How will I know if my COVID-19 symptoms are mild, moderate or severe?
Mild symptoms
Adults
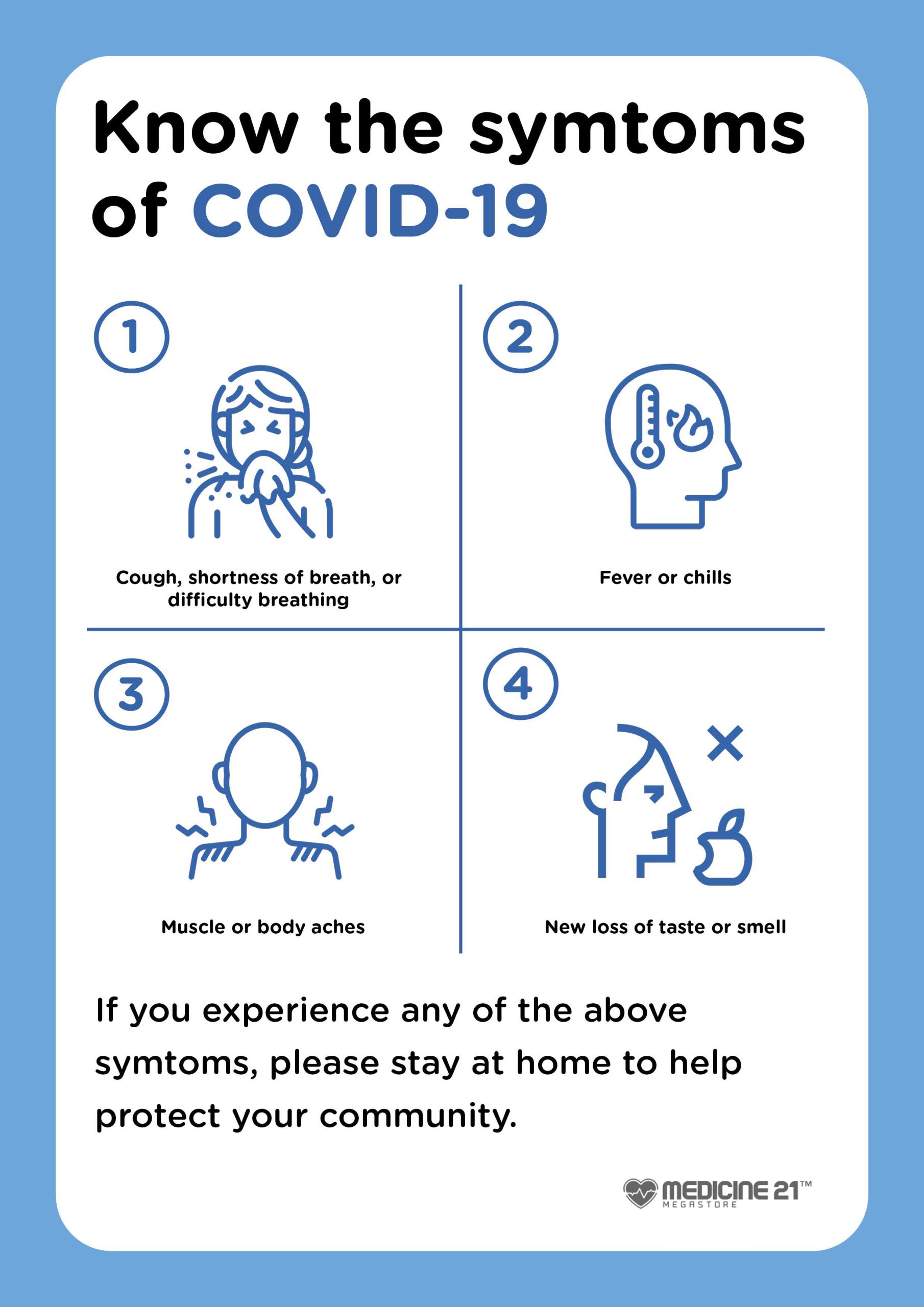
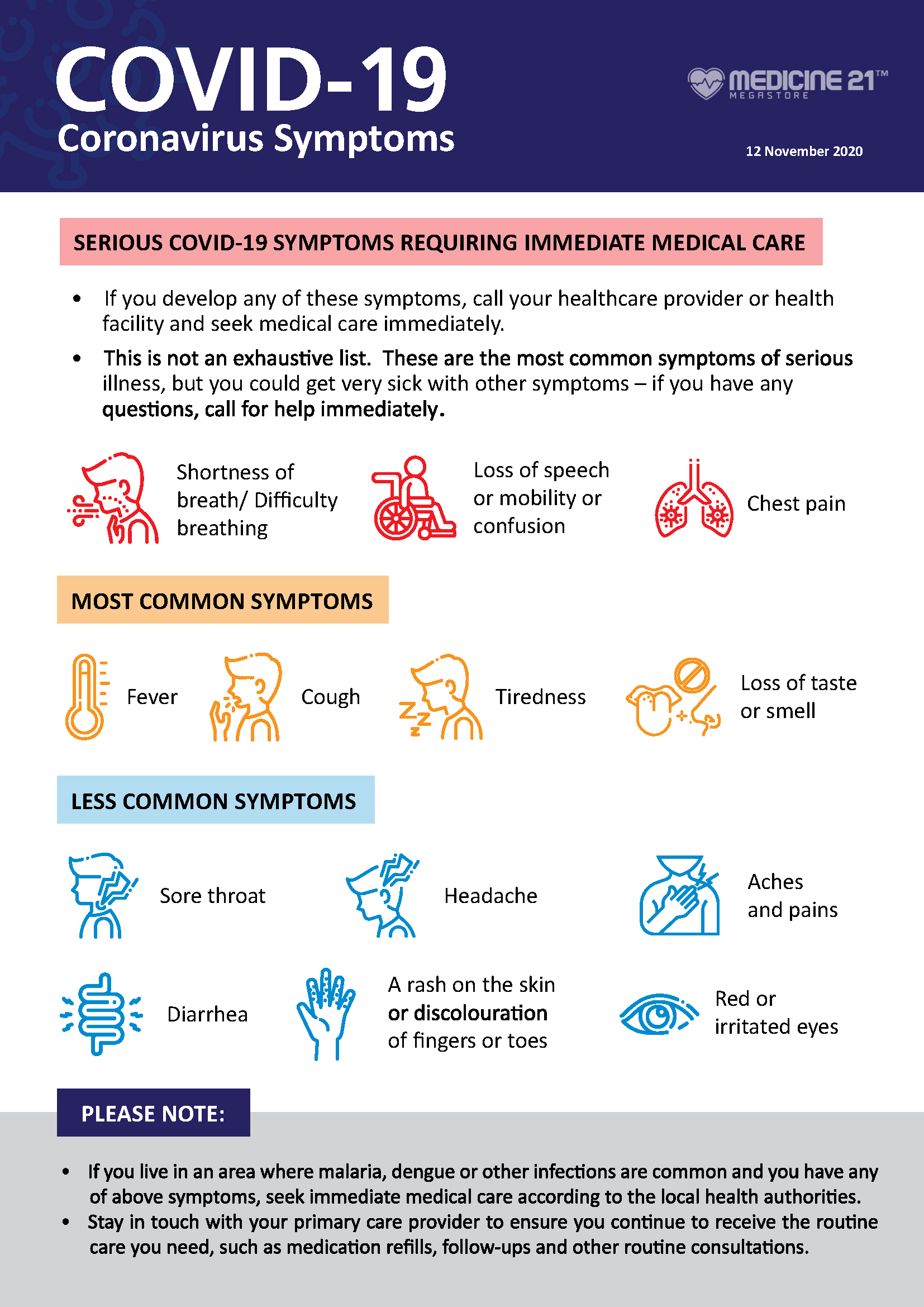
The following symptoms are considered mild in adults:
- mild upper respiratory tract symptoms such as a congested or runny nose, sneezing, or a scratchy or sore throat
- cough with no difficulty breathing
- new aches and pains, or lethargy or weakness without shortness of breath
- mild headache
- mild fever that responds to treatment
- loss of smell or taste
- loss of appetite
- nausea
- occasional vomiting or diarrhoea
- not drinking as much fluid (such as water) as usual in the last 24 hours
Some adults have no symptoms at all.
