Key facts
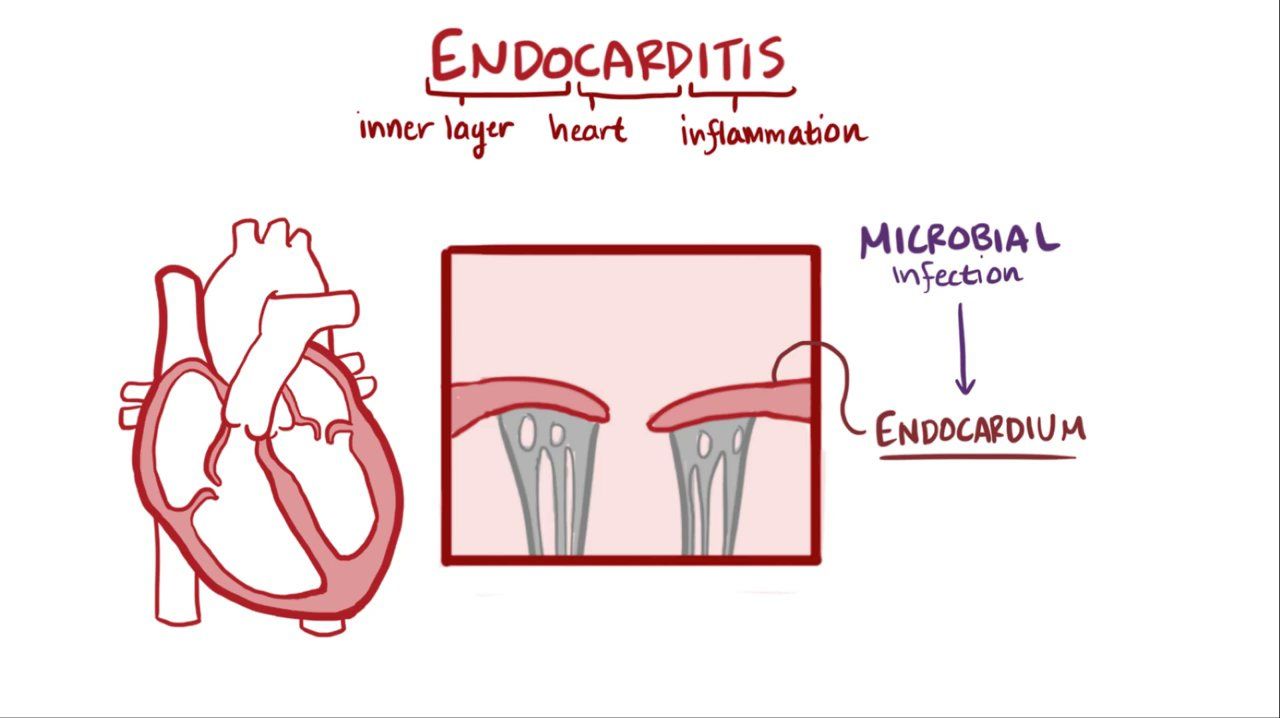
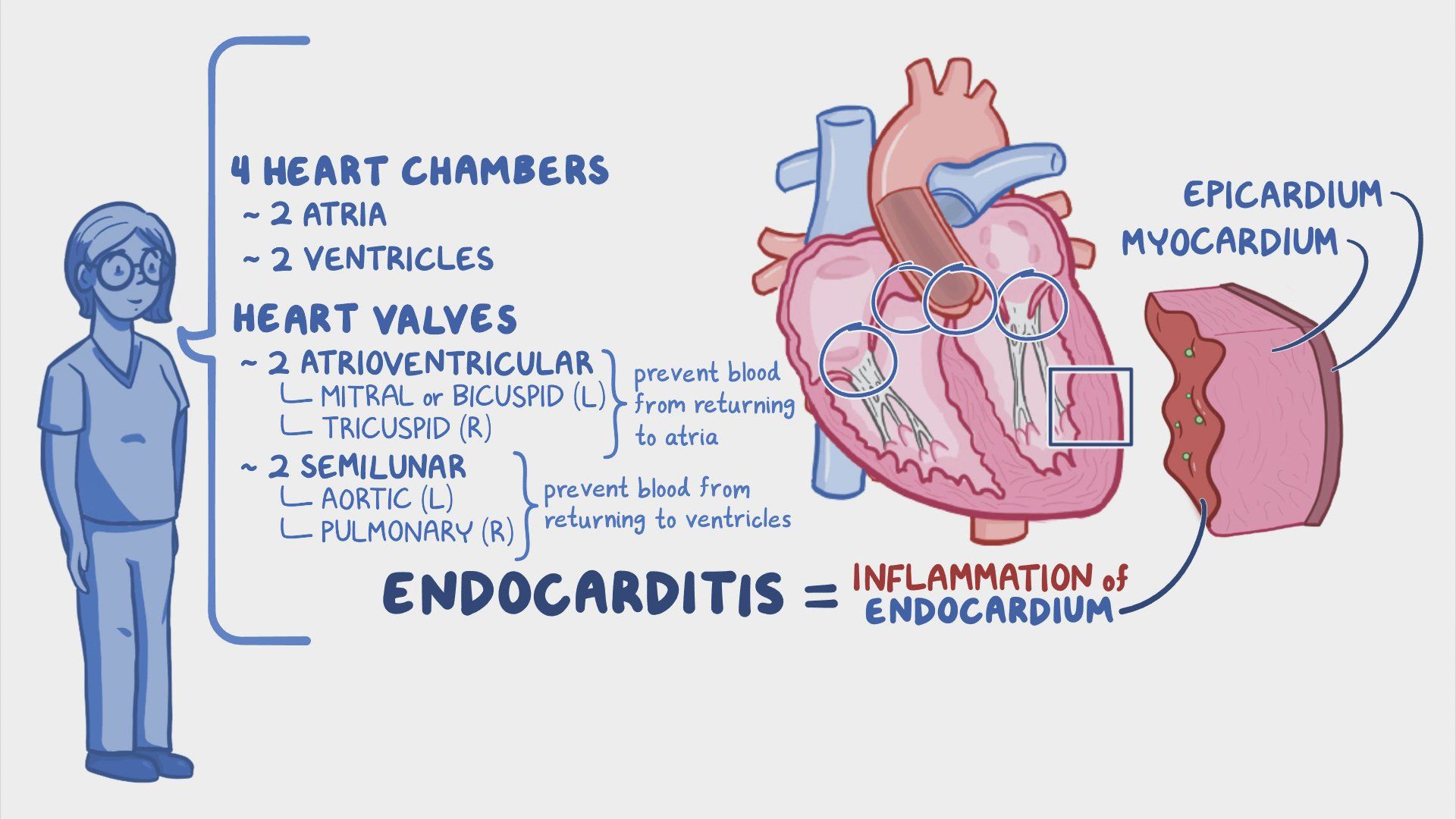
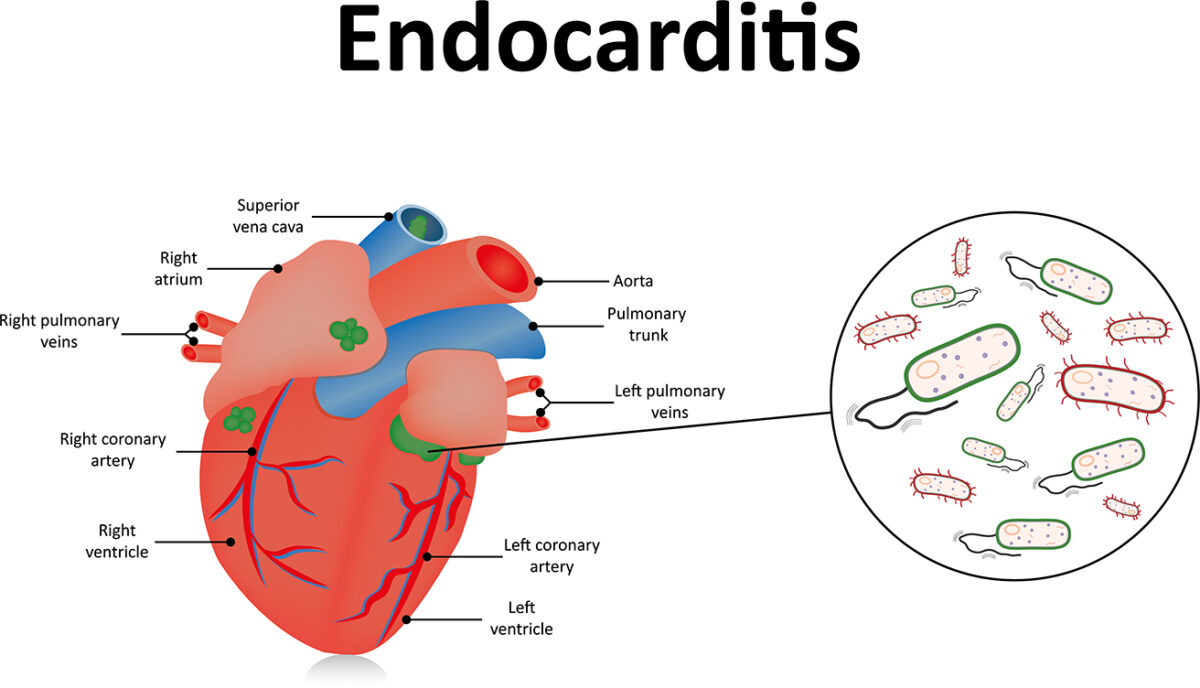
- Endocarditis is a rare but serious condition caused by an infection of the inner lining of your heart.
- It usually involves one or more of your heart valves.
- Symptoms can develop over a few days or several weeks, and may include fever, night sweats, tiredness, weight loss and general aches and pains.
