Overview
Sepsis is a dysregulated host response to infection leading to life-threatening organ dysfunction.
Sepsis is a commonly encountered problem in the healthcare setting and a major cause of morbidity and mortality. In its most simplistic form, sepsis is organ dysfunction secondary to an infection. It is regarded as a dysregulated host response to infection that is associated with both clinical and biochemical abnormalities.
It can be difficult to understand sepsis because the terminology used to define the condition has changed over the years and there is no universal agreement. In addition, in clinical practice, we see organ dysfunction in many systemic diseases. This means it may be difficult to truly say the organ dysfunction is secondary to an infection, especially if a specific organism is not identified that is not uncommon.
In practice, if we suspect an underlying infection and we identify clinical and biochemical abnormalities consistent with organ dysfunction, we can define sepsis. Several scoring systems are available to help us make this diagnosis. Sepsis is most commonly attributable to bacterial infections and treatment centres on prompt recognition and administration of intravenous antibiotics.
Definitions
Several important definitions are used to define sepsis and the association severity.
The definition of sepsis has changed over the years and there is no universal agreement. Sepsis represents a continuous spectrum of severity from early infection to life-threatening organ dysfunction.
Systemic inflammatory response syndrome
Traditionally, sepsis was defined using the ‘systemic inflammatory response syndrome’ (SIRS) criteria. SIRS is essentially a clinical syndrome due to dysregulated inflammation that is defined by the presence of ≥2 of the following:
- Temperature: > 38.0º or < 36.0º
- Heart rate: > 90/min
- Respiratory rate: > 20/min
- White cell count: > 12 x109/L or < 4 x109/L
The presence of SIRS and a suspected or identified source of infection was originally used to define sepsis. This has fallen out of favour in recent years because SIRS may be caused by a whole number of conditions (e.g. autoimmune disease, pancreatitis, burns, vasculitis, etc) and not just infection.
Early sepsis
Sepsis lies on a spectrum of severity from simple infection and bacteraemia (i.e. evidence of infection without organ dysfunction) to severe multi-organ failure.
The early recognition and treatment of sepsis can be life-saving. This is why there has been significant emphasis on the recognition of sepsis in clinical practice. Several scoring systems can be used to try and detect early signs of sepsis. These include:
- qSOFA (quick Sepsis Related Failure Assessment): aims to identify patients at increased risk of poor outcomes outside the ITU environment. It consists of three components:
- Mental status (score 1 if altered mental status)
- Respiratory rate (score 1 if ≥ 22)
- Systolic BP (score 1 if ≤ 100)
- NEWS (National Early Warning Score): a score derived from a patients’ observations (RR, O2 sats, HR, BP, GCS, Temperature) that alerts healthcare staff to early deterioration that warrants a review.
Sepsis
The modern definition of sepsis has been determined by the 2016 Society of Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM) task force. They define sepsis as:
“Life-threatening organ dysfunction caused by a dysregulated host response to infection”
Organ dysfunction is defined as an increase of ≥2 points in the Sequential Organ Failure Assessment (SOFA) Score. The SOFA score is an intensive care unit (ICU) tool that helps to predict mortality based on clinical and biochemical data. It is well-validated for use in sepsis.
There are several domains contributing to the score that each reflects an organ dysfunction:
- Respiratory dysfunction: Pa02, Fi02, need for ventilation
- Cardiovascular dysfunction: Blood pressure, need for inotropes
- Renal dysfunction: Acute kidney injury
- Haematological dysfunction: Platelet count, coagulation
- Liver dysfunction: Bilirubin
- Neurological dysfunction: Glasgow coma score
An infection should be suspected based on the presence of clinical features (e.g. productive cough, dysuria) and supporting evidence for infection based on microbiological and radiological data (e.g. culture results, CT showing a collection).
Septic shock
Shock describes circulatory failure resulting in inadequate tissue perfusion and insufficient delivery of oxygen. When this is secondary to sepsis we term it ‘septic shock’. This is a type of distributive shock because it is caused by peripheral vasodilatation leading to abnormal volume distribution and inadequate perfusion.
In relatively simple terms, septic shock is the presence of sepsis with hypotension (mean arterial pressure < 65 mmHg) despite adequate fluid resuscitation.
Patients with septic shock commonly require ICU support and inotropes (medicines that change the force of the hearts contraction and cause blood vessel vasoconstriction) to maintain adequate blood pressure.
Multiple organ dysfunction syndrome
The most severe end of sepsis is the development of multiple organ dysfunction syndrome (MODS). This refers to progressive organ dysfunction whereby homeostasis cannot be maintained without intervention. MODS is commonly the result of sepsis but can also be caused by non-infectious aetiologies.