Children
The following symptoms are considered mild in children:
- mild upper respiratory tract symptoms such as a congested or runny nose, sneezing, or a scratchy or sore throat
- cough with no difficulty breathing
- not drinking as much fluid (such as water) as usual in the last 24 hours
- mild vomiting and diarrhoea (fewer than 4 times in the last 24 hours)
- mild headache or body aches
- mild fever
- mild fatigue
Some children have no symptoms at all.
Moderate symptoms
Adults
The following symptoms are considered moderate in adults:
- shortness of breath while walking around such as noticeably having to breathe more heavily while walking around the house
- persistent fever above 38oC that’s not responding to treatment
- persistent worsening cough that regularly produces mucus
- struggling to get out of bed and feeling dizzy or weak
- reduced fluid intake (drinking) over the last 24 hours (but more than half the normal intake)
- reduced urine output (‘weeing’) over the last 24 hours (producing less urine, but more than half the normal amount)
- vomiting or diarrhoea (more than 4 times in the last 24 hours, of either)
Children
The following symptoms are considered moderate in children:
- mild breathlessness but able to speak in sentences and eat, and comfortable while resting
- drinking less fluid (such as water) in the last 24 hours but more than half the normal intake
- they’ve not produced much urine (‘wee’) over the last 24 hours but more than half the normal amount
- vomiting or diarrhoea (more than 4 times in the last 24 hours, of either)
- unable or unwilling to stand or walk
- persistent high fever (temperature of greater than 38oC) that’s not responding to treatment
- is 3 months or younger and has any fever (a temperature of greater than 38oC)
Severe symptoms
Adults
The following symptoms are considered severe in adults:
- breathlessness at rest and/or unable to speak in sentences
- being unconscious, fainting or drowsy
- skin turning blue or pale
- cold and clammy, or pale and mottled, skin
- pain or pressure in the chest lasting more than 10 minutes
- confusion
- passing no urine (‘wee’) or a lot less urine than usual
- coughing up blood
- severe headache
If you are experiencing any severe symptoms call triple zero (000) for an ambulance and tell the ambulance staff that you have COVID-19.
Children
The following symptoms are considered severe in children:
- high-pitched wheezing sound while breathing (stridor)
- gurgling or grunting while breathing
- working very hard to breathe, or using chest or abdominal (tummy) muscles to breathe
- being too breathless to speak or feed, or long pauses between breaths
- nostril flaring
- turning blue around the mouth or lips
- head bobbing
- skin feels unusually cold and sweaty
- skin colour looks ‘patchy’ or very pale
- unconscious, drowsy, or floppy or limp
- they’ve not drunk much fluids (such as water) in the last 24 hours (less than half their normal intake)
- they’ve not produced much urine (‘wee’) in the last 24 hours (less than half their normal amount)
- severe headache that is so bad that they can’t do normal tasks involving movement, keep their eyes open, read, watch TV or concentrate — a baby or young child might not want to move their head, and they may screw up their eyes or grimace in pain
symptoms
A skin rash is a less common symptom of COVID-19. It may occur at different stages of the disease and in different forms. This may happen in both adults and children.
You should discuss skin changes related to COVID-19 with a doctor. Treatment may be needed in some instances.
