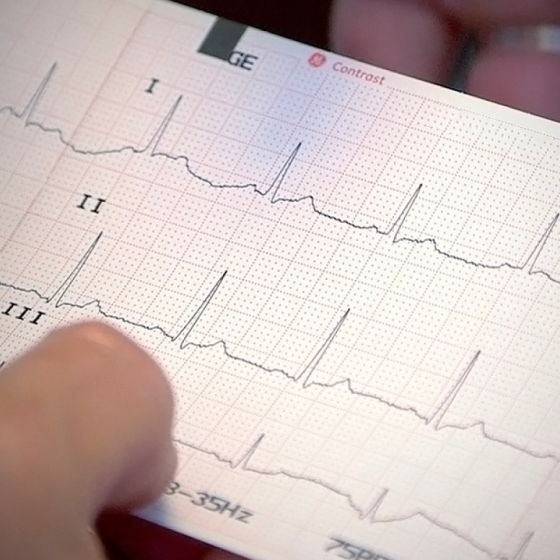
9. Reporting an ECG
Introduction It is important to have a good structure for analysing and subsequently reporting an ECG. When reporting an ECG, you should use the same structured approach every time. This is particularly important when first learning about ECGs. A structured approach allows you to systematically assess the ECG in order and not forget any key elements. Once you improve, you’ll start to develop pattern recognition for classic ECG features. We propose the following structure for analysing and reporting an ECG: Confirm correct patient details Rate Rhythm Cardiac axis P waves, Q waves & QRS complexes ST segments & T waves QT interval Putting it all together This