Sinus blockade
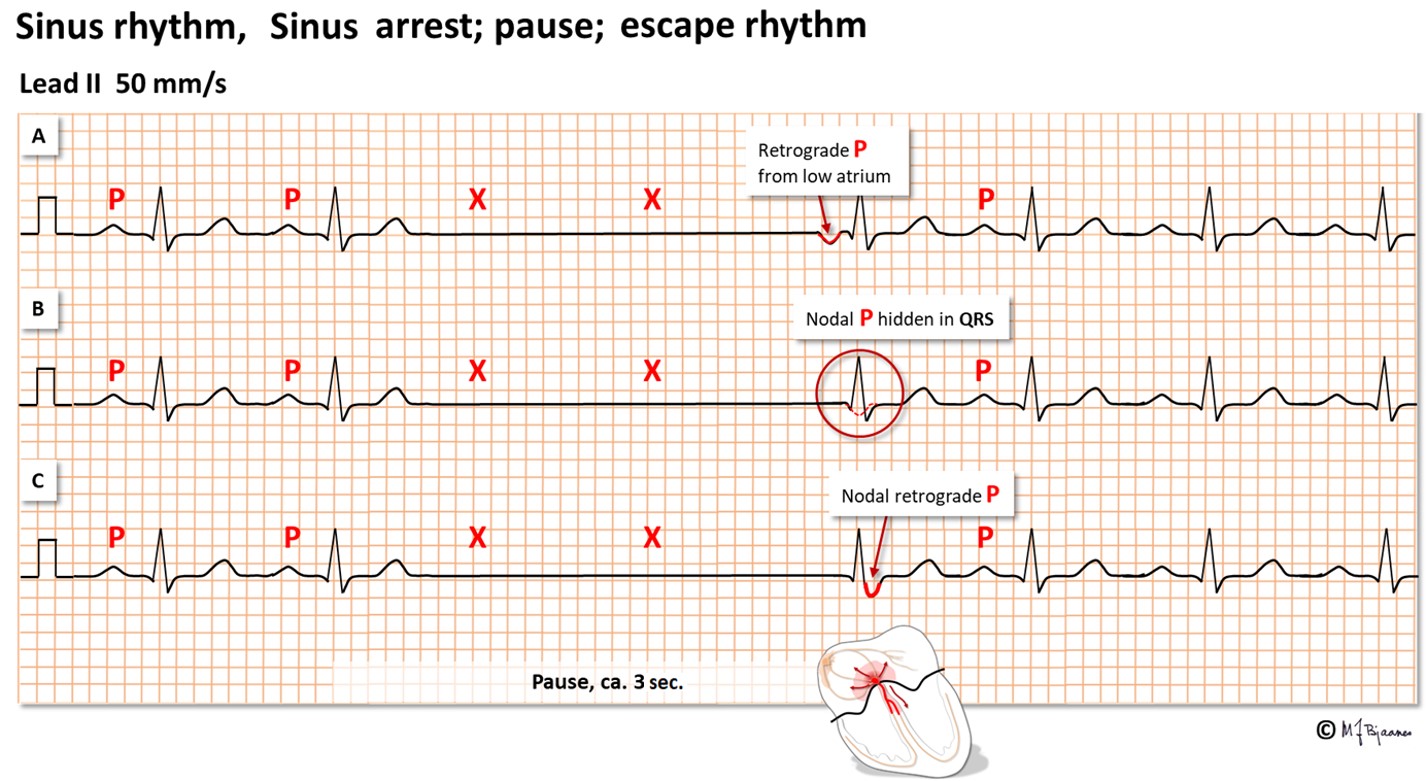
The normal heart beat starts in the sinus node that contains the fastest pacemaker cells. If no impulse should reach the atrium, and no atrial rescue impulse appears, there will be a pause without any P wave. The pause – sinus arrest – may be brief or long. When a pause exceeds 3-5 seconds, the patient may experience dizziness or a fainting spell. Usually, the normal rhythm soon recovers, and the patient immediately feels well.