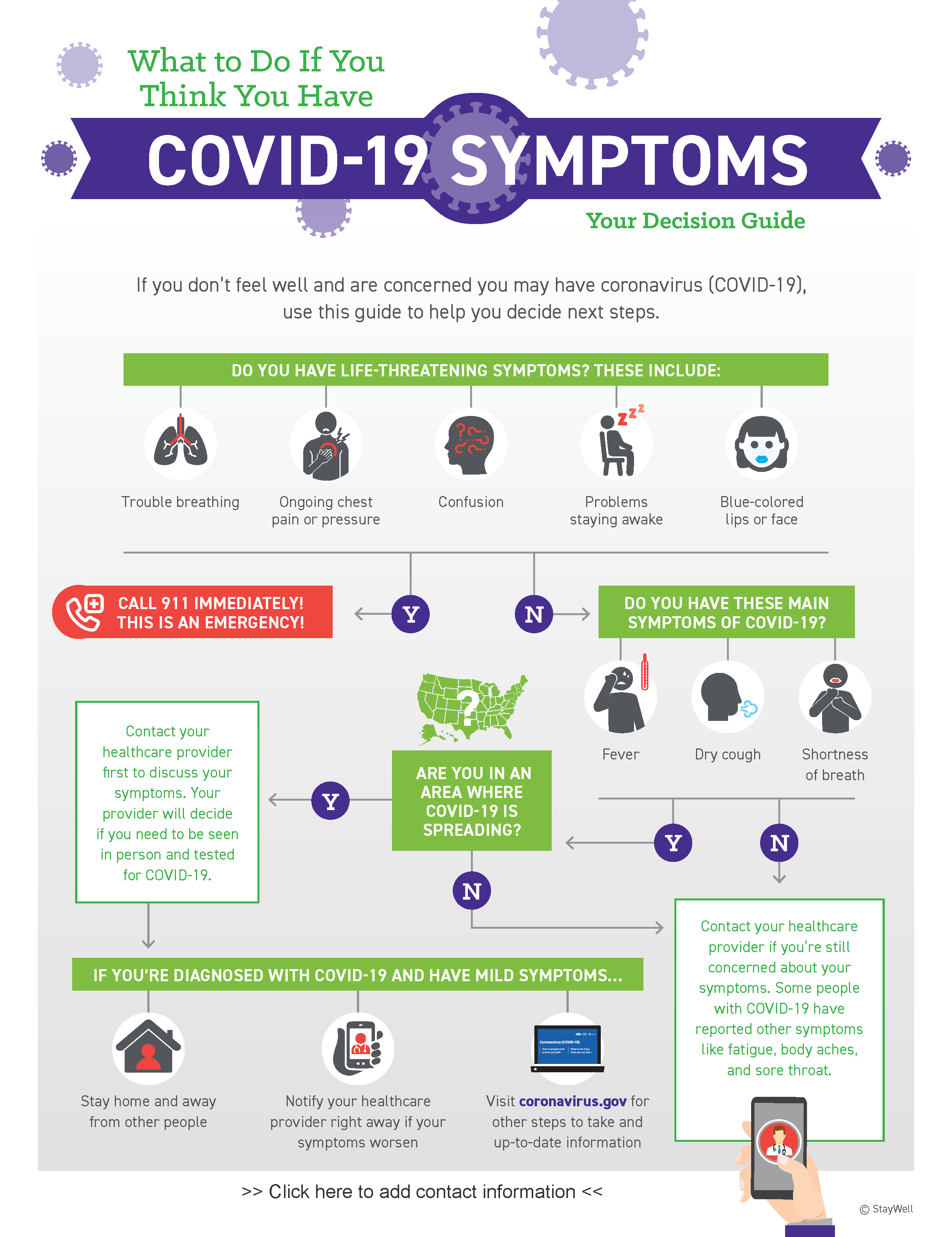
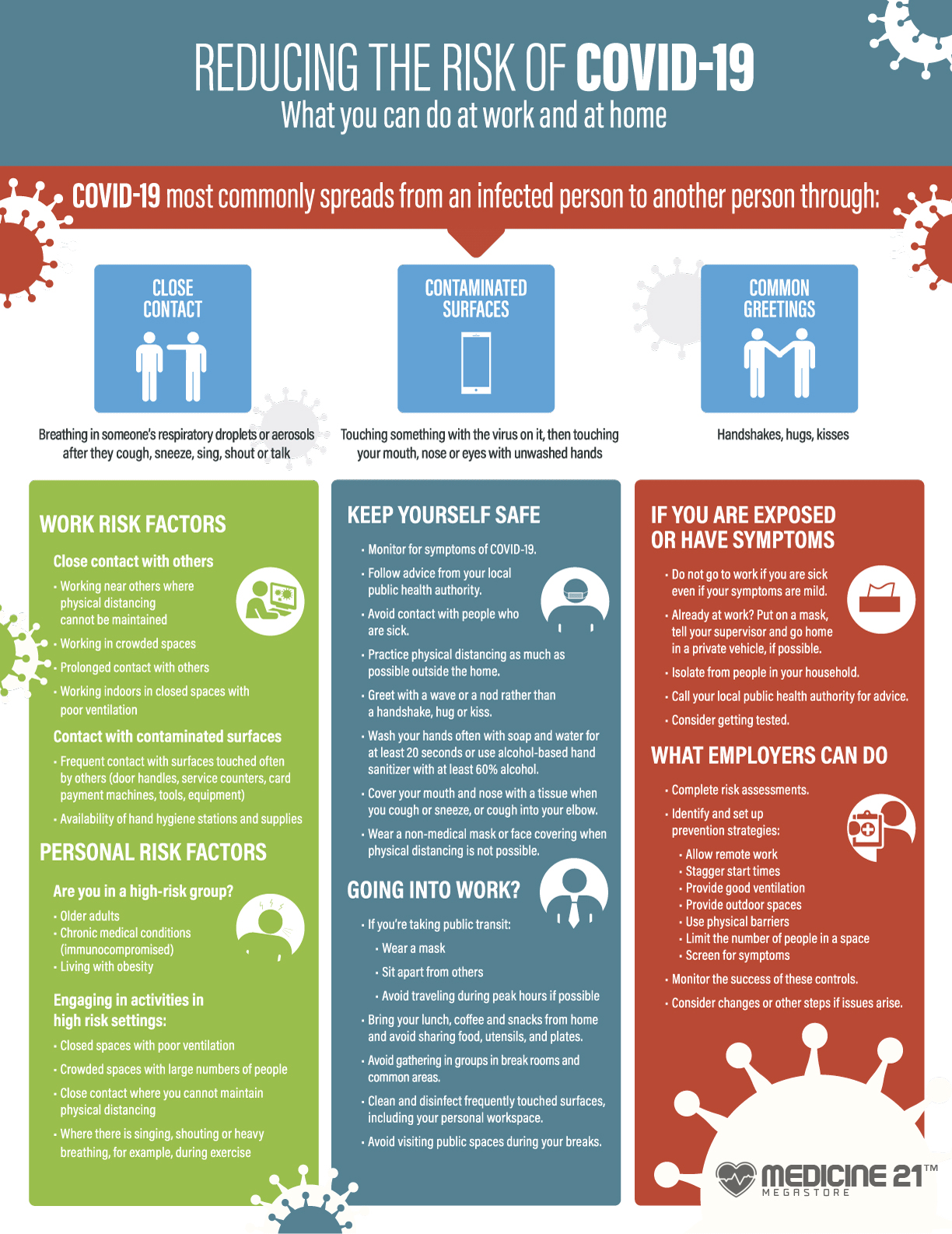
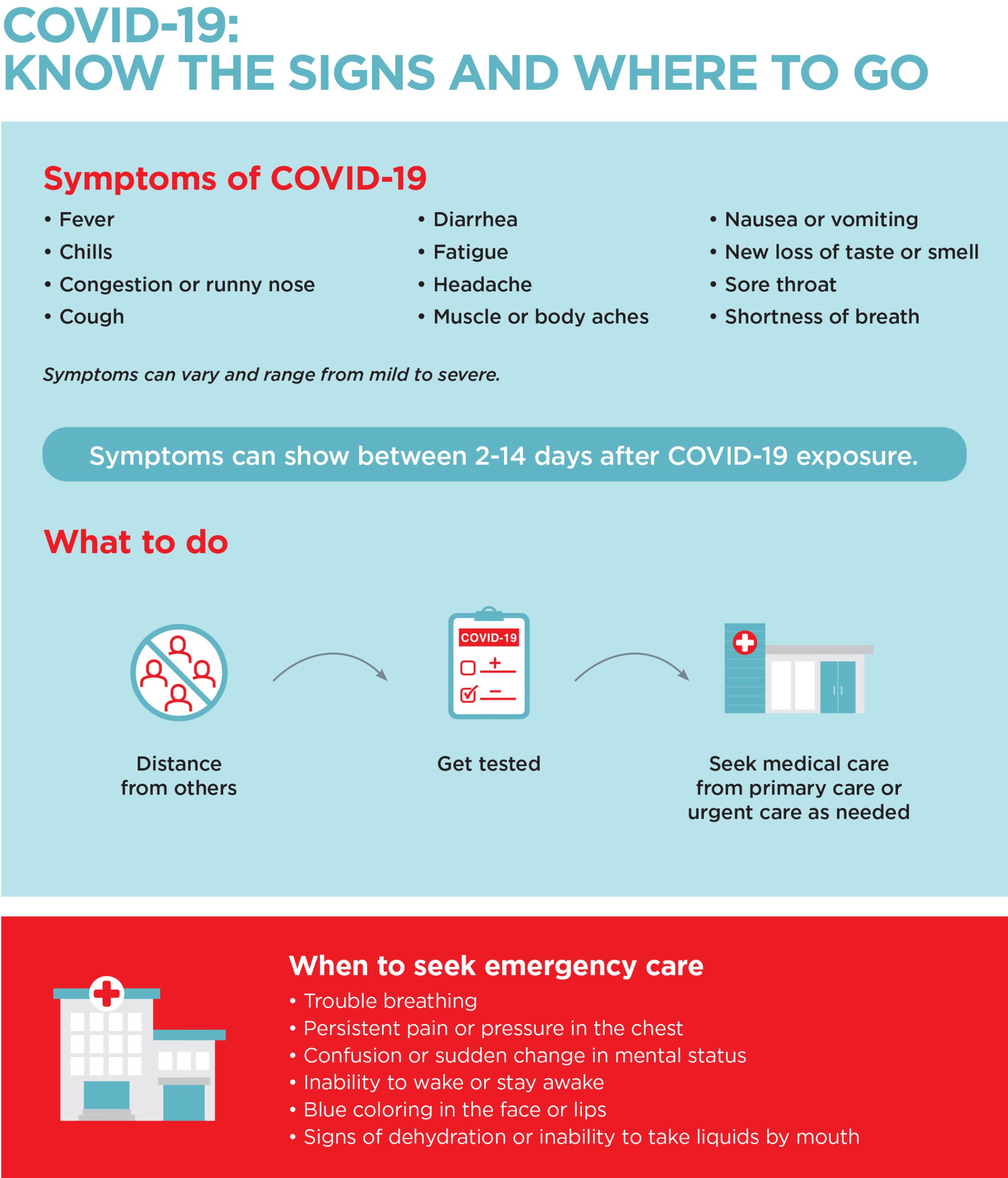
What should I do if I develop COVID-19 symptoms?
If you have any cold and flu like symptoms of COVID-19 — even if they are mild — you should get tested and stay at home while you are experiencing symptoms.
You should not visit high-risk places, such as hospitals, and aged and disability care places, for at least 7 days or until symptoms have gone or unless seeking immediate medical care.
Most people will have mild symptoms and can manage COVID-19 at home with over-the-counter medicines.
The Royal Australian College of General Practitioners (RACGP) has developed a guide for people managing COVID at home.
When should I seek medical advice?
You should contact a GP if you feel dizzy or lightheaded or your symptoms start to worsen.
