Pneumonia
This used to describe a lower respiratory tract infection which often occurs when normal defences are impaired
It is a blanket term which can be subdivided into a number of types, with different causes and features:
Lobar pneumonia
This is characterised by continuous consolidation of a lobe of the lung.
It is most frequently due to a bacterial agent, e.g., Streptococcus pneumoniae, Klebsiella pneumoniae, Haemophilus influenzae and Moraxella catarrhalis.
Bronchopneumonia
This is characterised by discontinuous areas of consolidation, often bilaterally in the basal lobes, with predominance around the bronchioles.
It is usually caused by bacterial agents: Staph aureus and Haemophilus influenzae are most frequently implicated.
Atypical pneumonia
This refers to pneumonia due to rarer causes and presents differently to classical pneumonia in that it is usually not associated with lobar consolidation.
Typical presenting symptoms include fatigue, malaise and a low-grade fever
Causative pathogens include Mycoplasma pneumoniae, Chlamydia psittaci and Legionella pneumophila.
Pneumonia is also classified according to the how and where you contract it:
Community-acquired
This refers to pneumonia which is contracted outside of the hospital.
Most common causes: Strep pneumoniae, H. influenzae, Moraxella catarrhalis
Hospital-acquired
This is defined as a pneumonia developed > 48 hours after a hospital admission.
Most often due to Staph aureus or Gram-negative enterobacteria (such as Pseudomonas aeruginosa)
Aspiration
This occurs in people with an incompetent swallow mechanism (e.g., stroke patients, intoxicated people) and those being intubated.
Causative pathogens include aerobic bacteria: Strep. pneumoniae, Staph aureus, Pseudomonas aeruginosa.
Aspiration pneumonia typically causes right lung consolidation as the right main bronchus is wider, straighter, and more vertical than the left.
Important Pathogens

Symptoms
Fever and malaise
Dyspnoea, pleuritic chest pain
Cough with purulent sputum/haemoptysis
Confusion
Expiratory crepitations
Sepsis, e.g., hypotension, tachycardia
Complications
Pleural effusions – associated with a one-sided (usually) parapneumonic effusion
Hypotension – secondary to loss of water in dehydration and/or from systemic vasodilation due to the body’s exaggerated immune response to bacteraemia (sepsis)
Atrial fibrillation – this usually resolves with treatment of pneumonia
Empyema – this is defined as pus in the pleural space. It is characterised by having a pH < 7.2, low glucose and raised LDH
Key tests
Blood test shows raised inflammatory markers, e.g., WCC and CRP:
CXR – shows consolidation, with lobar, bronchopneumonia or interstitial pattern
Sputum culture
Bronchoalveolar lavage is rarely needed (except for patients on ITU or those who have severe pneumonia which is failing to improve)
Management
Work out CURB-65 score to assess severity. Patients get 1 point for each risk factor
Confusion (mental tests core < 8)
Urea > 7mM
Respiratory rate >30/min
Blood pressure <90 systolic and/or 60mmHg diastolic
Age > 65
If the patient’s score is 0–1, indicates community management with oral antibiotics.
1st line is oral antibiotics e.g., amoxicillin (if allergic, then macrolide or tetracycline)
If the score 2 or more, indicates hospital treatment with IV antibiotics (and fluids).
