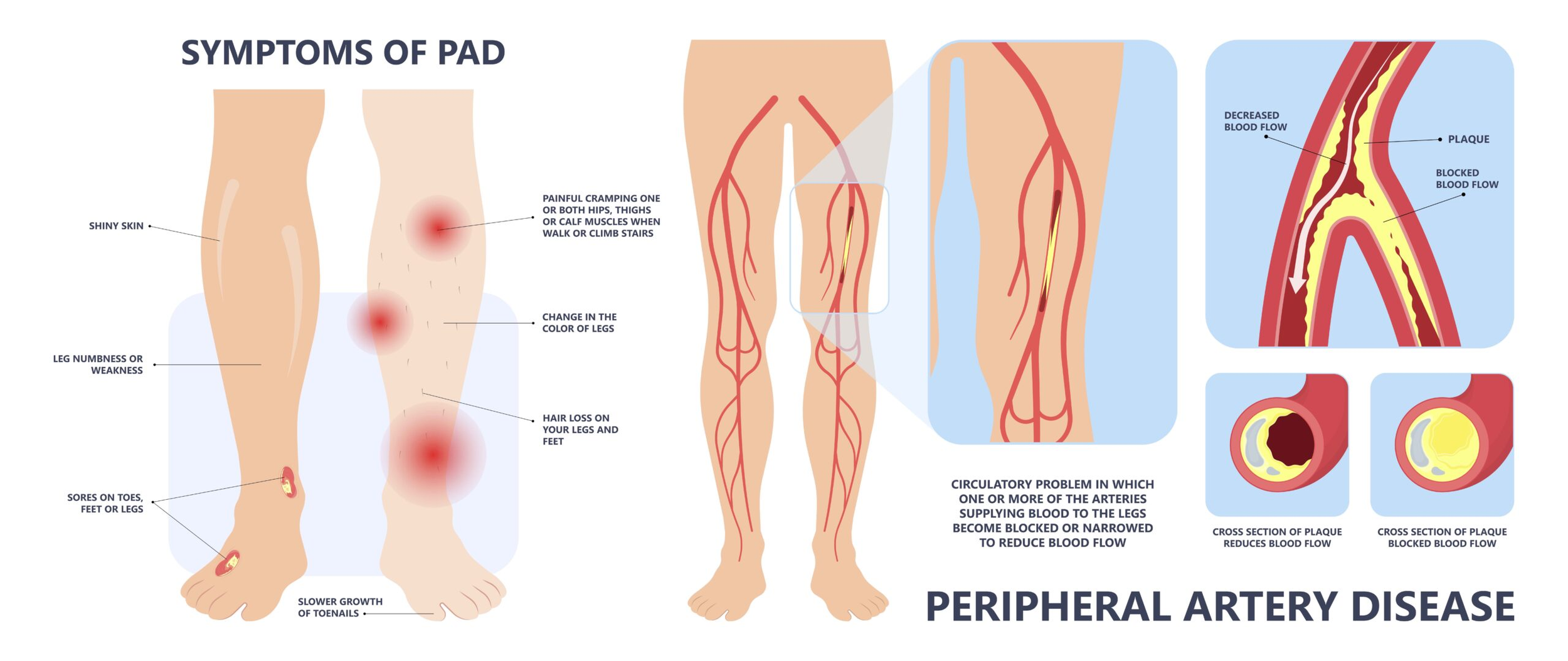
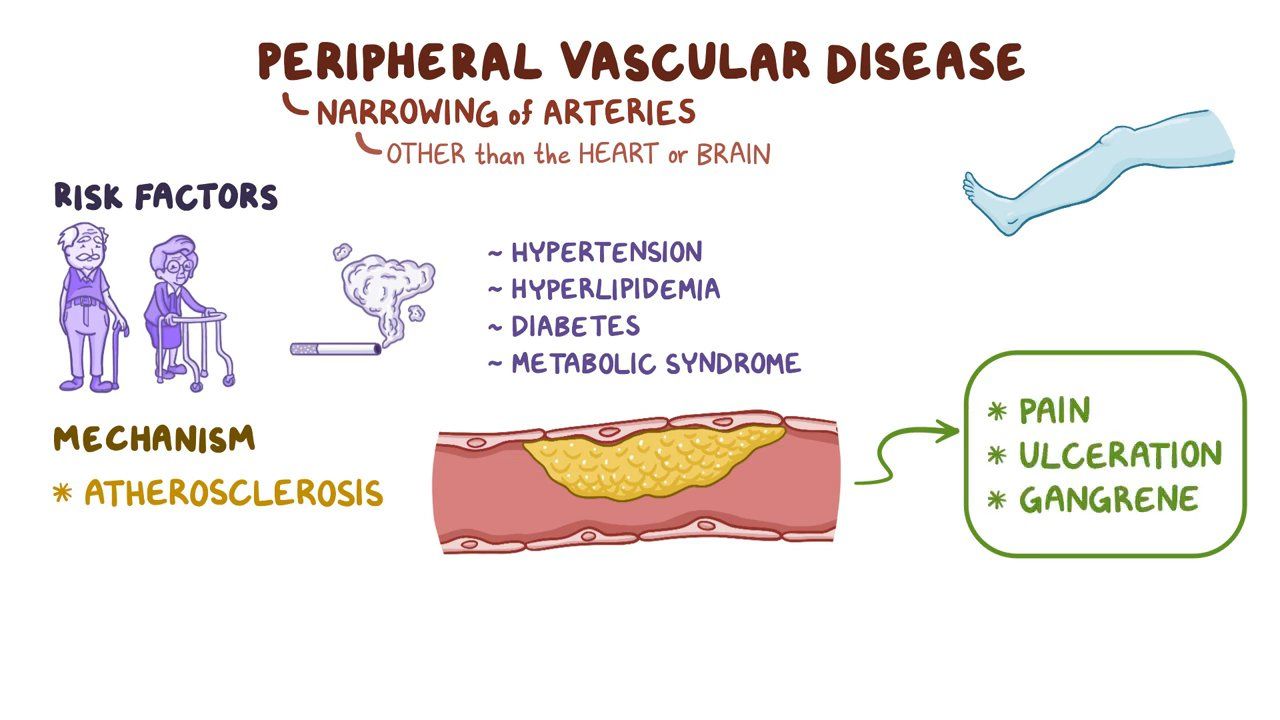
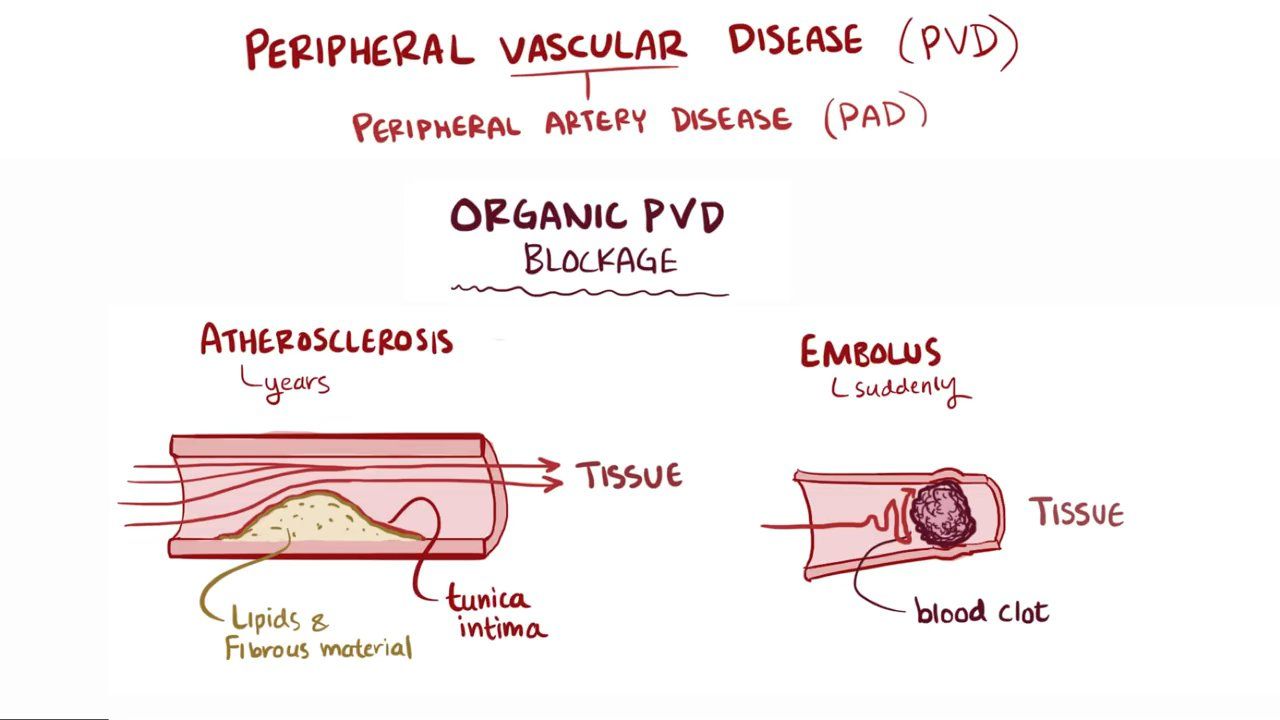
Peripheral vascular disease (PVD) is also known as ‘peripheral artery disease’ (PAD). It usually refers to narrowing of the arteries leading to your legs and feet.