- The main treatment is antibiotics but many people with endocarditis also need surgery to remove infected tissue and to rebuild or replace damaged heart valves.
- If you are at risk of endocarditis you should see your doctor.
What is endocarditis?
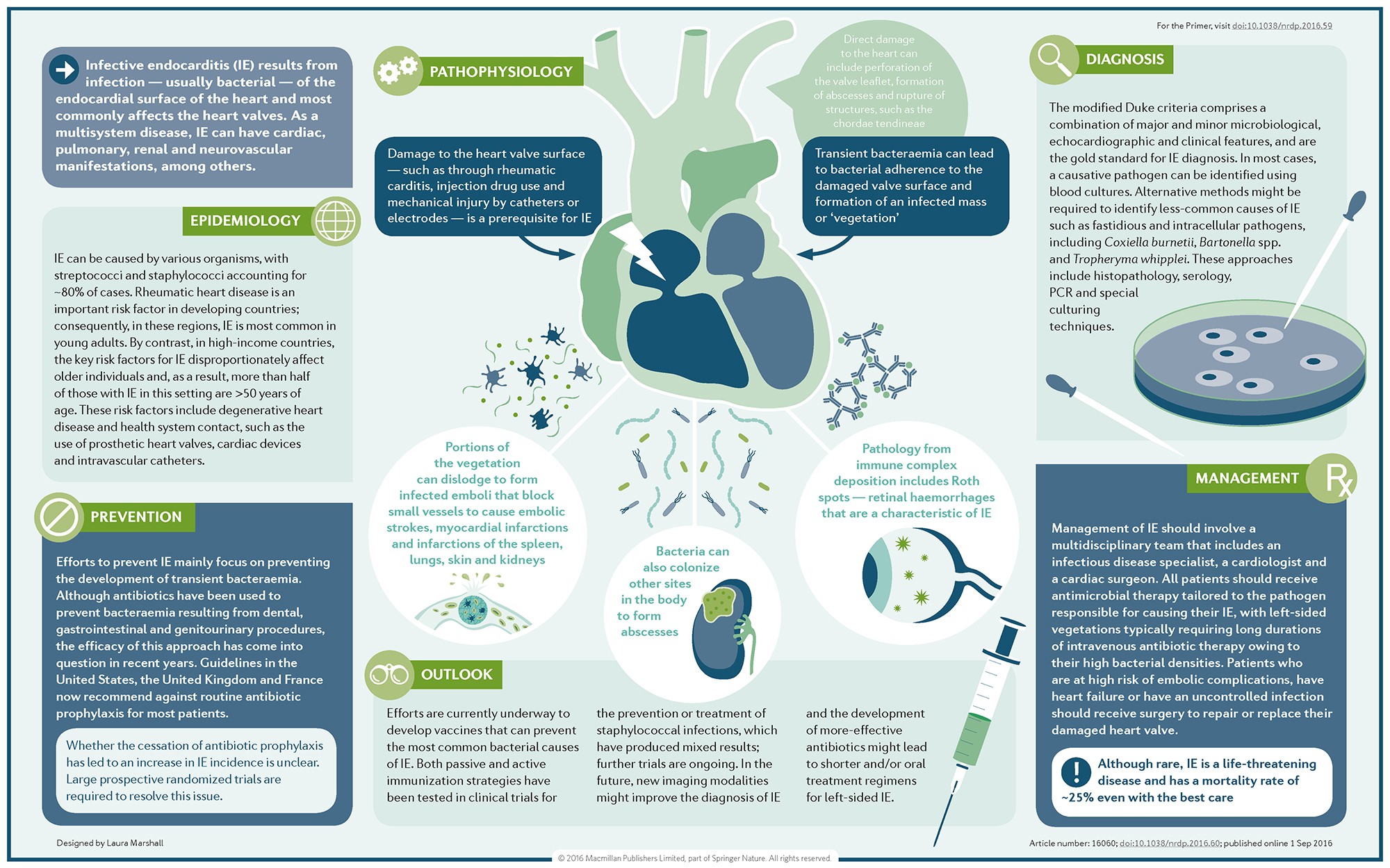
Endocarditis is a rare but serious condition caused by infection of the inner lining of your heart. It usually involves one or more of your heart valves. It is also called ‘infective endocarditis’ or ‘bacterial endocarditis’.