You should contact a GP or health service if you’re pregnant, have any chronic conditions or have any concerns about your health. Your doctor may be able to assess you over the phone or by video.
Some people may be eligible to get COVID-19 oral medication prescribed by a doctor to reduce their chance of severe illness or hospitalisation. It is important to get tested for COVID-19 as soon as possible so you can get treatment early.
You can use the COVID-19 Symptom and Antiviral Eligibility Checker to find out if you are eligible for COVID-19 medication or if you need to get tested or seek medical help.
Wear a mask when in the practice and tell staff straight away that you have COVID-19.
If you experience any severe symptoms call triple zero (000) for an ambulance and tell the ambulance staff that you have COVID-19.
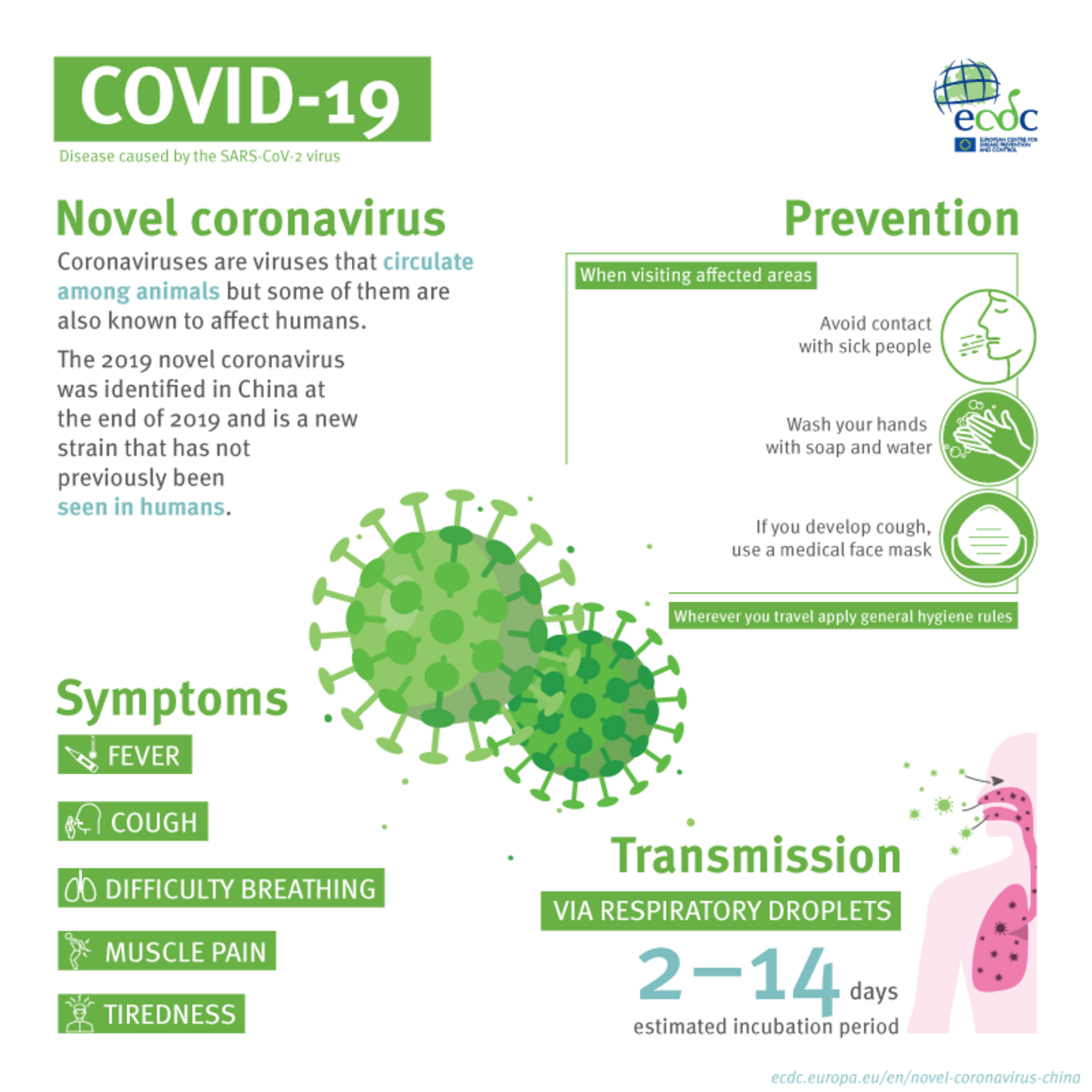
How soon after exposure to COVID-19 do symptoms appear?