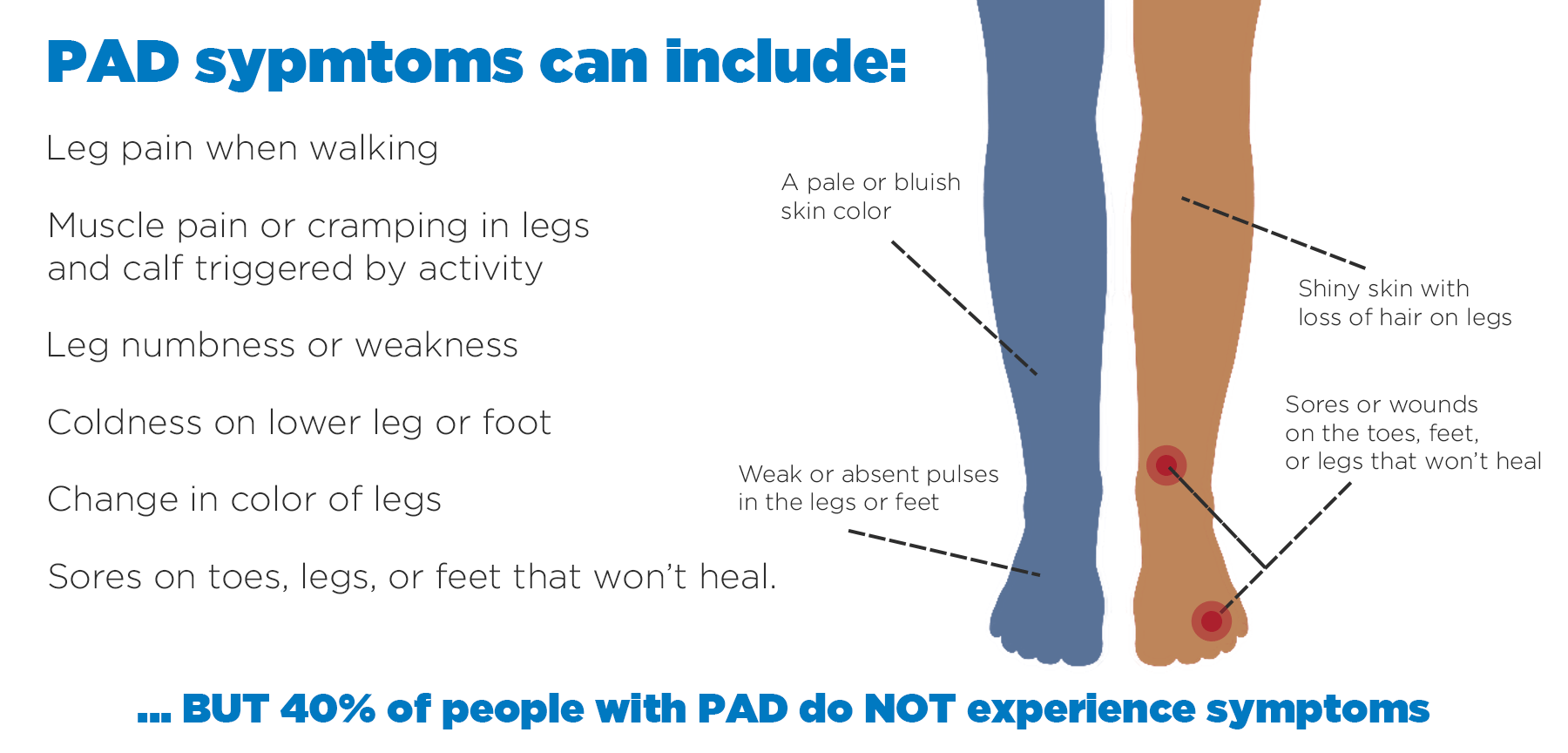
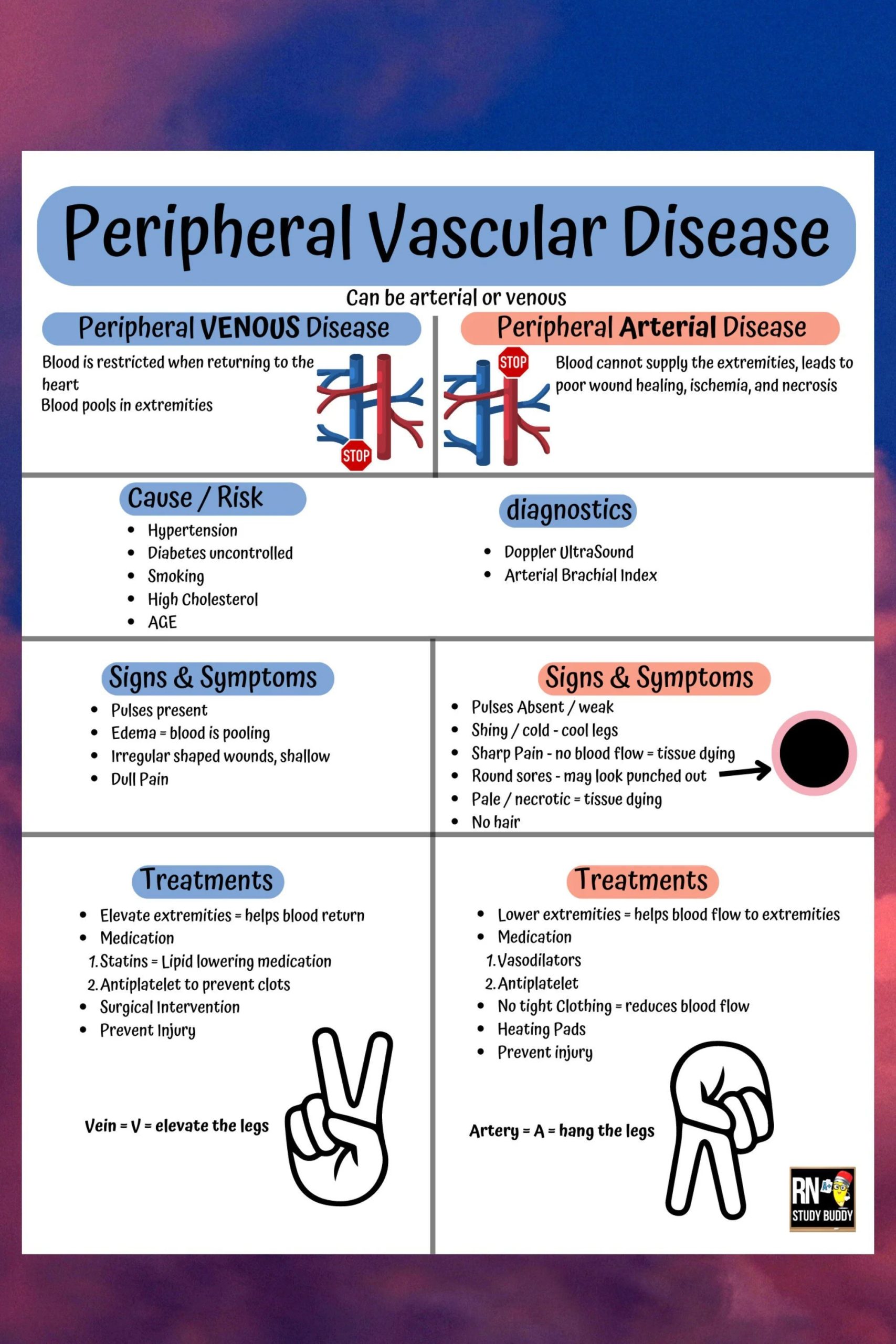
What are the symptoms of peripheral vascular disease?