Important notes :
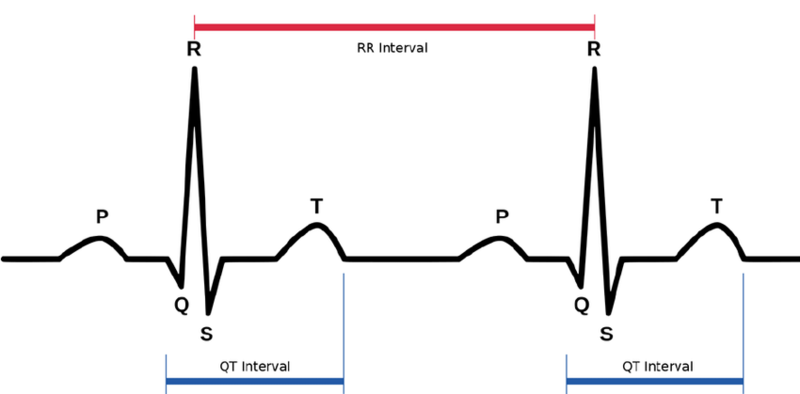
» If the speed is 50 mm/sec;
1 mm = 0.02 sec
» If the speed is 25 mm/sec;
1 mm = 0.04 sec
» Normal HR : 60 : 90 beats per minute
» Normal QRS complex duration = 0.06-0.10 sec.
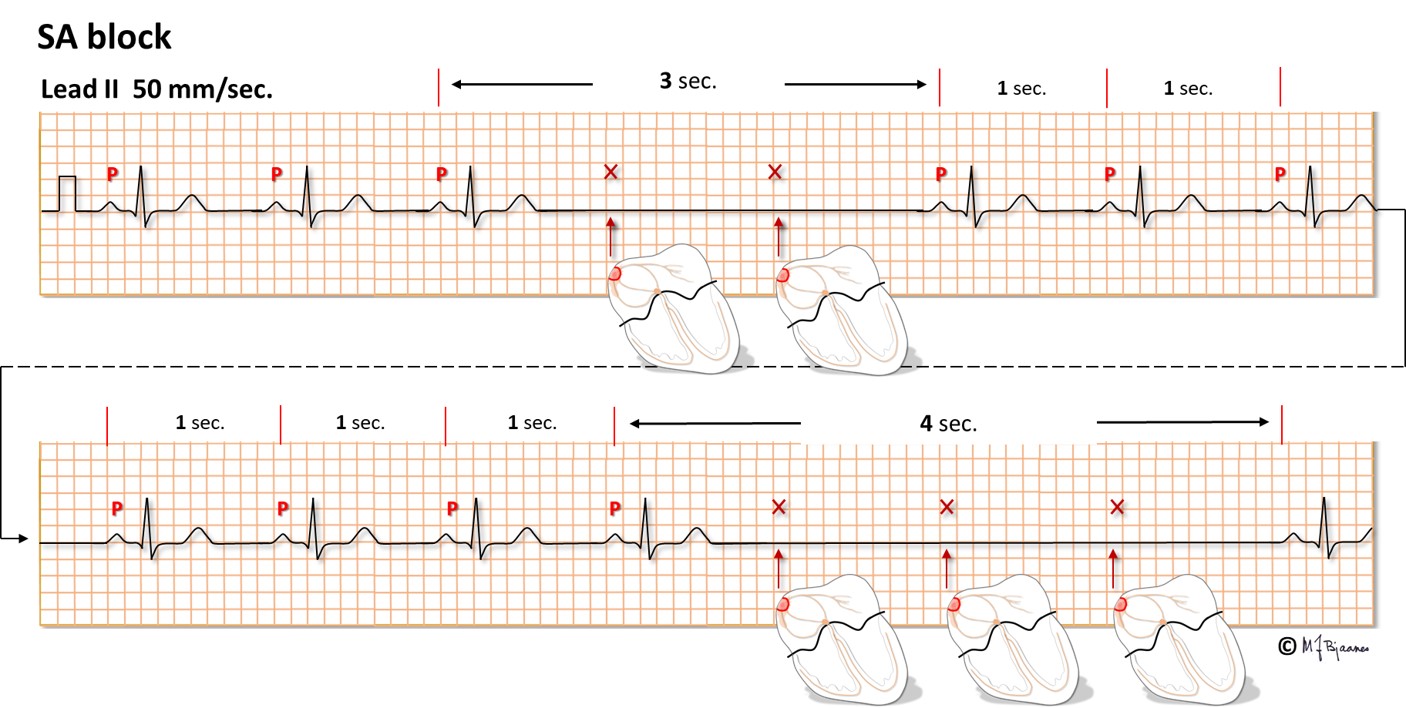
Sinoatrial blockade
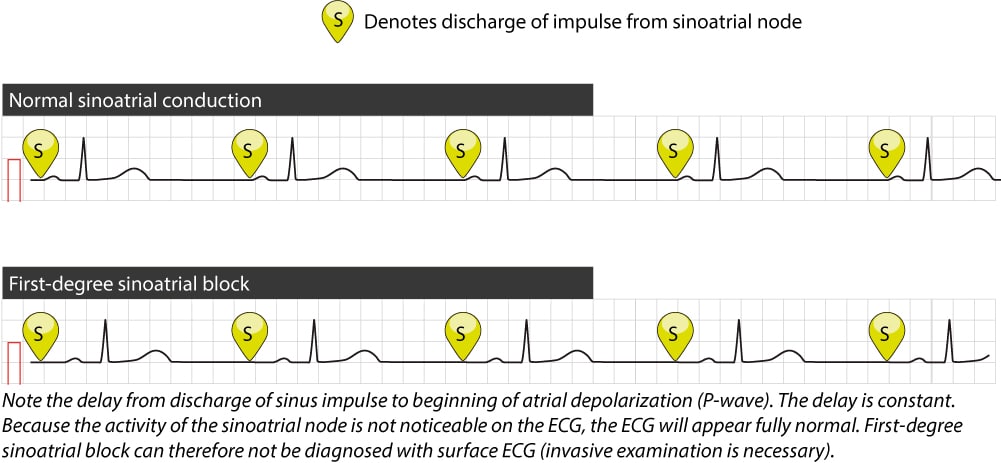
1st Degree
» First degree sinoatrial exit block is due to delayed transmission of an impulse from the sinoatrial node, and is not detectable on ECG.
2nd Degree
» Loss of one or more P waves.
» There are 2 types :
Type I
» Periodicals of Samoilov-Wenckebach. The loss of P wave is preceded by a shortening of the P-P intervals.