The COVID-19 incubation period, which is the time between when a person is exposed to the virus and when their symptoms first appear, ranges from 1 to 14 days. Most people develop symptoms 5 to 6 days after being in contact with a person who has COVID-19.
When is a person with COVID-19 infectious, and can they transmit the virus to others before symptoms appear?
If you have COVID-19, you are considered infectious generally from 48 hours before your symptoms develop (or before your positive test if you don’t have any symptoms).
If you still have symptoms, you may still be contagious. However, people with COVID-19 can still transmit the virus whether they have symptoms or not.
People who still have acute respiratory symptoms after 7 days are still considered infectious. Acute symptoms include fever, cough, shortness of breath and sore throat.
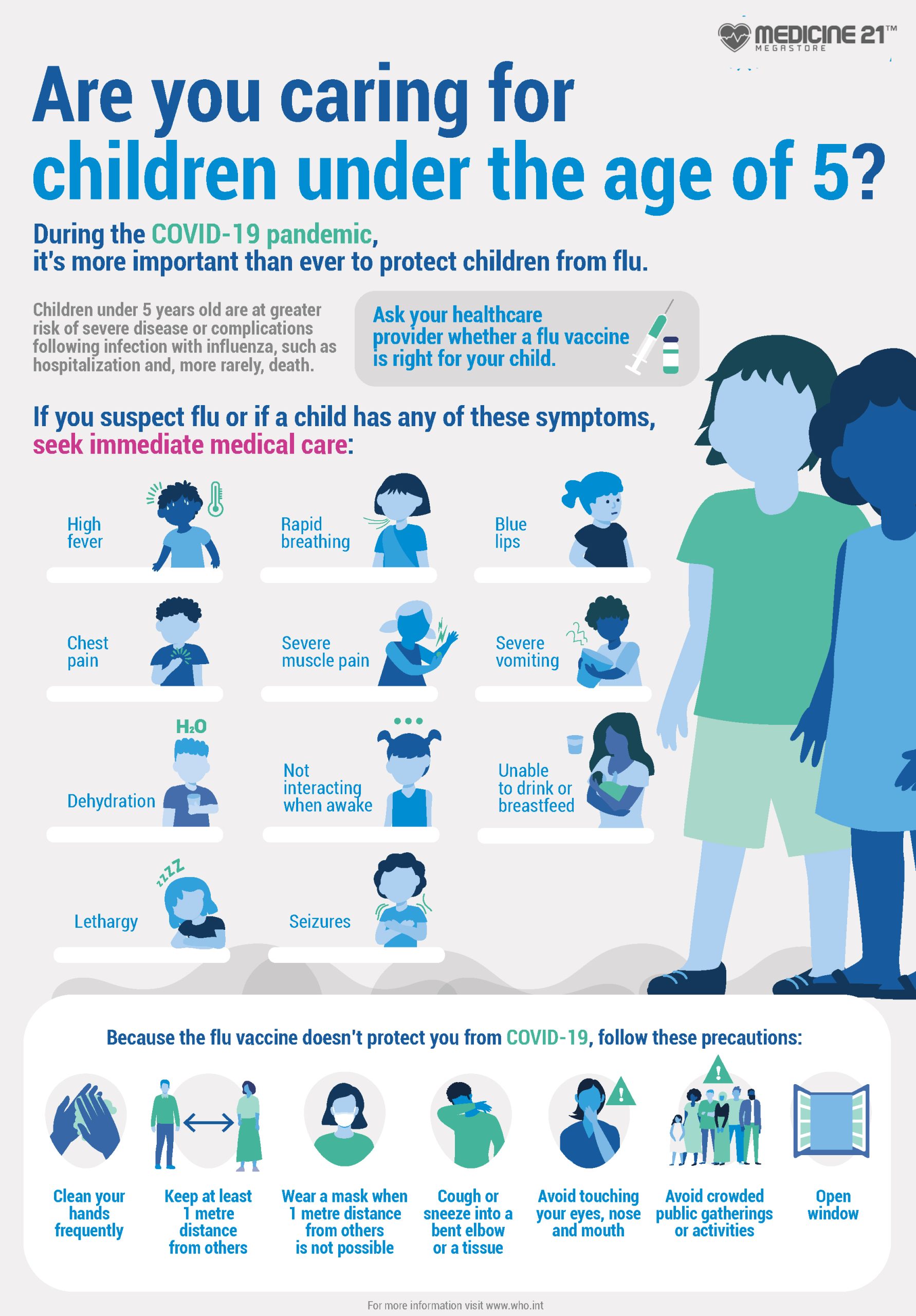
How does COVID-19 affect children?
COVID-19 is usually milder in children than in adults — it only very rarely causes severe illness. Around 98% of children and adolescents either get mild infection or have no symptoms at all.
Of those who do get symptoms, the illness is usually very similar to other respiratory viral illnesses — the most common symptoms are fever and cough. Children can also have symptoms like a runny nose and tiredness. Some children may have gastrointestinal symptoms like abdominal pain, diarrhoea or vomiting.
Some children may need hospitalisation and a smaller number may need to have intensive care. Studies have shown that children and adolescents with underlying medical conditions have a greater risk of developing severe disease and complications from COVID-19.
The conditions in children that increase the risk of being hospitalised with COVID-19 include but are not limited to:
- type 1 diabetes
- obesity
- being born premature
- heart disease including some congenital conditions
- immunocompromising conditions
- complex and chronic illnesses
Visit Pregnancy, Birth and Baby for more information on children and COVID-19.
Who is more at risk from COVID-19?
Some people are more at risk of serious illness from COVID-19. If you are more at risk and are feeling unwell, take a test as soon as you can. Speak to a doctor immediately if you are positive for COVID-19.