The most common symptom of PVD is painful cramping in your leg muscles. This is triggered by physical activity, such as walking or climbing stairs.
The pain usually develops in your calves (lower leg). Sometimes your thigh or buttock muscles can be affected. It can range from mild to severe.
The pain will usually go away after 5 to 10 minutes when you rest your legs. This pattern of symptoms is known as ‘intermittent claudication’. (Claudication is a Latin term that loosely translates as ‘limping’.)
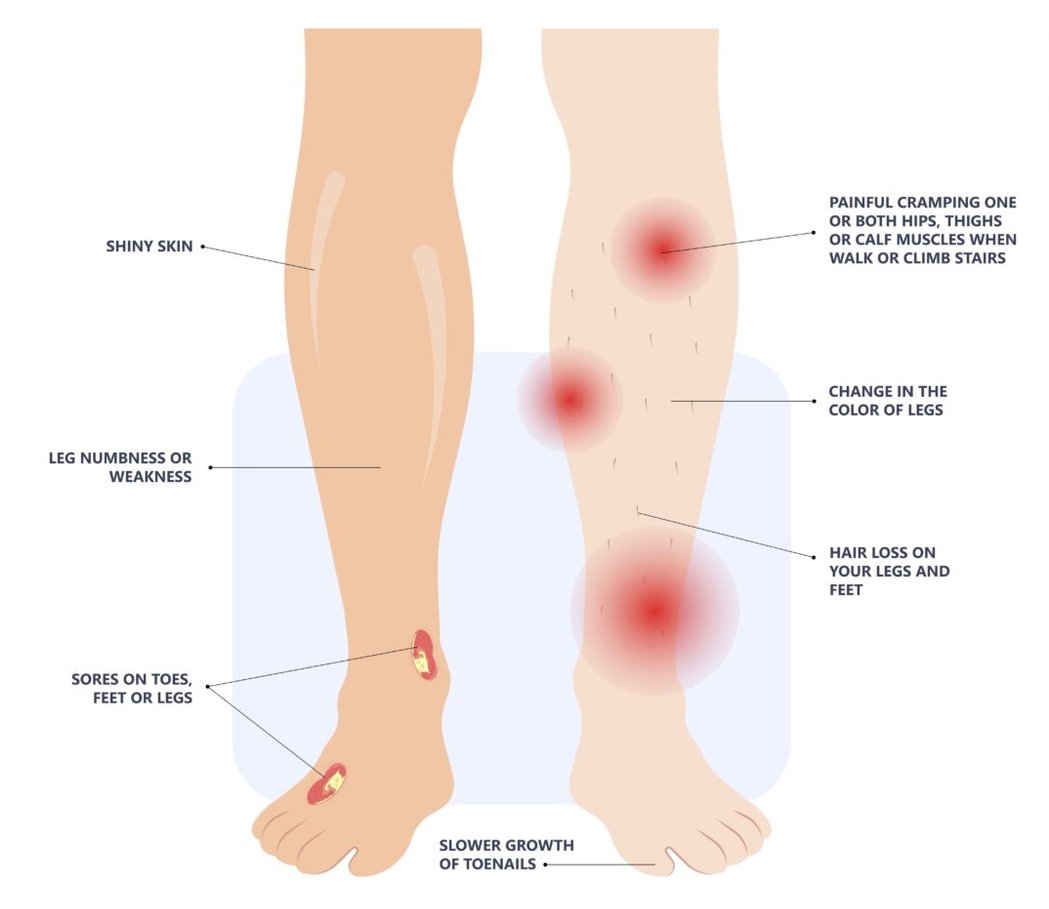
Other signs of PVD may include the following:
- Coldness in your lower legs or feet.
- Changing skin colour on your legs, turning pale when raised and then red when sitting.
If the blockage is more serious, you may have pain in your legs when resting. The pain may be severe and burning. It often happens at night or when your feet are elevated. The pain may get better if you dangle your legs over the edge of your bed.
