Introduction
Erythema nodosum (EN) is a panniculitis that presents with tender raised nodules that typically develop over the anterior shins.
It is thought to occur due to a delayed hypersensitivity reaction that results in a panniculitis (inflammation of the subcutaneous fat). It is idiopathic in 30-50% of cases with the remainder occurring secondary to a wide variety of triggers.
EN typically self-resolves over a few weeks though NSAIDs (in the absence of contraindications) are often given for symptomatic relief and may aid resolution. It is important to try and establish any underlying disorder that may exist.
Epidemiology
EN most commonly presents in women aged 20-40.
Following puberty women are affected 3-6 times more than men. It can occur at any age and in all ethnicities.
Aetiology
EN is idiopathic in an estimated 30-50% of patients.
Though no cause is found in 30-50% of patients, in the remainder EN is associated with a number of different infections, inflammatory conditions and malignancies. There are also several drugs that can trigger it.
Identified causes of EN include:
- Infections:
- Bacterial infection, includes:
- Streptococcal infection (most common)
- Tuberculosis
- Viral infection, includes:
- Hepatitis B
- HIV
- Fungal infections
- Parasitic infection
- Bacterial infection, includes:
- Inflammatory bowel disease:
- Crohn’s disease
- Ulcerative colitis
- Malignancy:
- Hodgkin’s lymphoma
- AML
- Others
- Others:
- Sarcoidosis
- Pregnancy
- Medications (e.g. contraceptive pills, penicillins, sulfonamide)
Clinical features
EN most commonly presents with an abrupt onset of tender, bilateral, raised, erythematous nodules on the legs.
EN may develop after a prodrome or pre-eruptive phase. This is characterised by fever, arthralgia and malaise.
Tender lesions, around 2-5cm, develop over the shins and lower legs though occasionally they will affect the upper body. Systemic symptoms of fever, arthralgia and malaise may be experienced.
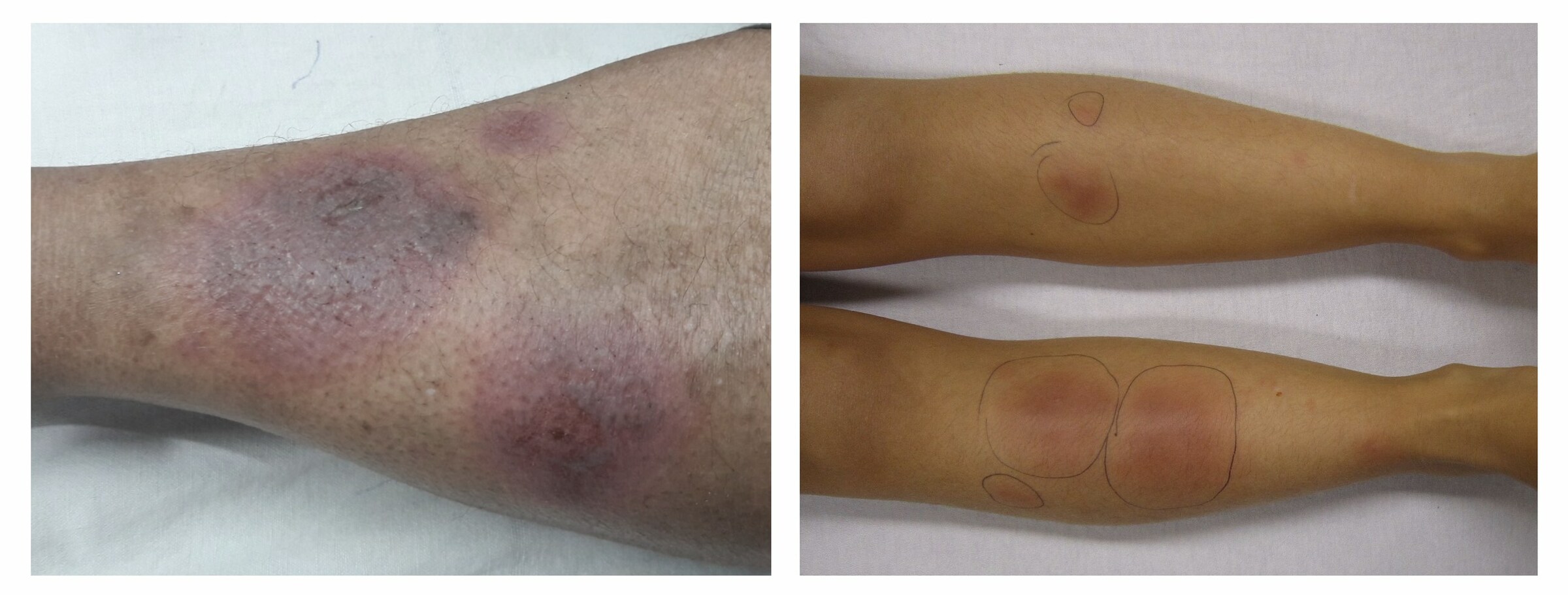
Erythema nodosum
Images courtesy of Medicalpal (left) and James Heilman (right)
Investigations
Investigations are important to identify any underlying cause of EN.
EN is normally a clinical diagnosis based on characteristic history and examination findings. Skin biopsy may be used in patients with atypical presentations.
Investigations aim to identify potential underlying causes. A thorough history (including medication review) and examination are both important.
Blood tests include ESR/CRP to look for signs of inflammation that may reflect an underlying infection or other inflammatory processes. An FBC should be ordered and the differential reviewed to look for signs of haematological malignancy.
A throat swab and antistreptolysin O titre (ASOT) can be used to give evidence of a recent Streptococcal infection.
A chest radiograph should be routinely performed. This may show evidence of potential causes including sarcoidosis, TB, lymphoma or a chest infection.
If there are signs of active TB these should be investigated. Otherwise, a Mantoux test and/or interferon-gamma release assay may be sent.
- Blood tests
- FBC
- ESR
- CRP
- ASOT
- Chest X-ray
- TB:
- Mantoux test
- Inteferon-gamma release assay
Further investigations may be indicated depending on the given history and patient factors.
Management
Treatment of EN typically involves NSAIDs and rest.
Most cases will resolve spontaneously after a few weeks. Medications like NSAIDs help with symptoms and may hasten resolution. Treatment options include:
- General measures: rest is advised, particularly in patients with systemic symptoms. Leg elevation may help.
- Compression stockings: low-grade compression stockings may be used if pain allows.
- NSAIDs: in patients without contraindications (e.g. history of gastric ulcers) NSAIDs provide symptomatic relief and can help to accelerate the resolution of EN.
- Potassium iodide: not widely available but can lead to rapid resolution of EN.
Second-line options in patients with severe disease or requiring quick resolution include systemic corticosteroids. Other immunosuppressants may be used particularly in patients with chronic or recurrent disease.
In cases where an underlying cause is identified and requires further management, a referral should be made to the relevant specialty for further review.