1st line is dual antibiotic therapy, e.g., amoxicillin and macrolide (clarithromycin)
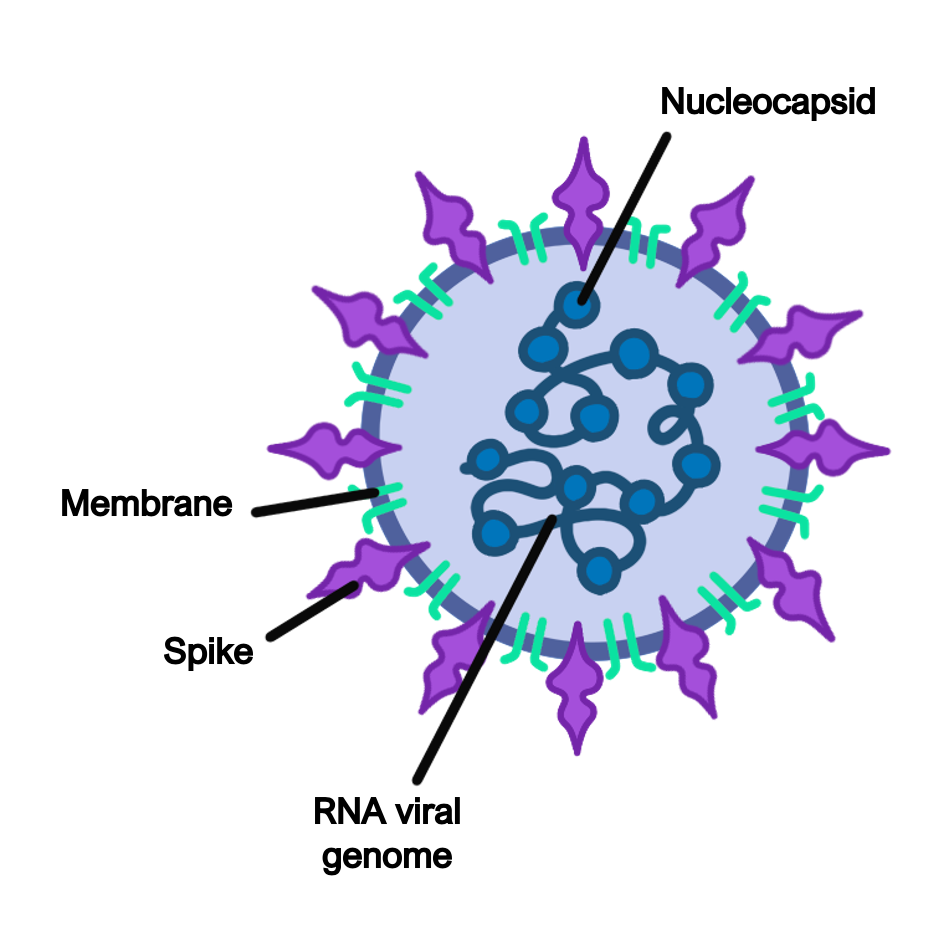
COVID-19
Coronavirus disease 19 (COVID-19) is a respiratory disease caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2).
The virus is spread mainly through respiratory droplets (e.g., from coughing).
The prevalence and mortality have decreased since the innovation of COVID-19 vaccines, which often involve multiple doses spread months apart.
Pathophysiology
The immune system usually stops SARS-CoV-2 at the level of the upper respiratory tract, so most people experience mild symptoms.
However, in some patients, the virus extends down to the lower respiratory tract, causing more severe symptoms.
Infected lung cells release pro-inflammatory cytokines (e.g., IL-6), leading to lung inflammation, alveolar damage, and pulmonary oedema.
SARS-CoV-2 also affects the endothelium of various organs, leading to increased risk of clotting and organ damage.
Symptoms
Cough
Fever
General malaise and fatigue
Altered sense of taste/smell
URTI symptoms (e.g., rhinorrhoea)
Key tests
Naso/oropharyngeal swab uses RT-PCR to detect the virus
Lateral flow test uses immunoassays (antibodies) to detect viral antigen
Chest X-ray may show ground-glass opacities or oedema
Management
Most only require conservative management (such as isolation and hydration)
Dexamethasone and antivirals (such as remdesivir) are used in severe COVID-19
Ventilatory support may be needed (such as CPAP if type 1 respiratory failure)