You may also have:
- hair loss on your legs and feet
- shiny, pale, dry skin on your legs
- bluish coloured feet
- brittle, slow-growing toenails
- numbness or weakness in your legs
- wasting of the muscles in your legs
- wounds and ulcers (open sores) on your feet and legs, which don’t heal
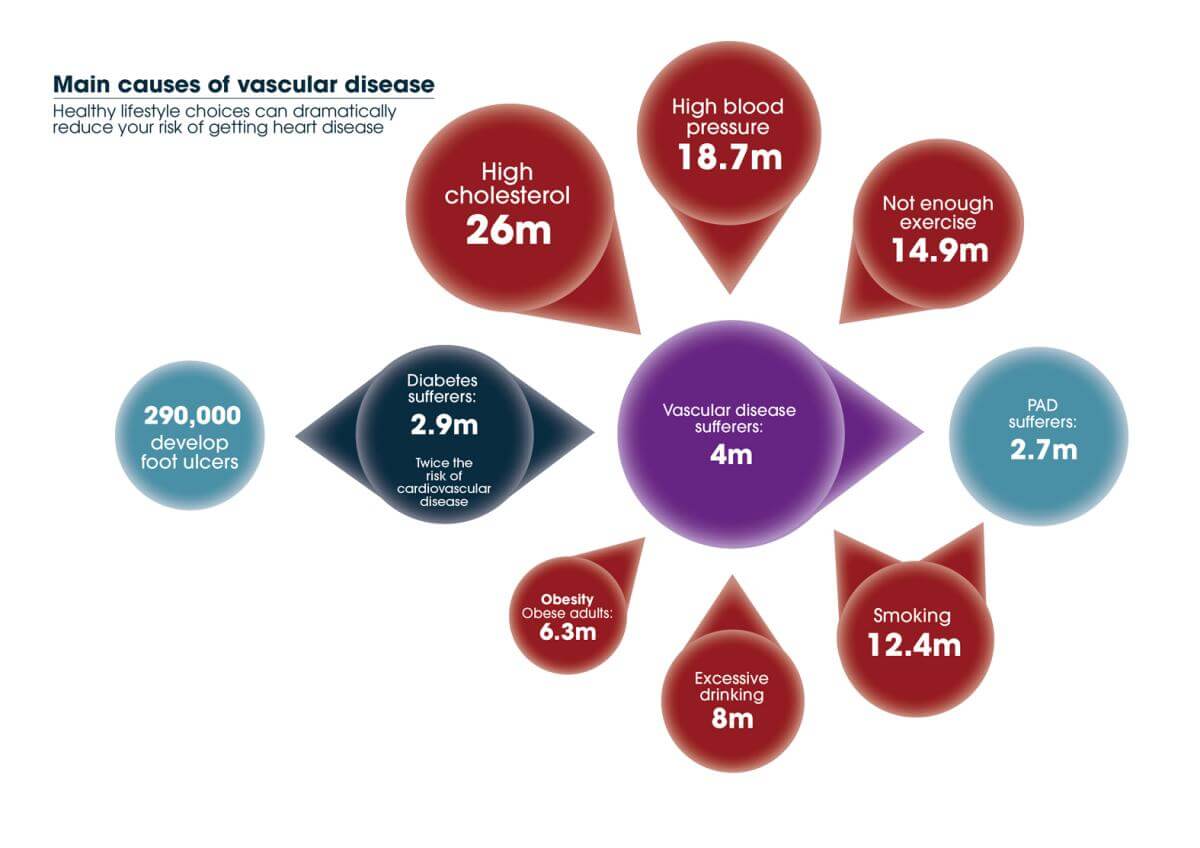
What causes peripheral vascular disease?
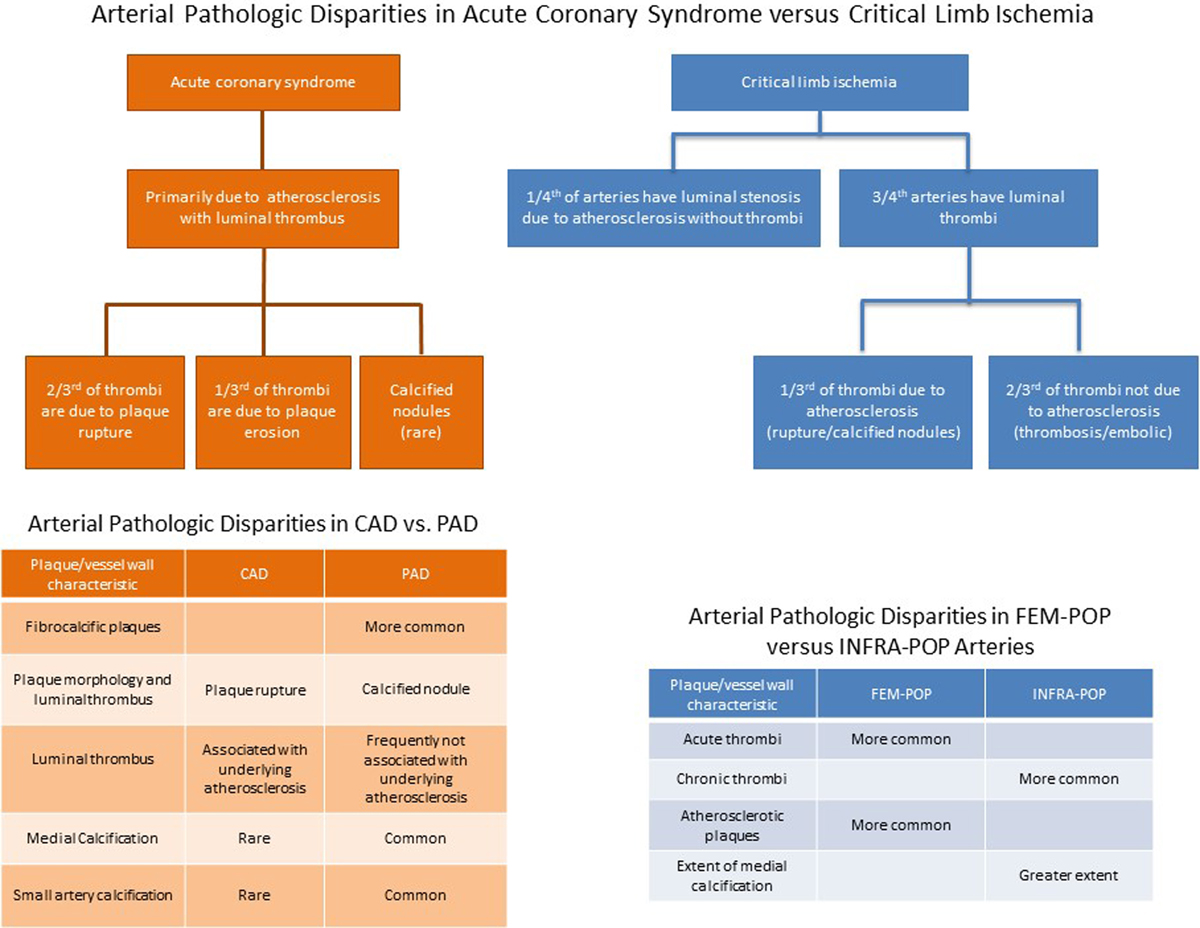
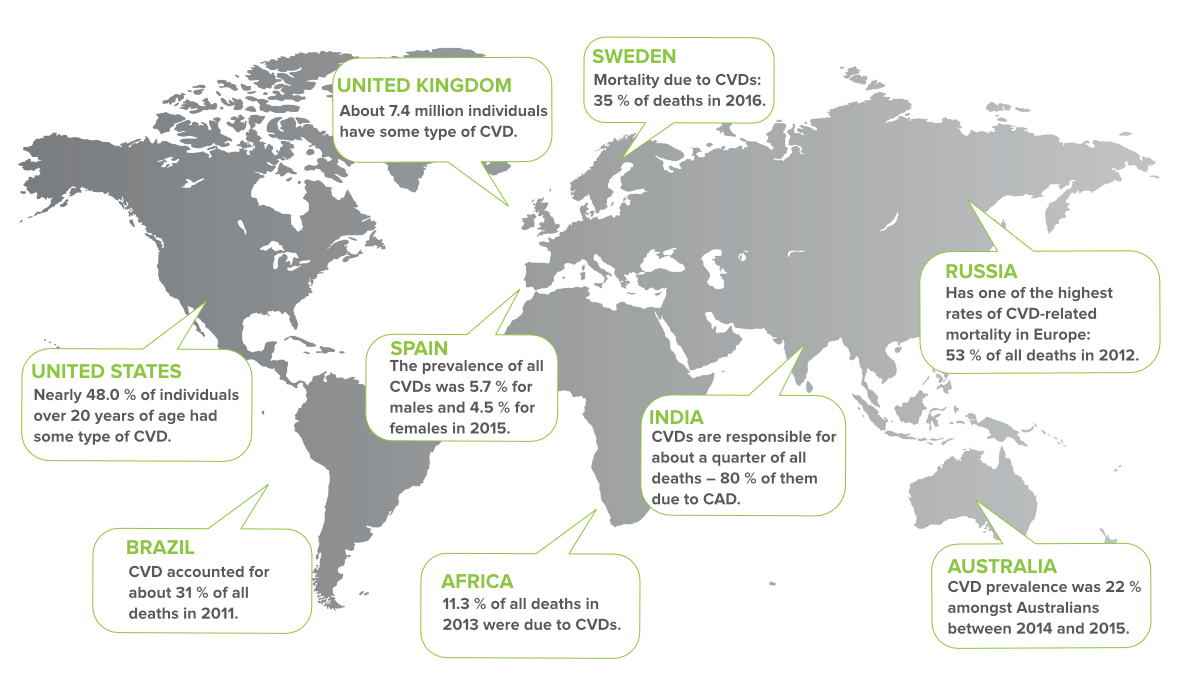
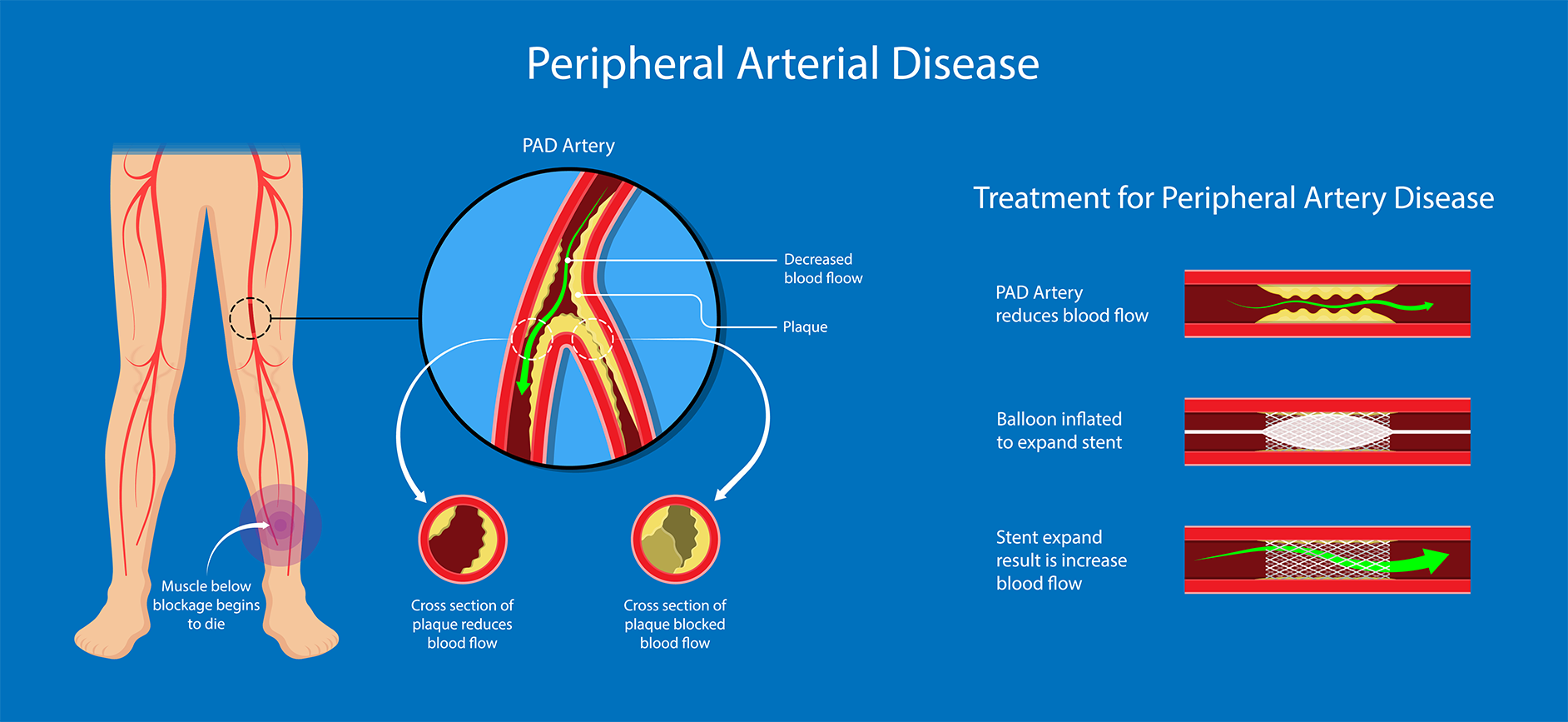
PVD is caused by a build-up of atheroma (fatty deposits on the walls of your arteries). This makes the arteries narrower. It restricts the flow of blood to the part of the body affected. This process is called ‘atherosclerosis’.
There are many factors that can contribute to the narrowing of your arteries. These include:
- smoking
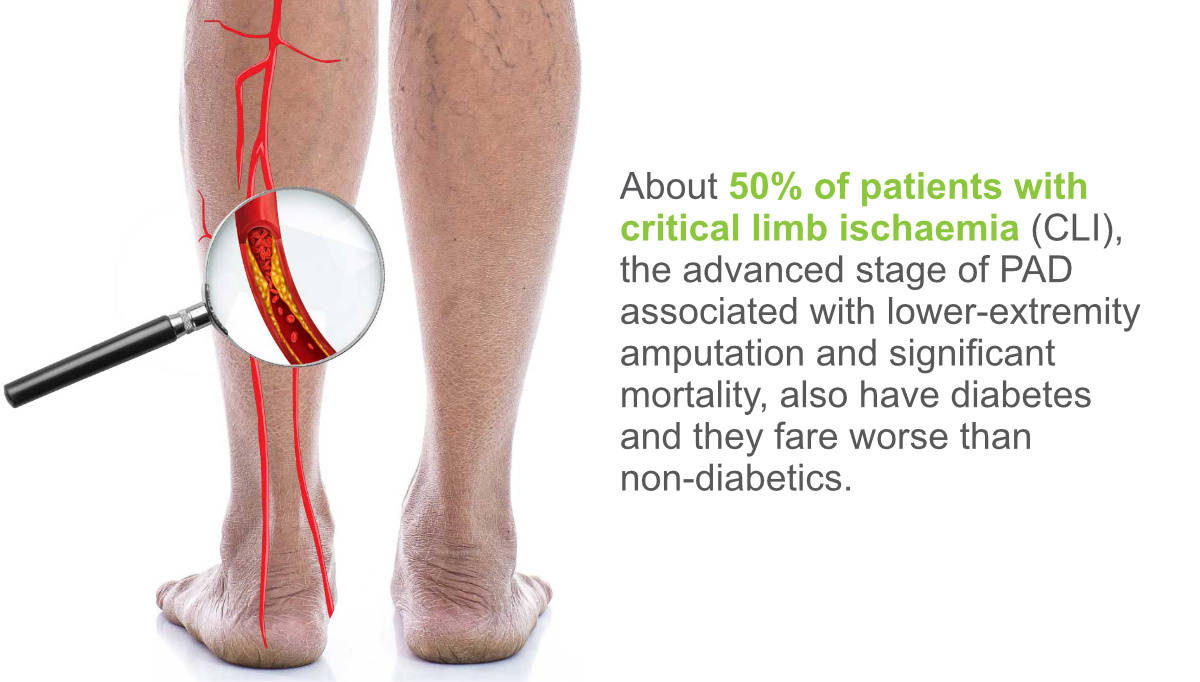
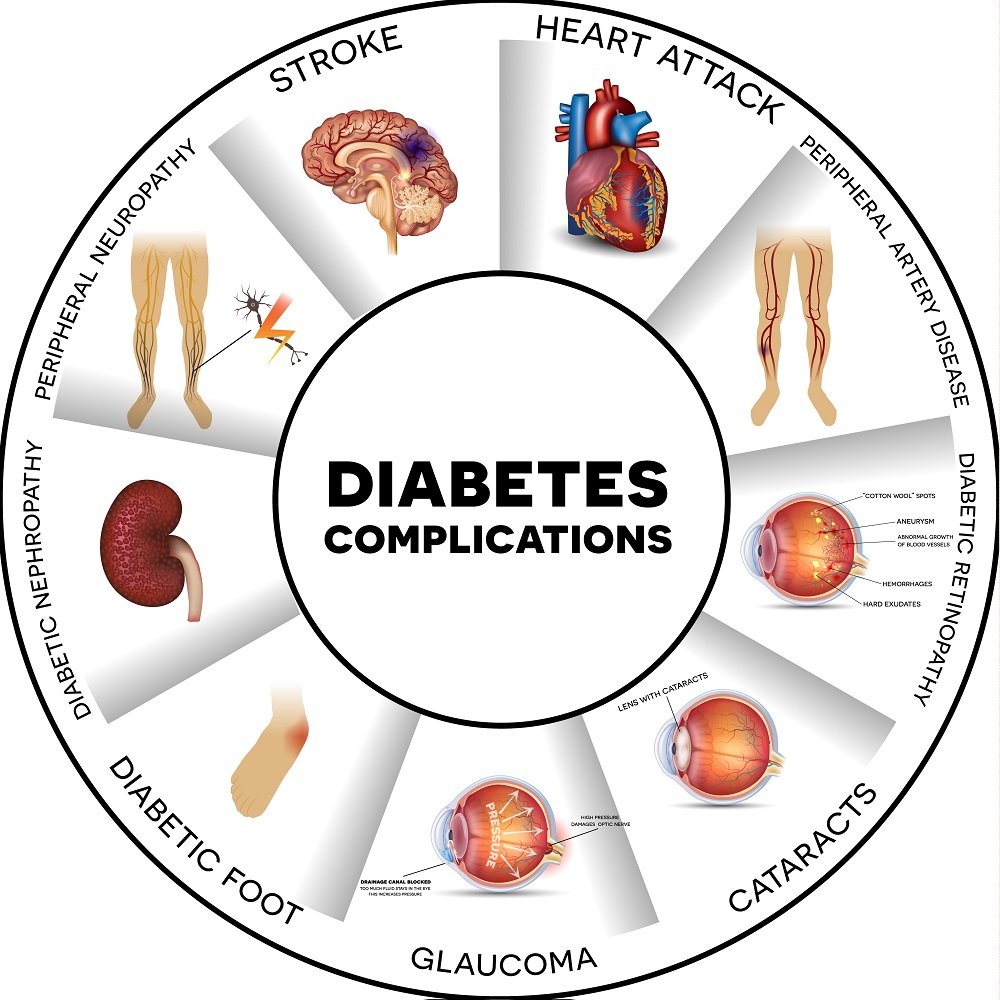
- having poorly controlled diabetes
- eating a high-fat diet
- having high cholesterol
- high blood pressure
- increasing age
If you have PVD, you also have a greater risk of coronary heart disease and stroke.
When should I see my doctor?