» The duration of the pause with the loss of the P wave is less than the doubled P-P interva
Look For : Progressively shortened PP intervals, followed by a pause.

Type II
» Loss of one or more P waves, as a result of which pauses appear equal to 2 or 3 P-P intervals
Look For :
A constant PP interval, with a pause that is a multiple of the PP interval.
3rd Degree
» Complete sinoatrial blockade: not a single impulse from the sinus node is conducted to the atria.
» Not diagnosed by ECG
Look For :
» Complete lack of P waves
» An escape rhythm may be present
Atrioventricular blockade
Slowing down or stopping the conduction of the impulse from the atria to the ventricles
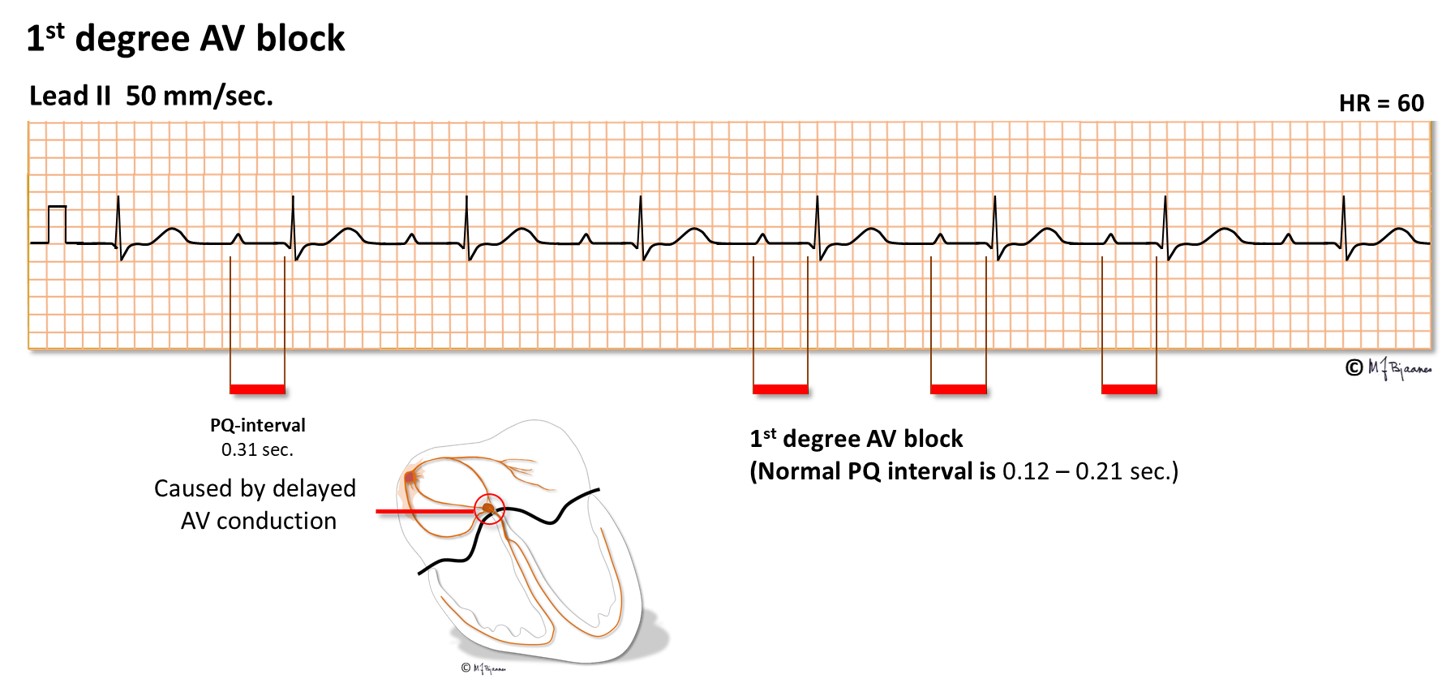
1st Degree
PQ lengthening more than 0.2 s. All impulses from the atria to the ventricles are conducted
Look For :
Prolonged PR interval >200ms (5mm).
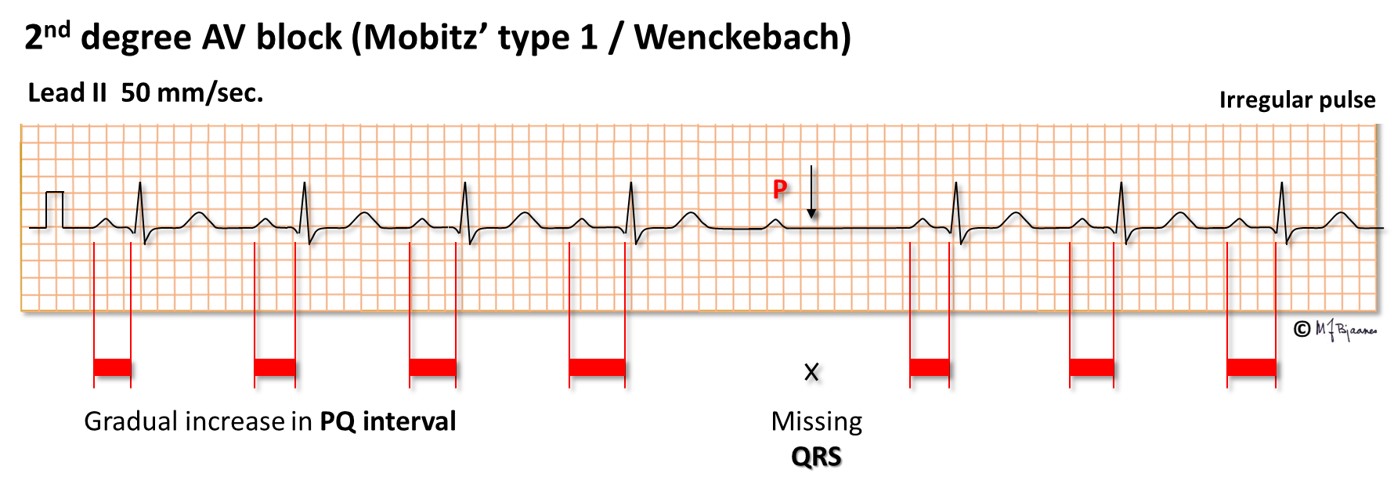
2nd Degree
» Incomplete AV block. Some of the impulses from the atria are not conducted to the ventricles
» There are 2 types :
Type I – Mobitz I
» Periodicals of Samoilov-Wenckebach. Proximal type of blockade. Gradual increase in PQ followed by loss of QRS
Look For : Initial normal PR interval with progressive prolongation of
PR interval followed by a dropped QRS complex.