You are at a high risk of becoming very sick from COVID-19 and needing hospital treatment if you:
- are 70 years of age or older
- are 50 years of age or older with 2 risk factors including neurological disease, chronic lung disease (moderate or severe asthma needing inhaled steroids), obesity, heart disease, diabetes and kidney disease
- are an Aboriginal or Torres Strait Islander person who’s 30 years of age or older with one of the risk factors mentioned above
- are 18 years of age or older and moderately to severely immunocompromised
- live in a rural or remote area with limited healthcare services
- live in a residential aged-care facility
- have complex and significant disability
- are pregnant
- are on immunosuppressants
- have certain health conditions
Older people
The risk of serious illness from COVID-19 increases with age, particularly for people over 70 years old. This risk increases if you have a chronic condition or a weakened immune system.
People living with dementia or some form of cognitive condition may be less able to follow instructions or to let others know about possible COVID-19 symptoms. This is especially so if they find it difficult to communicate verbally or to express pain and discomfort. Someone who knows a person with dementia may be able to help see changes in their health.
People with disability
Some people with disability will be at greater risk of serious illness from COVID-19 because they:
- may have a chronic condition, or different conditions that overlap
- may have a weak immune system
- have difficulties physical distancing, especially people who rely on support and assistance from family, carers and support workers
- may be unable to safely wear a mask
- live in higher-risk accommodation such as group homes or larger facilities
Aboriginal and Torres Strait Islander peoples
Aboriginal and Torres Strait Islander peoples and people living in remote communities are at greater risk of COVID-19 for the following reasons:
- They experience higher rates of other health issues such as chronic diseases. This means they’re more susceptible to severe illness following COVID-19 infection.
- It can be harder to get healthcare because of where some live. They might not have many services nearby and they might not have enough transport.
- People in the community can be very mobile and travel a lot between cities, towns and communities.
