Kaposi’s sarcoma
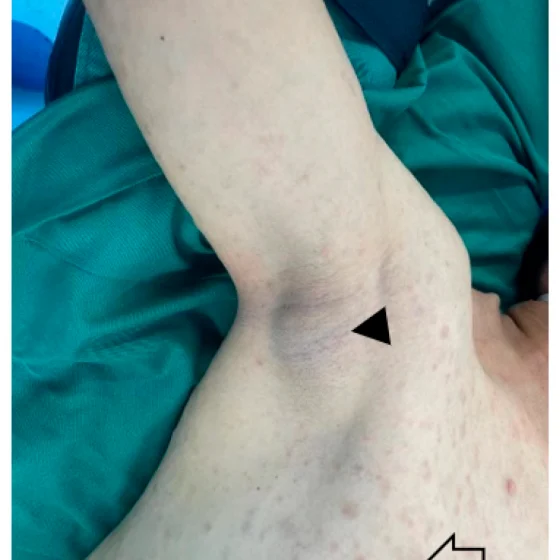
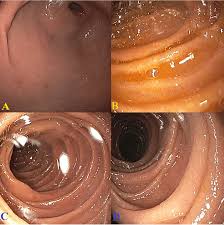
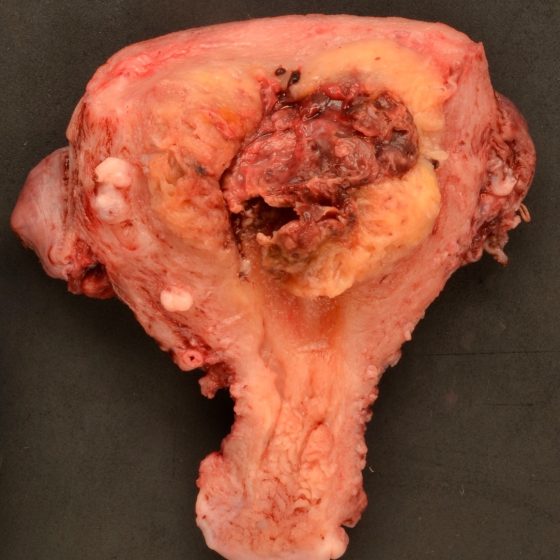
Kaposi’s sarcoma (KS) is a rare type of soft tissue sarcoma. A soft tissue sarcoma is a type of cancer. What is Kaposi’s sarcoma? Kaposi’s sarcoma (KS) develops from cells called endothelial cells, which line the blood and lymph vessels. It is most commonly found on the skin, but it can also affect the inside of the body, such as the lymph nodes, lungs, bowel, liver and spleen. KS growths are also called lesions or tumours. KS develops in a different way from other types of cancer. Most cancers begin in one place in the body and may then spread to