Many people mistakenly think that recurring episodes of leg pain are part of growing older. But this is not true. There is no reason why a healthy person should experience leg pain.
If you do have episodes of leg pain, that comes on when walking and gets better when you rest, see your doctor.
When should I get urgent medical advice?
Some symptoms suggest that the supply of blood to your legs has become severely restricted and you may need to see a doctor urgently. These include:
- sudden onset of foot pain, paleness or coldness over hours or days
- being unable to move the muscles in your affected leg
- numbness in your affected leg
- having your toes suddenly turn blue
How is peripheral vascular disease diagnosed?
Your doctor will ask about your symptoms and examine your legs. They will feel for pulses in your legs as part of the examination.
Your doctor may compare the blood pressure in your legs to the blood pressure in your arms by using a test called the ankle brachial index (ABI).
They may also recommend some tests. These may include:
- an ultrasound scan to look at the blood flow in your legs
- an angiogram (where dye is injected into your blood vessels so the doctor can watch your blood flow using various imaging techniques)
- blood tests
Your doctor may also refer you to a specialist.
How is peripheral vascular disease treated?
Lifestyle changes
Making lifestyle changes can improve symptoms. They can also reduce your risk of developing coronary heart disease and stroke.
Recommended lifestyle and self-care measures include:
- quitting smoking
- eating a healthy diet
- losing weight if you are overweight
- regular foot care and foot check-ups, especially if you also have diabetes
- exercise programs to improve your walking distance
Walking exercise programs help to reduce the severity and frequency of your PVD symptoms.
At the same time, exercise can reduce your risk of heart disease. Ask your doctor about the best way to exercise.
Medicines
Taking medicines can address the underlying cause of PVD and reduce your risk of developing cardiovascular disease. Your doctor may recommend you take:
- a statin medicine to lower your cholesterol levels
- medicine to treat high blood pressure
- low-dose aspirin and/or a similar medicine to prevent blood clots
- medicines to control your blood sugar levels if you have diabetes
Surgery
One possible procedure is angioplasty and stenting to unblock your artery and keep it open.
Surgery may be recommended as a last resort in severe cases.
This may involve a bypass graft if the blood flow in your leg is blocked
Can peripheral vascular disease be prevented?
If you smoke, you should quit. This will reduce your risk of PVD.
You can also help to prevent PVD by making sure your diabetes is controlled and keeping your blood pressure and blood cholesterol at healthy levels.
Make healthy food choices and exercise regularly, for at least 30 minutes on most days of the week.
If you are overweight, losing even a small about of weight will help to reduce your risk of PVD.
Complications of peripheral vascular disease and related problems
Severe cases of PVD can lead to ‘chronic limb ischemia’ (lacking blood supply). This is when blood flow to your limb is severely restricted. It is very serious.
Males with PVD may develop impotence (erectile dysfunction). They may have difficulty being able to obtain or keep an erection.