- Some communities have frequent visitors and they may have been exposed to COVID-19.
Pregnancy
If you are pregnant and have COVID-19, you have a higher risk of certain complications than non-pregnant females with COVID-19 of the same age. There is an increased risk of being admitted to hospital as well as needing ventilation.
COVID-19 also increases the risk of certain pregnancy complications including premature birth and stillbirth, or your baby needing admission to a newborn care unit. If you have certain health conditions, you’re more likely to have severe illness if you get COVID-19 during pregnancy. These conditions include:
- being older than 35 years
- being overweight or obese
- pre-existing high blood pressure
- pre-existing type 1 or type 2 diabetes
Visit Pregnancy, Birth and Baby for more information about pregnancy and COVID-19.
People who are immunocompromised
If your immune system is compromised, you are more likely to become severely ill with COVID-19.
You are considered moderately to severely immunocompromised if you have:
- been living with disability with multiple conditions including frailty
- blood cancer or some red blood cell disorders (thalassemia, sickle cell disease)
- been a transplant recipient
- a primary or an acquired (HIV) immunodeficiency
- had chemotherapy or whole-body radiotherapy in the last 3 months
- had high dose corticosteroids or pulse corticosteroid therapy in the last 3 months
- had immunosuppressive treatments in the last 3 months
- had rituximab in the last 12 months
- cerebral palsy or Down Syndrome
- congenital heart disease
- certain medical conditions, listed below
People with underlying health conditions
Conditions that can increase your risk of severe COVID-19 illness include:
- chronic kidney failure
- heart disease
- chronic lung disease — excluding mild or moderate asthma
- blood cancer such as leukaemia, lymphoma or myelodysplastic syndrome
- non-haematological cancer (diagnosed in the past 5 years)
- childhood cancer
- diabetes
- severe obesity with a body mass index (BMI) of 40 kilograms per square metres or more
- chronic liver disease
- some neurological conditions such as stroke or dementia
- some chronic inflammatory conditions needing treatment
- poorly controlled blood pressure
- severe mental health condition
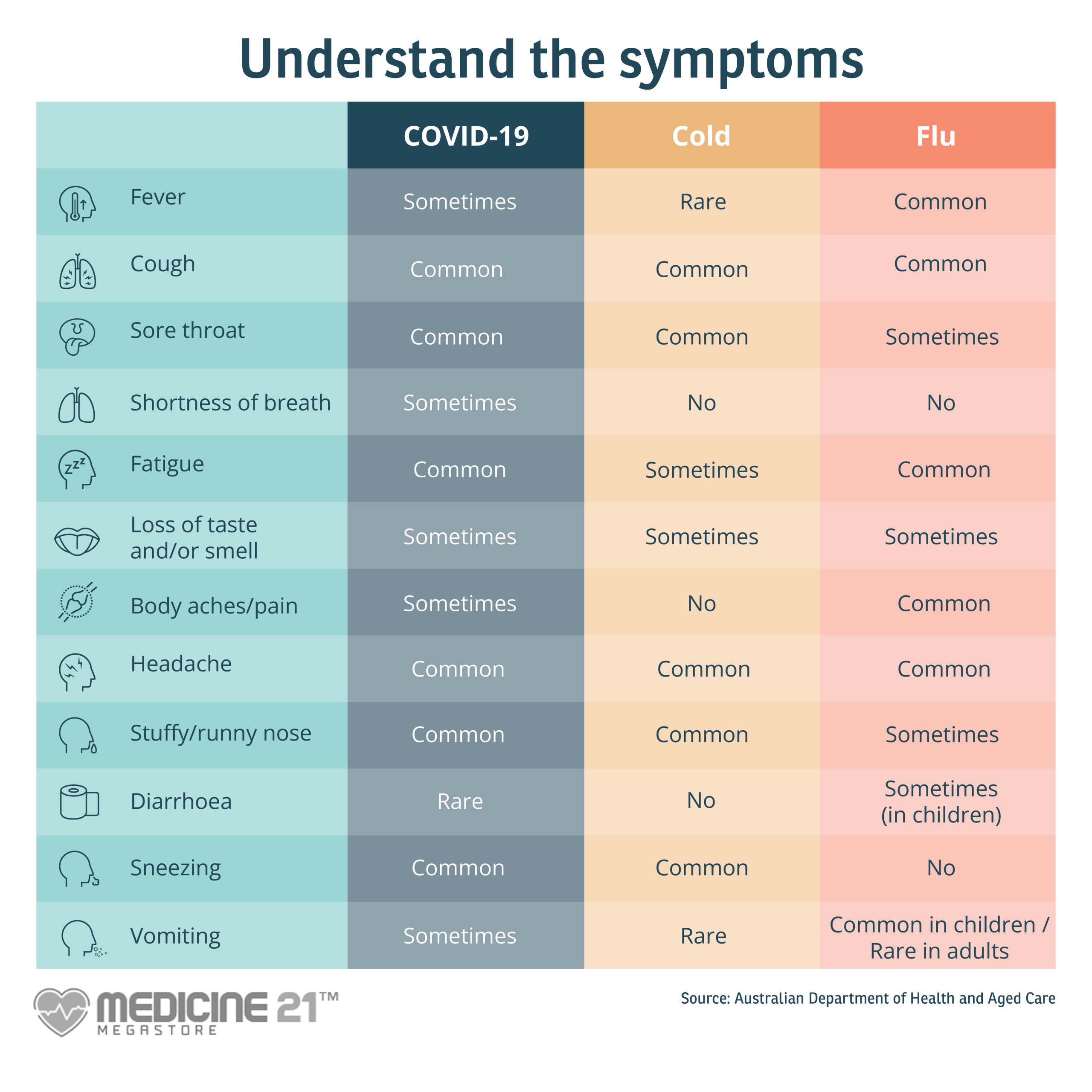
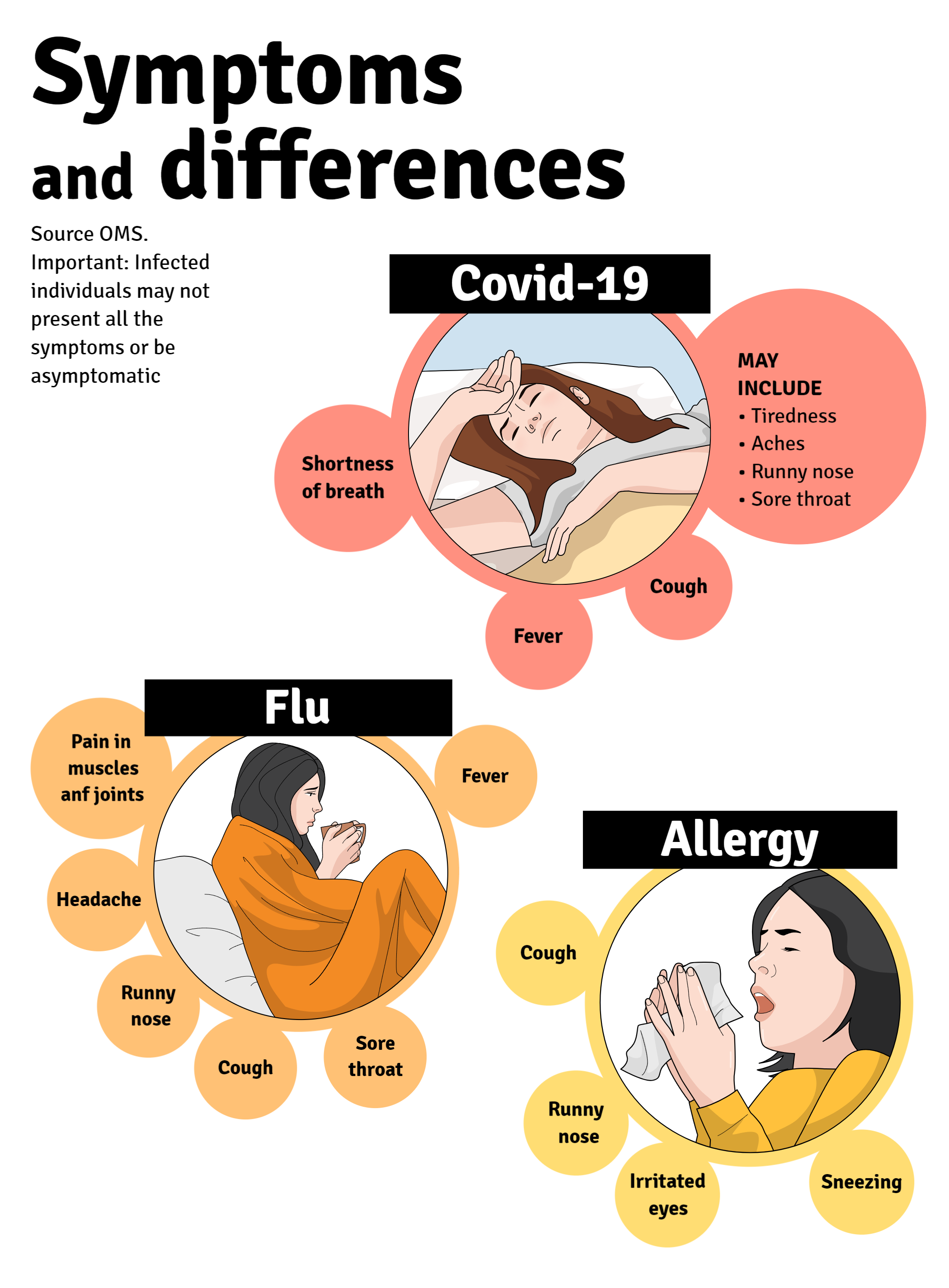
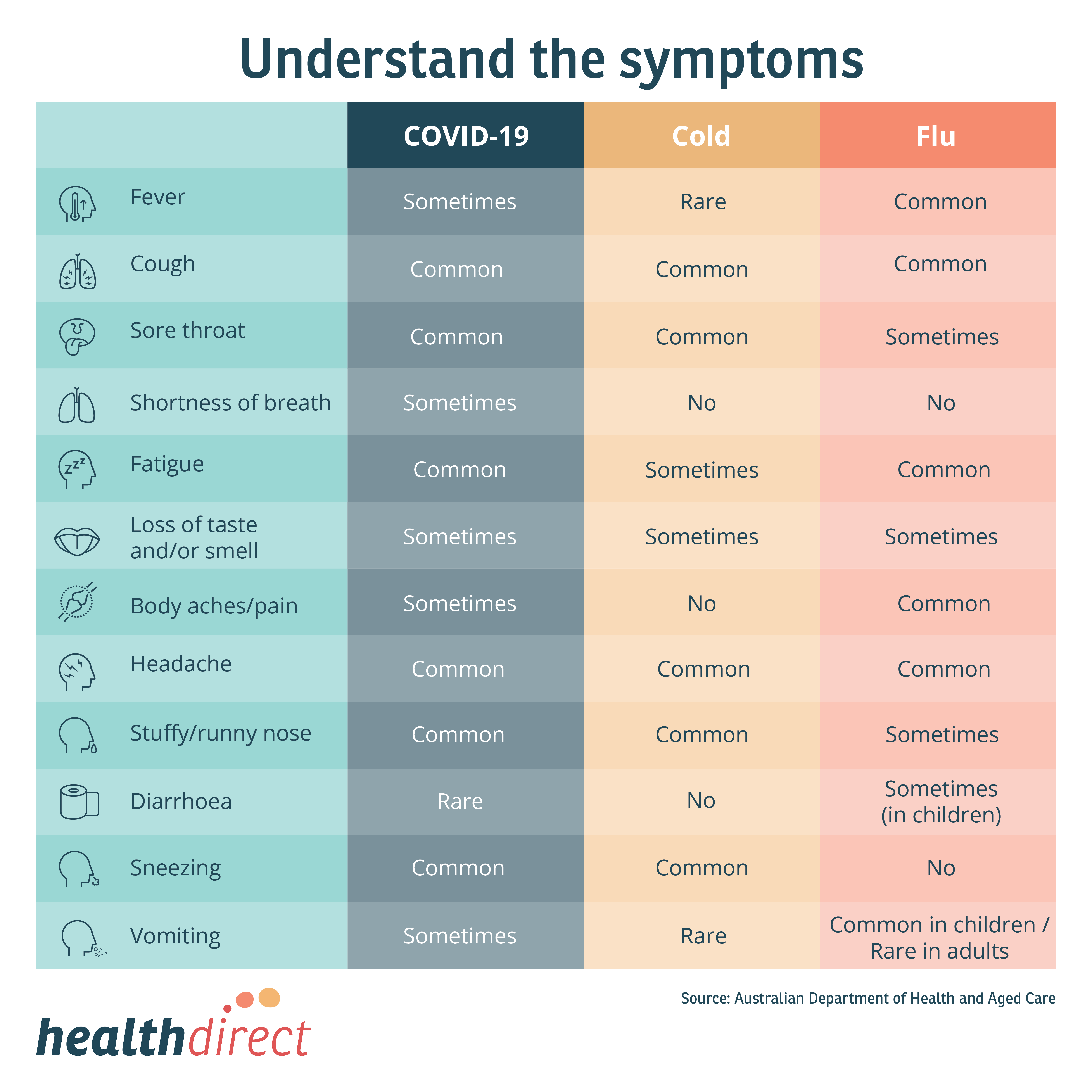
How is COVID-19 different from the flu (influenza)?