For more information see our Multi-organ dysfunction syndrome note.
Aetiology
Sepsis is most commonly caused by bacterial infections.
A variety of infectious agents can lead to sepsis of which bacteria are the most commonly implicated.
- Bacteria (e.g. Streptococcus, Staphylococcus, Escherichia)
- Viruses (e.g. Influenza, Coronavirus, Respiratory syncytial virus)
- Fungi (e.g. Candida, Aspergillus).
Importantly, in up to 50% of cases of sepsis, an organism cannot be identified.
Risk factors
There are several risk factors that increase the risk of sepsis. These include:
- Very young (<1 years old)
- Very old (>75 years old) or frail
- Immunosuppressed (use of chemotherapy, long-term steroids, transplant recipients, immunodeficiencies, immunosuppressive agents)
- Recent surgery (or invasive procedure)
- Intravenous drug misuse
- Indwelling lines (e.g. dialysis catheter)
- Breach of skin integrity (e.g. cuts, burns)
Pathophysiology
Sepsis is characterised by a dysregulated host immune response.
Sepsis is a complex process involving the infectious organism (i.e. the pathogen) and the host immune response to that pathogen. In general, the transition from infection to sepsis is usually marked by a release of many pro-inflammatory mediators (e.g. tumor necrosis factor-α and interleukin (IL)-1β) that cause a systemic response leading to organ damage.
This systemic inflammatory response may be seen in the absence of infection, which is why there has been a move away from the traditional SIRS criteria for sepsis. There are many reasons why this systemic inflammatory response occurs including the virulence of the pathogen, excess production of proinflammatory cytokines at the initial site of infection, prominent activation of the complement system, and underlying genetic factors.
The consequence of this inflammatory response is cellular injury that occurs due to a variety of factors including tissue ischaemia, direct injury by pro-inflammatory mediators, and altered rates of apoptosis. Cellular injury culminates in organ dysfunction, which if severe, can lead to multi-organ dysfunction syndrome.
Clinical features
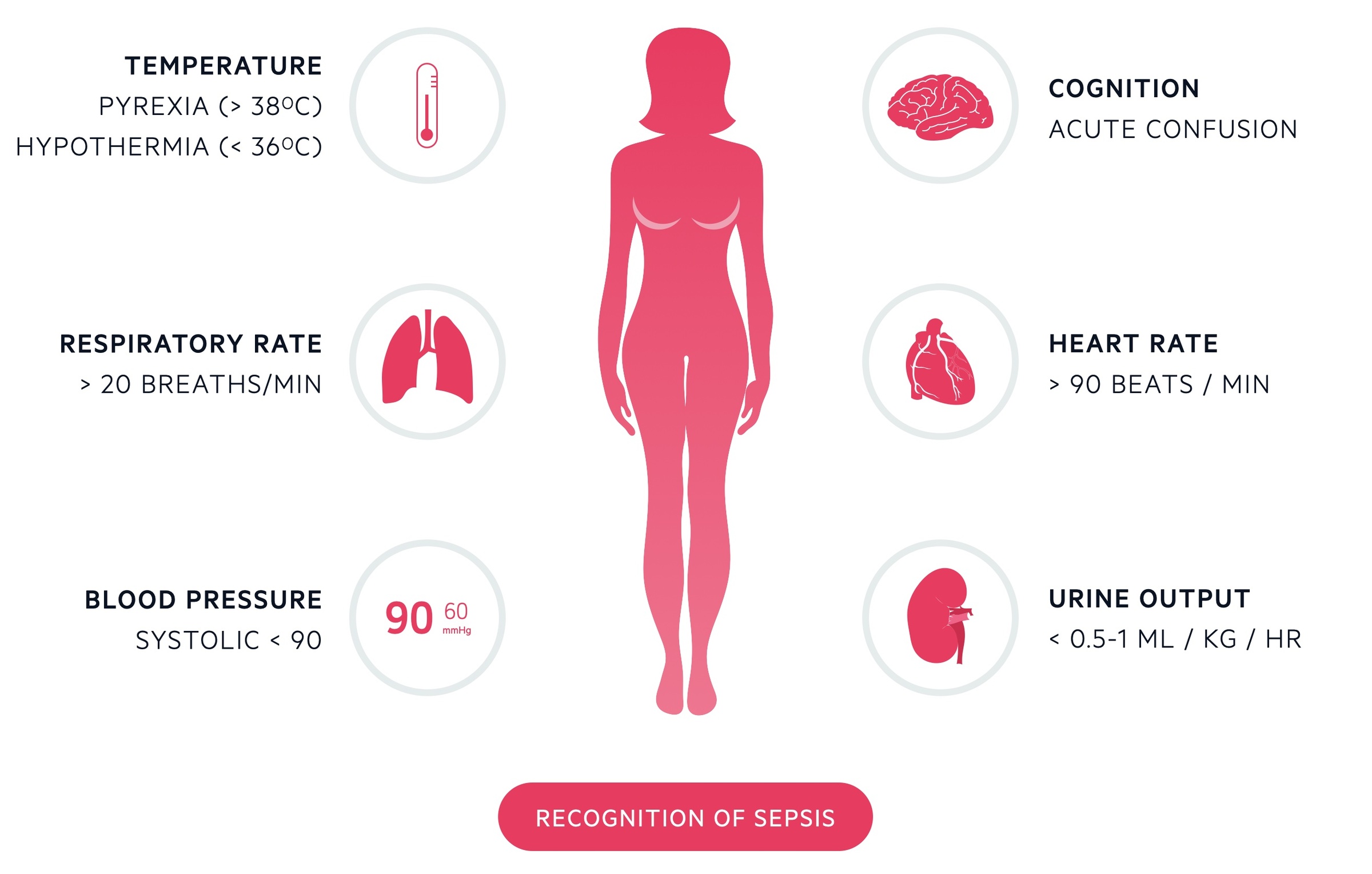
Classic features of sepsis include fever, tachycardia, tachypnea, and hypotension.