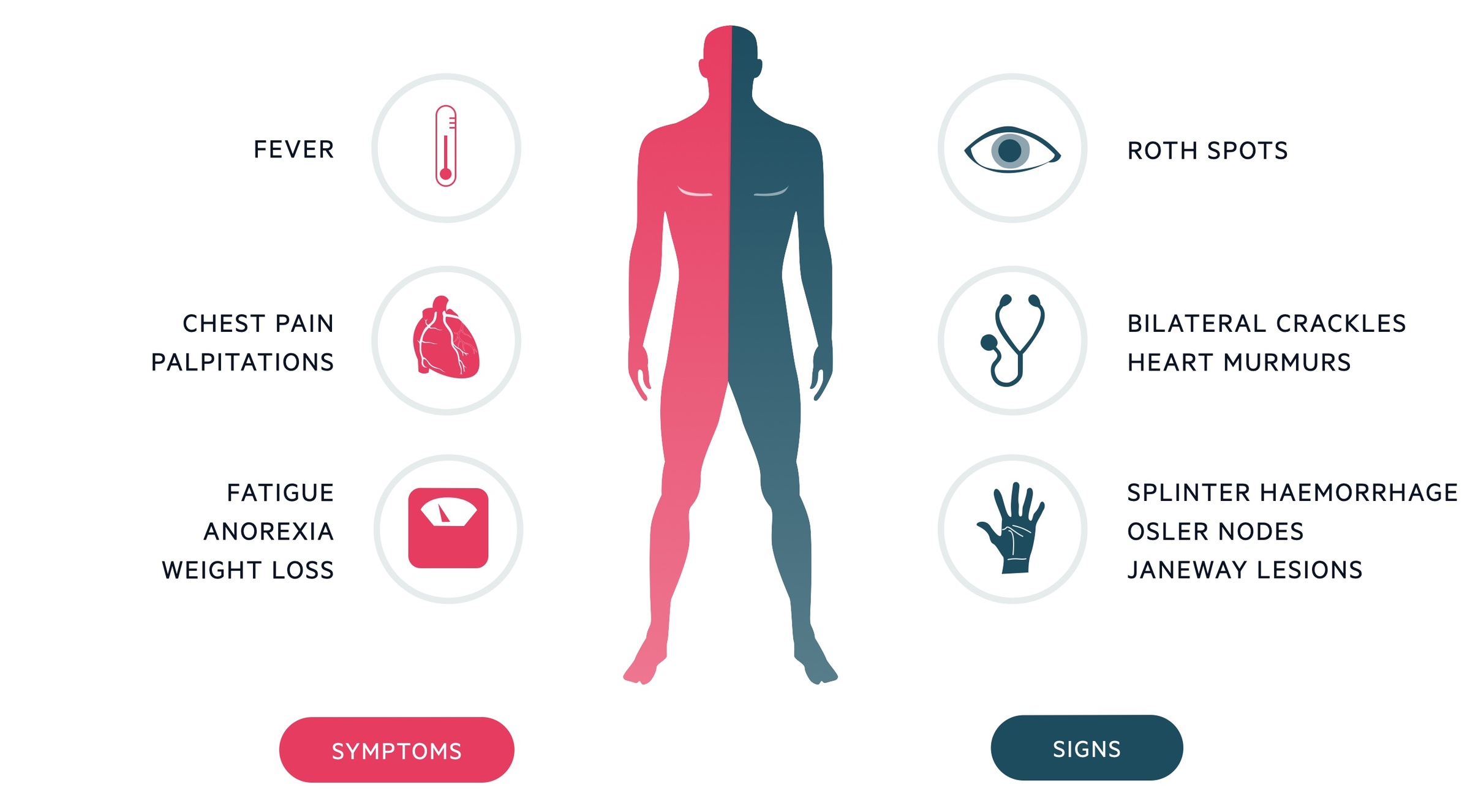
What are the symptoms of endocarditis?