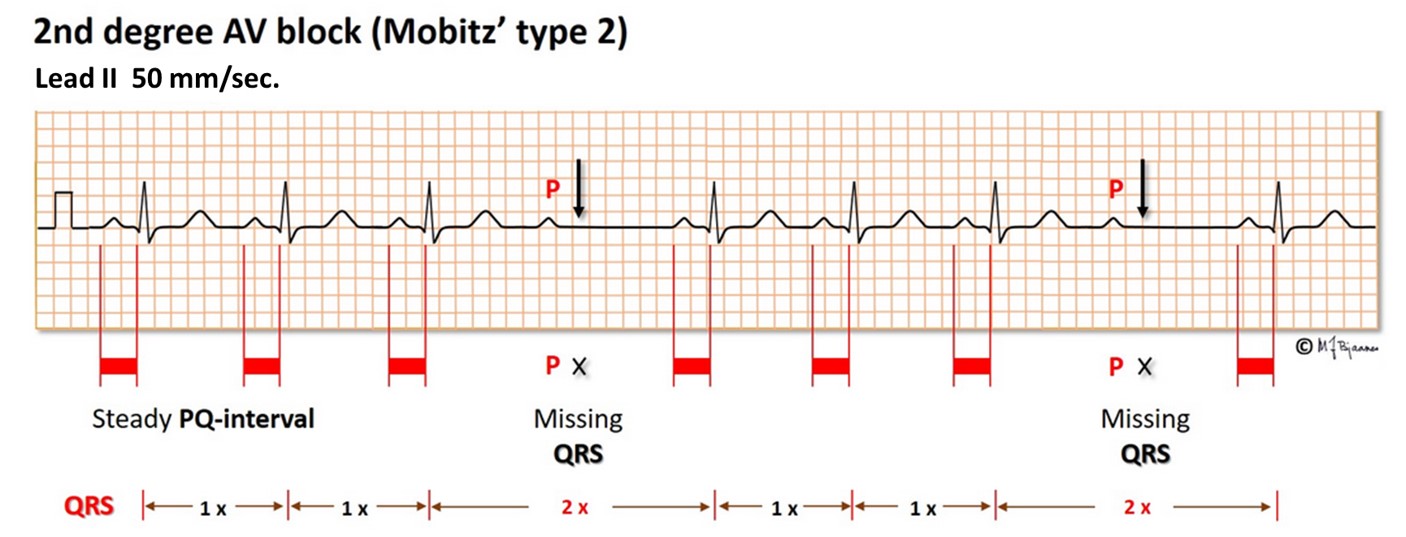
Type II – Mobitz II
» Distal blockade: prolapse of the ventricular complex without previous PQ lengthening
Look For :
Constant PR interval with intermittently dropped QRS complexes.