The clinical features of sepsis are often non-specific and may be attributable to other severe illnesses (e.g. pancreatitis).
Signs & symptoms
- Features of a specific infection (e.g. productive cough, dysuria, abscess, headache)
- Warm and flushed skin (vasodilatation due to inflammatory mediators)
- Cool, mottled skin (features suggestive of shock)
- Prolonged capillary refill time (features suggestive of shock)
- Febrile (>38.0º)
- Hypothermic (<36.0º)
- Tachycardia (>90)
- Tachypnea (>20)
- Hypotension (< 90 mmHg or decrease >40 mmHg)
Features of organ dysfunction
- Respiratory: hypoxia
- Cardiovascular: hypotension
- Gastrointestinal: jaundice, ileus (absent bowel sounds, distended abdomen, vomiting)
- Haematological: bleeding, bruising
- Neurological: altered mental status, agitated, reduced consciousness
- Renal: low urine output, anuric
Diagnosis
A prompt diagnosis of sepsis is usually made on early clinical suspicion.
A delay in the diagnosis of sepsis whilst awaiting investigations can lead to significant morbidity and mortality. Therefore, the diagnosis is usually made on clinical suspicion based on early observations and clinical assessment. Based on these data, treatment can be instigated.
A formal diagnosis may be made retrospectively based on the return of investigations (e.g. positive blood culture and evidence of acute kidney injury) in the context of the initial presentation (e.g. hypotension, altered mental status). In the absence of an identified pathogen, an improvement with antibiotics may indicate the cause of deterioration is an underlying infection. If there is no suggestion of an infection on subsequent investigations then treatment can be stepped down.
Any patient with suspected sepsis should have urgent observations and a clinical assessment. Features that suggest a high risk of severe illness or death from sepsis include:
- Heart rate: >130/min
- Respiratory rate: >25/min
- Blood pressure: <90 mmHg or >40 mmHg drop
- Level of consciousness: new altered consciousness
- Oxygen saturation: new need foo ≥40% oxygen to maintain sats >92% (88% for CO2 retainers)
- Urine output: <0.5 ml/kg/hour or not passed any for >18 hours
- Skin: mottled appearance, cyanosis, or non-blanching rash
NOTE: Do not use a person’s temperature as the sole predictor of sepsis and do not rely on fever or hypothermia to rule sepsis either in or out.
All patients with suspected sepsis should be urgently transferred to a hospital if they have high-risk criteria or they are < 17 years ago and their immunity is impaired by drugs or illness. Outside of the hospital setting, patients with moderate to high-risk criteria should be assessed to see whether they need treatment in a hospital.
Investigations & management
Investigations and management are completed concurrently in patients with suspected sepsis.
Any patient with suspected sepsis should be managed with the SEPSIS-6 principles in mind.
The sepsis six bundle is a protocol by which a patient may be investigated and treated for sepsis. It is by no means exhaustive but incorporates key investigation and treatment points. The bundle should be initiated and completed within one hour of recognition of the signs. All patients with a significant infection should have a senior review. Further support may be required including vasopressors (e.g. noradrenaline) to maintain blood pressure, given in A&E resus or ITU. The sepsis bundle can be remembered as ‘Three IN, Three OUT’.
