Vaginal Conditions
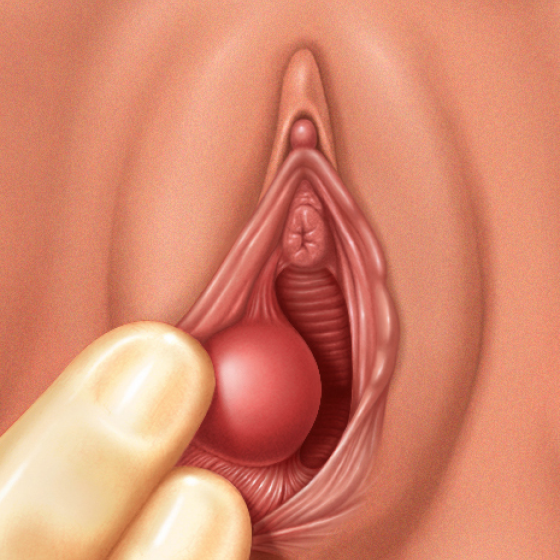
Bartholin’s abscess This is an abscess which forms on the Bartholin’s glands which line the vagina. – It arises when one of the ducts carrying fluid from the gland gets blocked, giving a fluid filled lump (cyst) – The cysts can then become infected by bacteria leading to the formation of a Bartholin’s abscess. Symptoms: – Vaginal pain and redness – Unilateral swelling near the vaginal introitus Diagnosis: Clinical Diagnosis Management: – 1st line is antibiotics. – If abscess does not respond/is painful, cyst drainage is performed (using word catheter or marsupialization) Vulval Carcinoma This describes a