Endocarditis symptoms can develop over a few days or several weeks. Symptoms can include:
- a high temperature (fever), chills and night sweats
- muscle aches and pains
- shortness of breath
- headaches
- chest pain
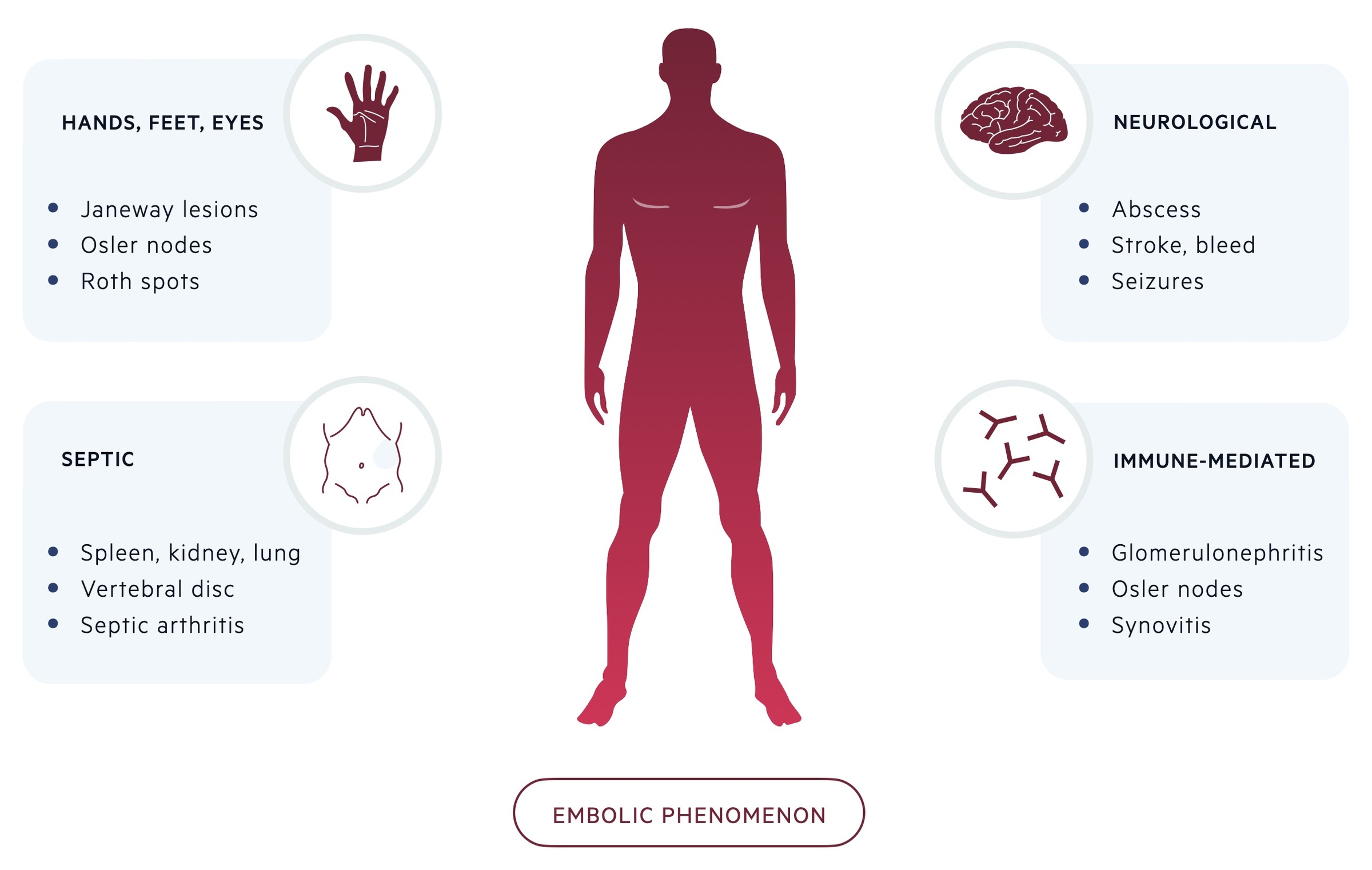
- red or brown marks under your fingernails or toenails
- painless red spots on the palms or soles of your feet
- painful lumps on your fingertips or toes
- extreme tiredness and weight loss
- swelling in the feet or ankles
If you develop any of these symptoms, especially if you are at risk of endocarditis, you should see your doctor as soon as possible.
Although many of the symptoms also have other causes, endocarditis must be diagnosed and treated rapidly.