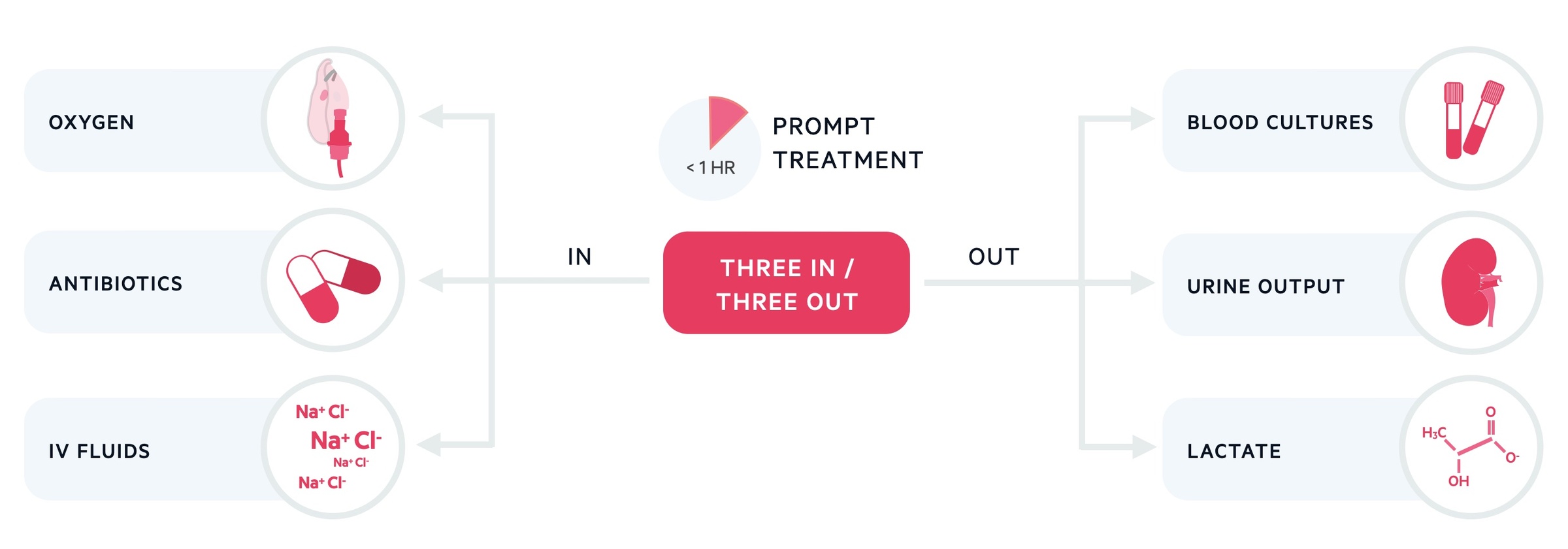
Three In
Patients should receive high flow oxygen to achieve appropriate target saturations. A target of 94-98% is appropriate for the majority of patients. Those at risk of carbon dioxide retention (e.g. chronic obstructive pulmonary disease) should have a target of 88-92%.
Intravenous (IV) fluids should be started, often 500 mL of a crystalloid over 15 minutes with reference to the patients’ haemodynamic status and co-morbidities. It is important to choose a crystalloid with a sodium content between 130-154 mmol/L.
Antibiotics are key and should be given without delay, the choice of antibiotics should be guided by local hospital guidelines. It should be an empirical antibiotic given intravenously. There are usually recommendations for treating ‘sepsis of unknown cause’ if the site of infection is unknown.
Three out
A minimum of two sets of blood cultures should be taken. Ideally, this should happen prior to administration of antibiotics though they should not be a cause for delay. Serum lactate should be obtained normally via a blood gas (arterial or venous) to help assess the patient’s status. Urine output should be measured ideally with a catheter with a careful fluid balance recorded.
Additional investigations
In addition to the SEPSIS-6 bundle, patients should undergo investigations to look for organ dysfunction and the suspected source of infection. When thinking about a source of infection, not all of these investigations will be required if the source is obvious from the history and clinical assessment.
- Organ dysfunction: Full blood count, U&E, CRP, Clotting screen, liver function tests, ongoing observations
- Source of infection: Chest x-ray (chest), urine MC&S (urine), CT abdomen/pelvis (Intrabdominal pathology), lumbar puncture (meningitis), blood film (malaria), joint aspiration (septic arthritis)
Senior review
All patients with sepsis should be discussed with a senior clinician and have ongoing monitoring. NICE guidelines NG51 recommend that all patients presenting with ≥1 high-risk criteria should be discussed with a consultant. If there is any deterioration or features of septic shock/MODS, patients should be discussed and reviewed by the intensive care team.