COVID-19 is caused by a coronavirus known as SARS-CoV-2. The seasonal flu is caused by different types of influenza virus.
Both diseases are infections and can cause respiratory symptoms such as a sore throat, runny nose and cough, as well as fever.
However, there are some differences:
- Influenza often includes muscle pains and headache, while these symptoms are less common in COVID-19.
- So far, severe COVID-19 has mainly affected older age groups and people with chronic illnesses. But severe cases of the flu can sometimes make otherwise healthy people, children and pregnant females very sick too.
How does COVID-19 affect children?
Generally, COVID-19 is milder in children than in adults. Most children with symptoms experience similar illness to other respiratory infections, including fever, cough, runny nose and tiredness. Some children may have gastrointestinal symptoms like abdominal pain, diarrhoea or vomiting.
Although rare, some children may need hospitalisation and a smaller number may need intensive care. Studies show that children and adolescents with underlying medical conditions have a greater risk of severe disease and complications from COVID-19 and other respiratory illnesses.
Some children may need hospitalisation and a smaller number may need to have intensive care. Studies have shown that children and adolescents with underlying medical conditions have a greater risk of developing severe disease and complications from COVID-19.
Conditions that increase risk for severe illness with COVID-19 include but are not limited to:
- type 1 diabetes
- obesity
- being born premature
- heart disease including some congenital conditions
- immunocompromising conditions
- complex and chronic illnesses
Visit Pregnancy, Birth and Baby for more information on children and COVID-19.
Who is more at risk from COVID-19?
Some people are more at risk of becoming very sick from COVID-19. If you are more at risk and are feeling unwell, take a test immediately then speak to a doctor as soon as you can if the result is positive.
You are at a high risk of becoming very sick from COVID-19 and needing hospital treatment if you:
- are 70 years of age or older
- are 50 years of age or older with 2 risk factors including neurological disease, chronic lung disease (including moderate or severe asthma needing inhaled steroids), obesity, heart disease, diabetes and kidney disease
- are an Aboriginal or Torres Strait Islander person who’s 30 years of age or older with one of the risk factors mentioned above
- are 18 years of age or older and moderately to severely immunocompromised
- live in a rural or remote area with limited healthcare services
- live in a residential aged-care facility
- have complex and significant disability
- are pregnant
- are on immunosuppressants
- have certain health conditions
Older people
The risk of serious illness from COVID-19 increases with age, particularly for people over 70 years old. This risk increases if you have a chronic condition or a weakened immune system.
People living with dementia or some form of cognitive condition may be less able to follow instructions or to let others know about possible COVID-19 symptoms.
People with disability
Some people with disability will be at greater risk of serious illness from COVID-19 because they may:
- have a chronic condition, or different conditions that overlap
- have a weak immune system
- have difficulties physical distancing, especially people who rely on support and assistance from family, carers and support workers
- be unable to safely wear a mask
- live in higher-risk accommodation such as group homes or larger facilities
Aboriginal and Torres Strait Islander peoples
Aboriginal and Torres Strait Islander peoples and people living in remote communities are at greater risk of COVID-19 because of factors such as higher rates of health issues and less access to healthcare services.
Pregnancy
If you are pregnant and have COVID-19, you have a higher risk of hospitalisation, ventilation, premature birth, stillbirth, or your baby needing special care. If you have any of the following conditions, you’re more likely to have severe illness if you get COVID-19 during pregnancy:
- being older than 35 years
- being overweight or obese
- pre-existing high blood pressure
- pre-existing type 1 or type 2 diabetes
Visit Pregnancy, Birth and Baby for more information about pregnancy and COVID-19.
People who are immunocompromised
If you have a weakened immune system, you are more likely to become severely unwell with COVID-19. You are considered moderately to severely immunocompromised if you have:
- been living with disability with multiple conditions including frailty
- blood cancer or some red blood cell disorders (thalassemia, sickle cell disease)
- been a transplant recipient
- a primary or an acquired (HIV) immunodeficiency
- had chemotherapy or whole-body radiotherapy in the last 3 months
- had high dose corticosteroids or pulse corticosteroid therapy in the last 3 months
- had immunosuppressive treatments in the last 3 months
- had rituximab in the last 12 months
- cerebral palsy or Down Syndrome
- congenital heart disease
- certain medical conditions, listed below
People with underlying health conditions
Conditions that can increase your risk of severe COVID-19 illness include:
- chronic kidney failure
- heart disease
- chronic lung disease — excluding mild or moderate asthma
- blood cancer such as leukaemia, lymphoma or myelodysplastic syndrome
- non-haematological cancer (diagnosed in the past 5 years)
- childhood cancer
- diabetes
- severe obesity with a body mass index (BMI) of 40 kilograms per square metres or more
- chronic liver disease
- some neurological conditions such as stroke or dementia
- some chronic inflammatory conditions needing treatment
- poorly controlled blood pressure
- severe mental health condition