What causes endocarditis?
Endocarditis is usually caused by a bacterial infection. It can sometimes be caused by a fungal infection. Bacteria can reach your heart:
- through your mouth after a dental procedure or after regular brushing and flossing
- after surgery or other medical procedures
- through your skin, digestive system or urinary tract
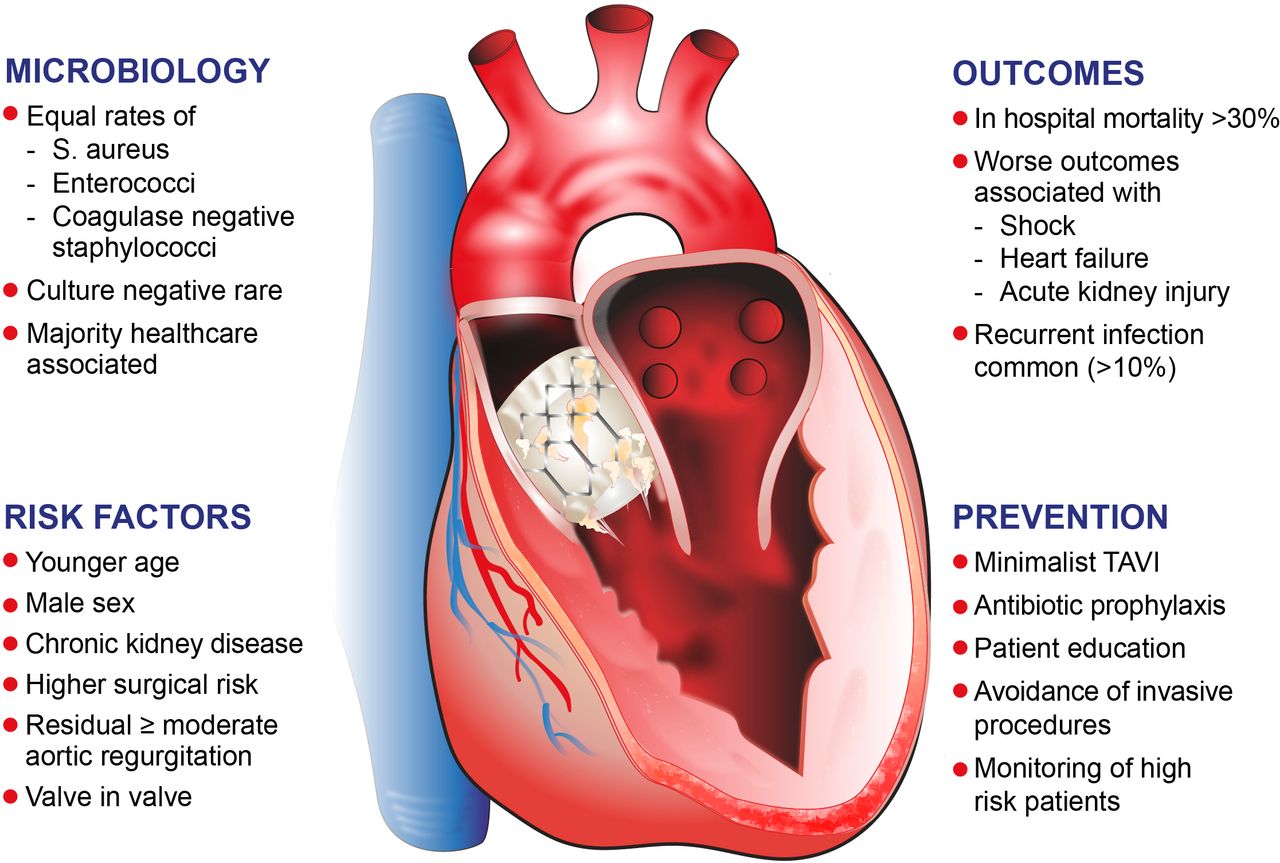
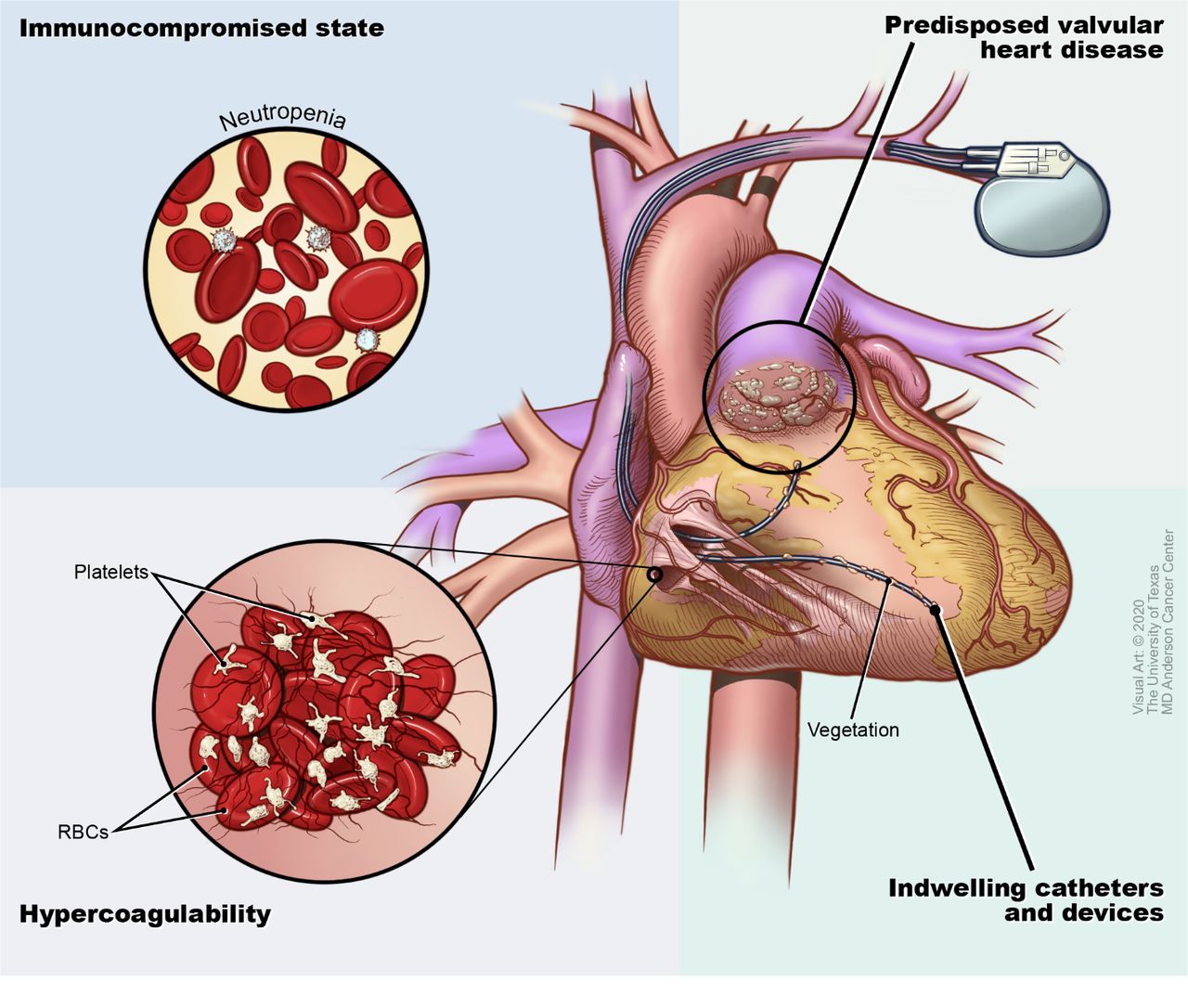
What can increase your risk of endocarditis?
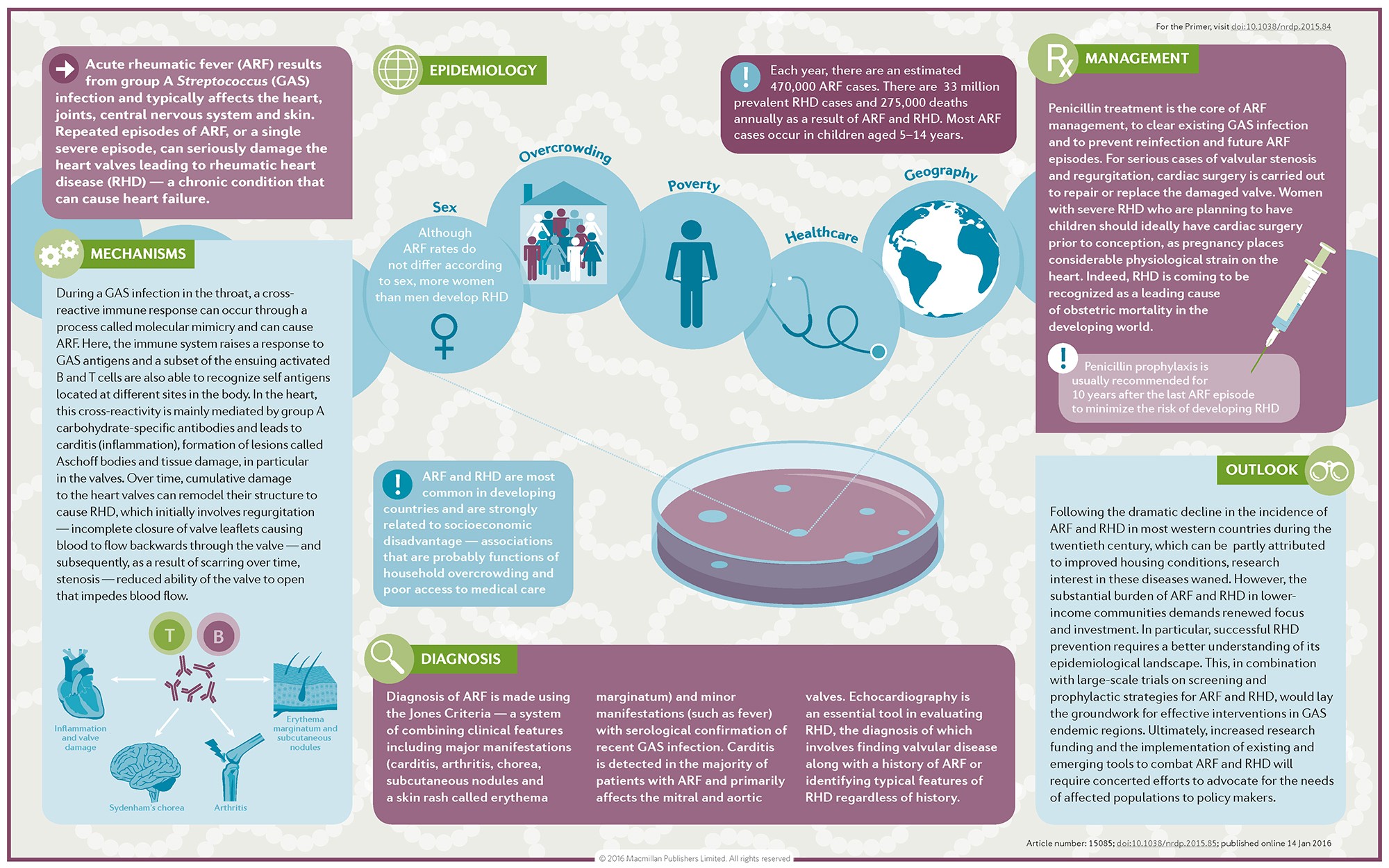
Bacteria in your bloodstream are more likely to infect a heart that already has some damage. This damage might have been present at birth (congenital) or caused by disease.