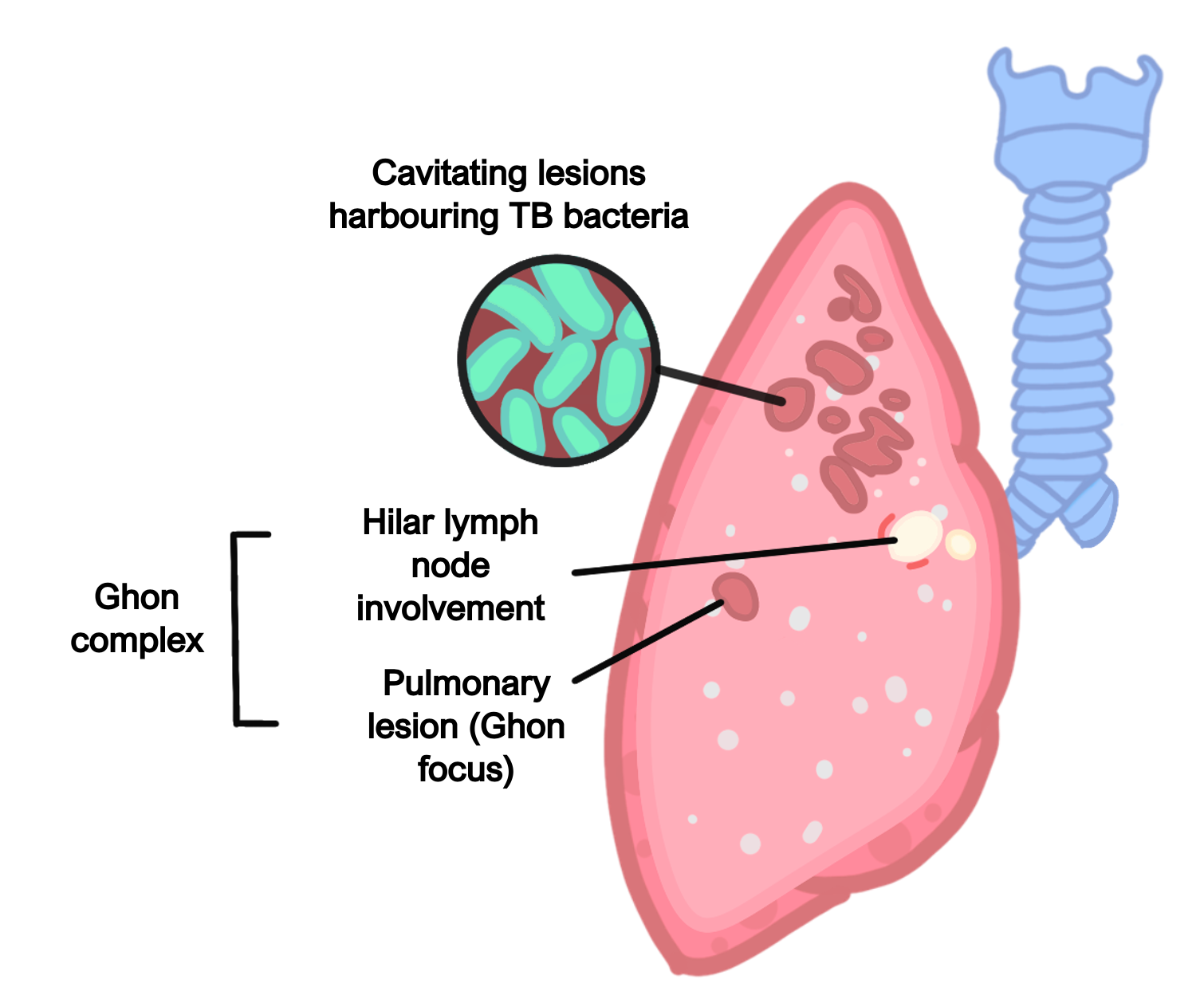
TB
This is a disease which is caused by the inhalation of Mycobacterium tuberculosis.
This is a mycobacterium which has a thick waxy capsule, making it harder to treat.
It typically affects patients from certain endemic countries (like India) and poorer socioeconomic backgrounds (where crowded living is more common, which increases transmission of the disease).
Pulmonary Symptoms
Chest pain
Malaise and weight loss
Low grade fever and night sweats
Persistent cough with haemoptysis
Clubbing and erythema nodosum
Potential Bronchiectasis
Extrapulmonary Symptoms
Meningitis – fever, neck stiffness and photophobia with a headache.
Pott’s disease (vertebrae) – this causes lower back pain, leading to vertebral narrowing and vertebral collapse/pathological fractures
Urogenital TB – this leads to cystitis which is unresponsive to conventional antibiotics
Miliary TB – this is when TB becomes disseminated, leading to formation of granulomas throughout the body
Key tests
CXR – shows opacification, cavitations and can show miliary TB
Nucleic acid amplification test (NAAT) of sputum sample
Sputum sample can also be smear-stained for acid-fast bacilli and cultured
HIV test – as this commonly co-occurs with TB
Management
This involves a regime of antibiotics targeted against Mycobacterium tuberculosis e.g., rifampicin, isoniazid, pyrazinamide and ethambutol for 2 months, followed by rifampicin and isoniazid for a further 4 months