Heart conditions that can increase your risk of endocarditis include:
- previously having endocarditis
- having an artificial heart valve
- having certain types of congenital heart disease
- having had a heart transplant
- having an implanted heart device such as a pacemaker or an implantable cardioverter-defibrillator
- having heart valve disease
- having certain types of cardiomyopathy
Your risk of endocarditis is also increased if you are more likely to have a bloodstream infection, such as from:
- having an intravascular catheter (for example, for dialysis)
- intravenous drug use (injecting drugs)
- having an underactive immune system
When should I see my doctor?
See your doctor as soon as possible or go to the nearest hospital emergency department if you develop symptoms of endocarditis.
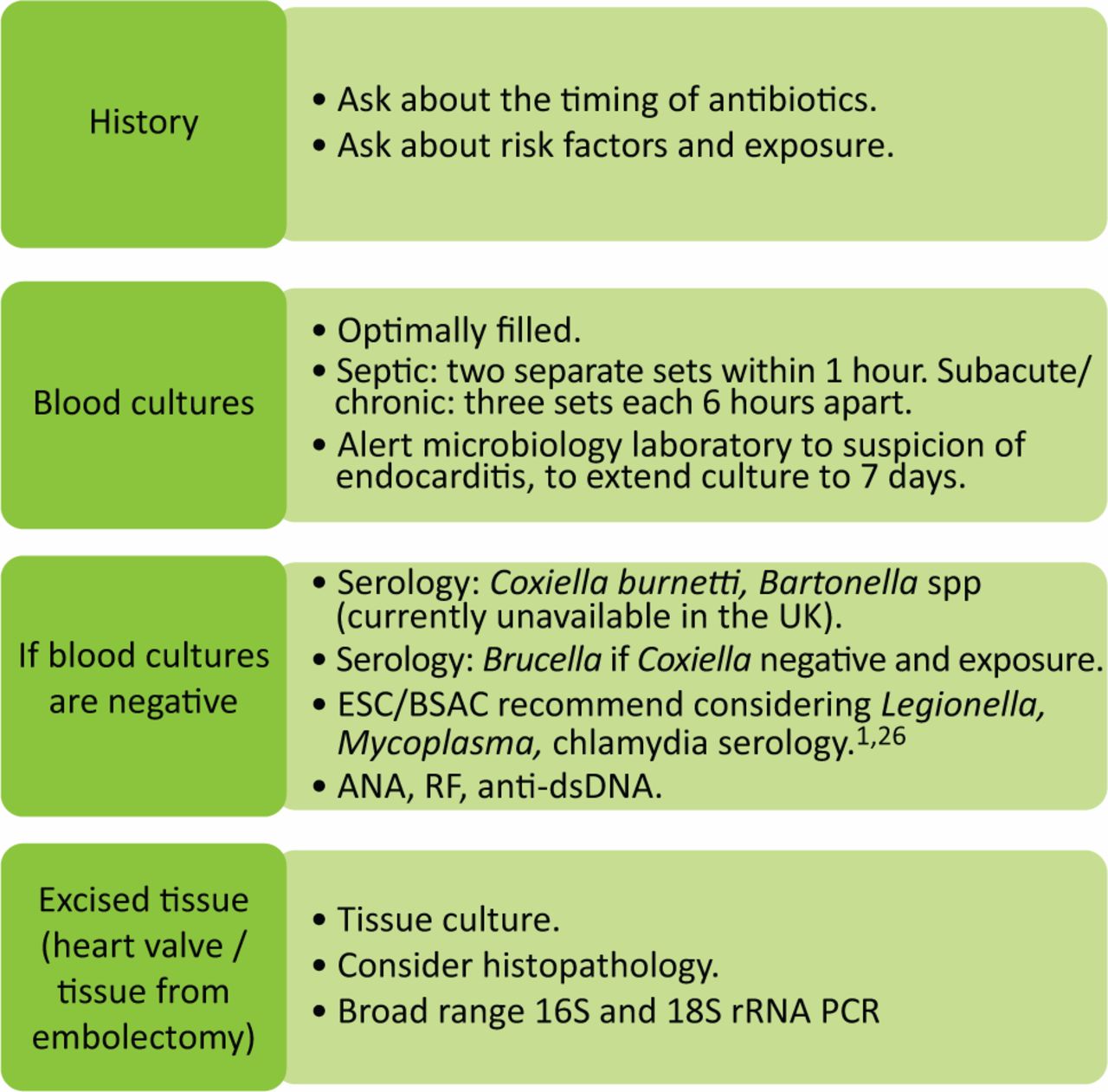
How is endocarditis diagnosed?
Your doctor will ask about your symptoms and medical history. They will also examine you. Part of the examination will be listening to your heart for new or changing heart murmurs.
Tests that may be recommended include:
- an electrocardiogram (ECG) to see how well your heart is working
- multiple blood tests to check on the health of your organs and to look for infection
- a chest x-ray
- an echocardiogram, which is an ultrasound of your heart
- a urine (wee) test
You might also have other imaging tests such as an MRI scan or a PET scan.
How is endocarditis treated?
Endocarditis is a serious and complex condition. If diagnosed, you will need to be treated in hospital, at least initially. You might need treatment in an intensive care unit.
You might see a range of doctors, including:
- a cardiologist (heart doctor)
- a microbiologist (someone who studies microscopic organisms that cause infection)
- an infectious diseases specialist
- a heart surgeon
Antibiotics
The main treatment for endocarditis is antibiotics. This will initially be through an intravenous (IV) drip into a vein.
People with fungal infections need treatment with antifungal therapy.
Surgery
You may need surgery to remove infected tissue and to rebuild or replace your damaged heart valves.
Monitoring
You will need to have repeated blood tests, x-rays and other imaging tests to monitor your progress.
Endocarditis can come back, so your health will be monitored closely for the next year or so. You’ll learn how to reduce your chance of reinfection and how to recognise if it occurs.
Can endocarditis be prevented?
If you are at risk of endocarditis, you should talk with your doctor to learn more about prevention.
Measures to help prevent endocarditis in people at risk include:
- good dental hygiene to reduce your risk of bacteria entering through your mouth
- regular dental check-ups
- getting advice from your doctor before having any non-medical procedures, such as body piercing or tattoos
If you are at risk of endocarditis, antibiotics may be recommended before certain dental procedures. Talk to your doctor and dentist about the risks and benefits of taking antibiotics before dental work.
Complications of endocarditis
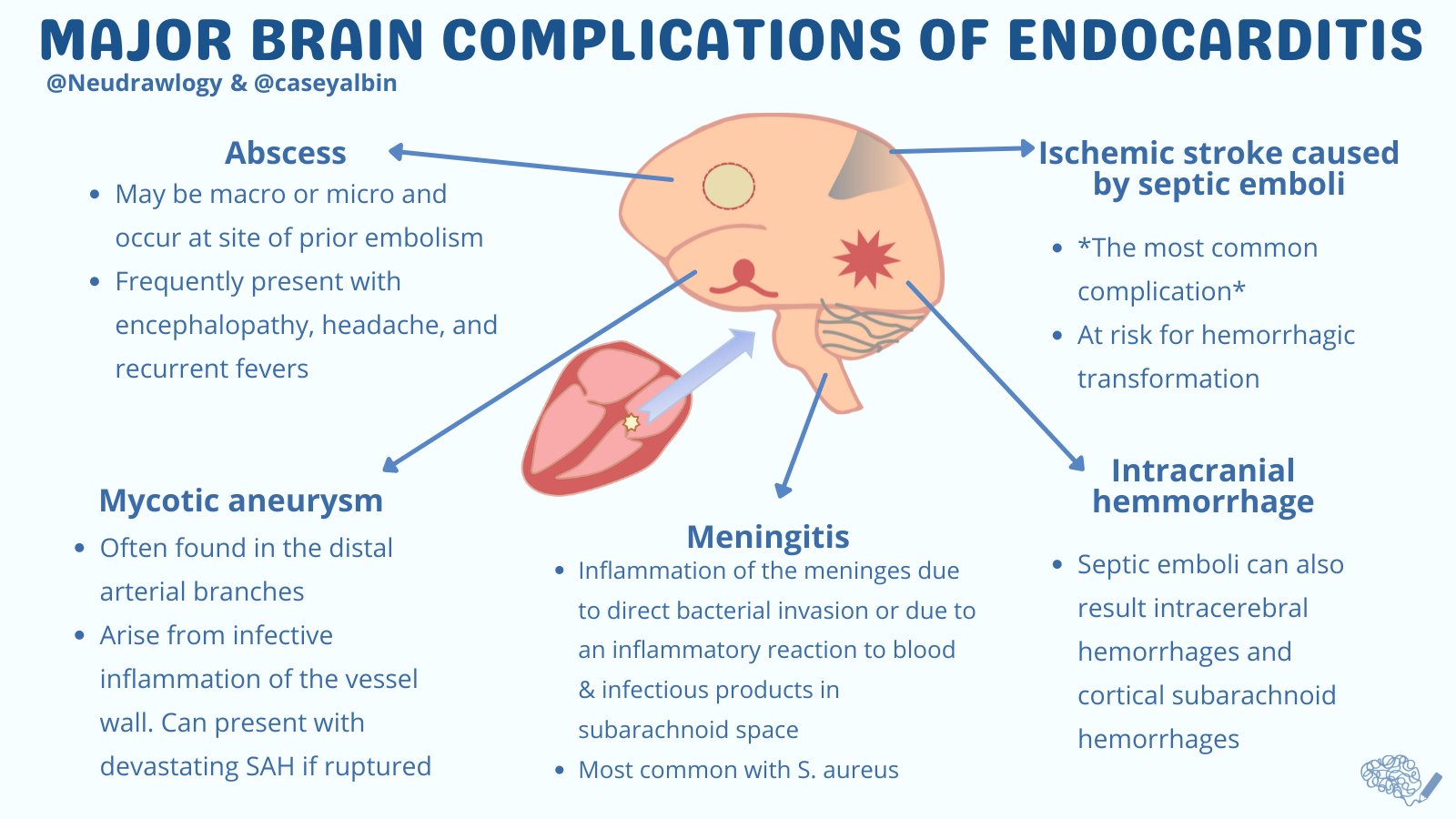
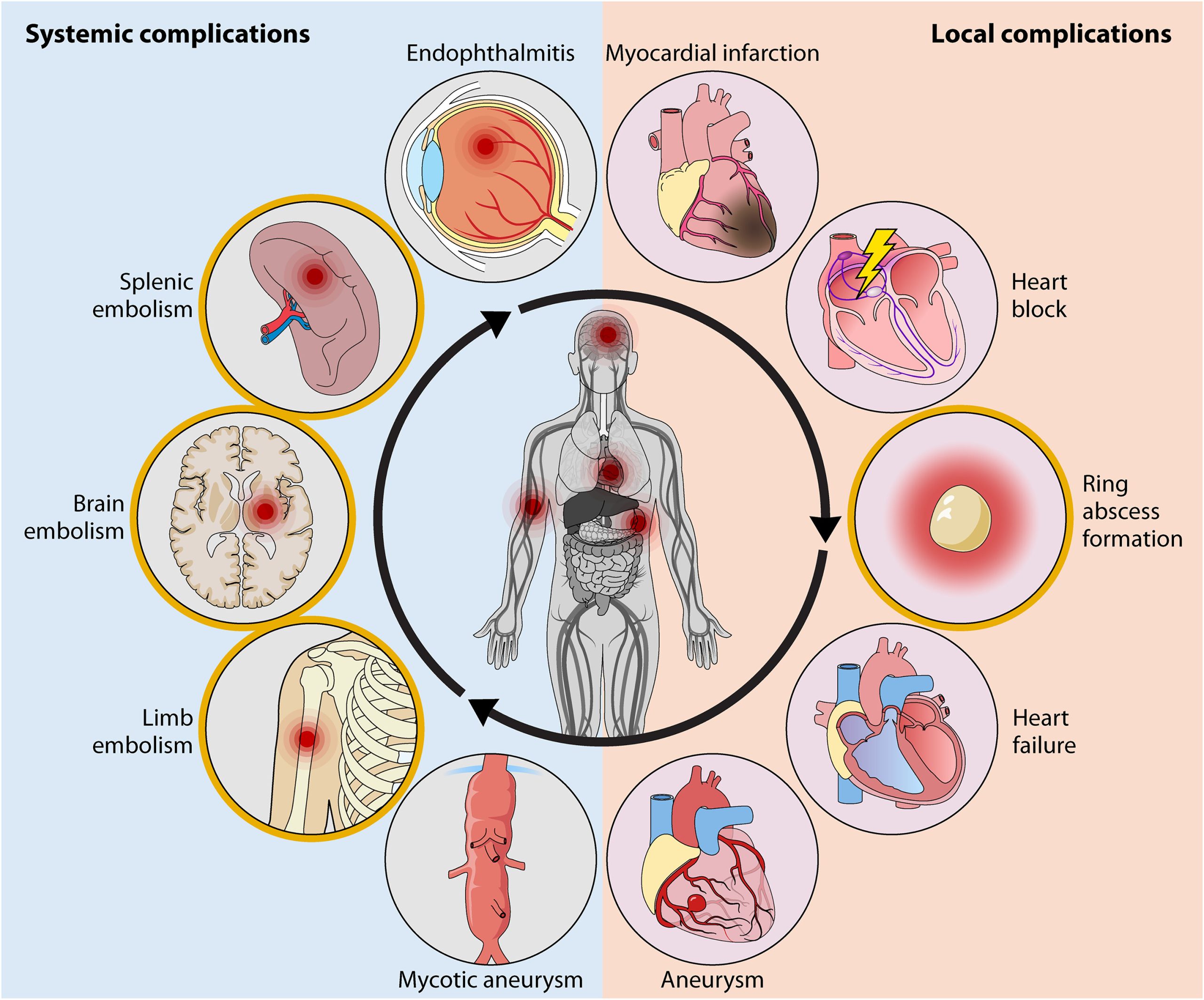
There are several possible complications associated with infective endocarditis. Some of these include:
- heart valve damage
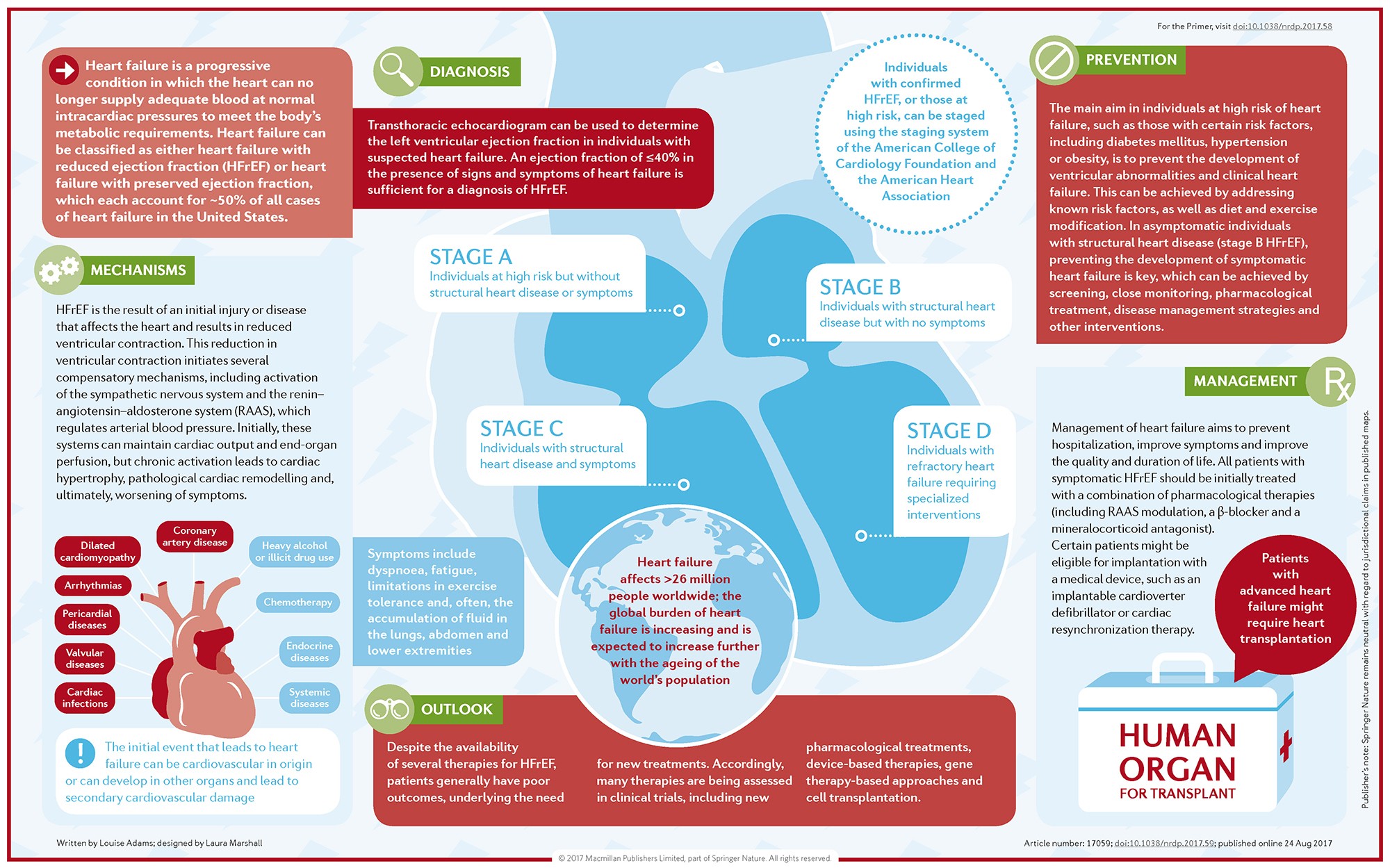
- heart failure
- kidney damage
- sepsis
- stroke