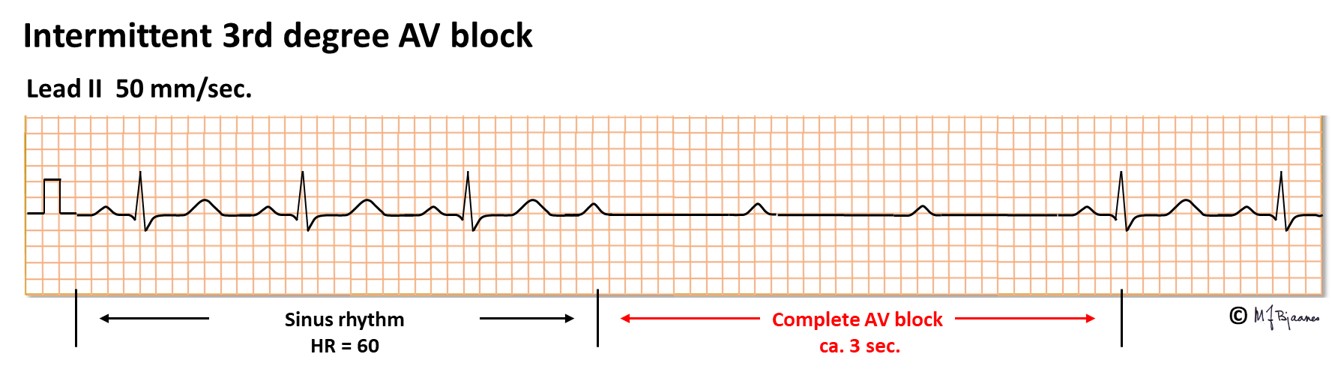
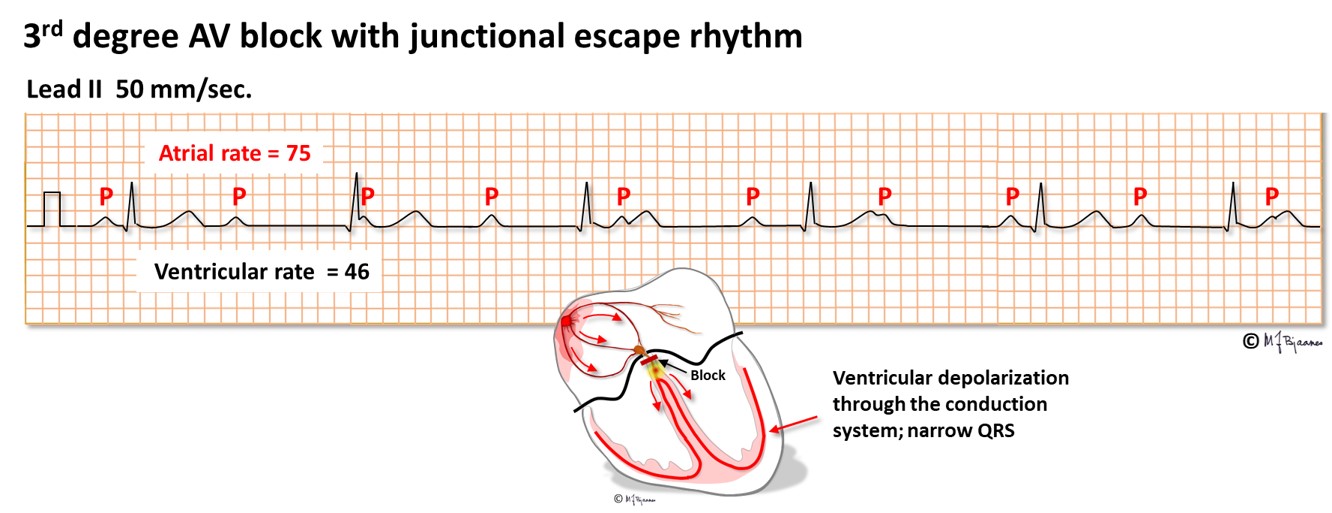
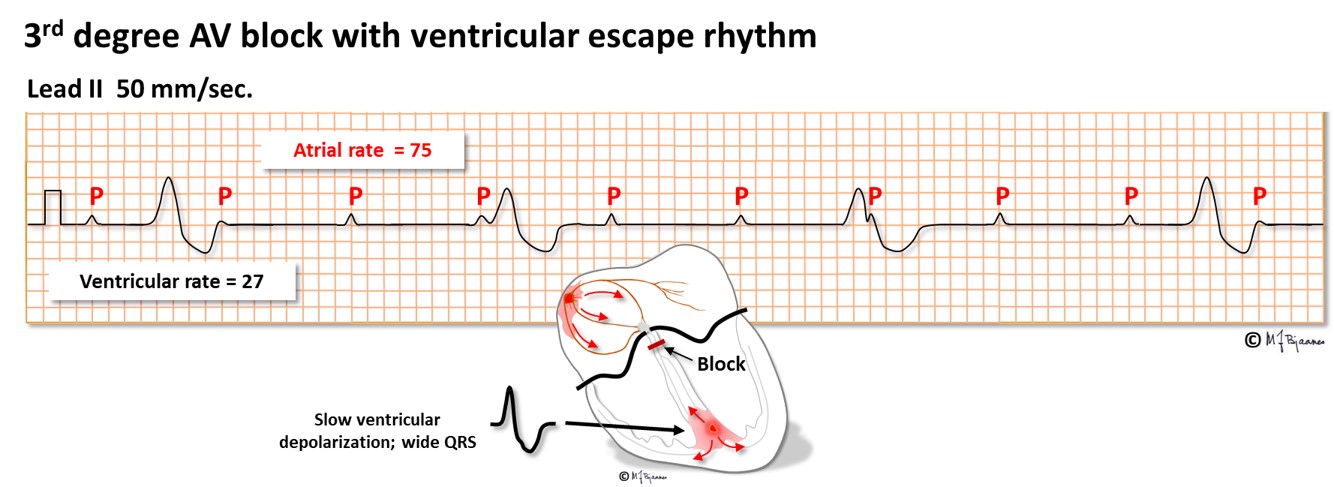
3rd Degree – Complete AV block
» Complete transverse block. There is no regularity in the relationship between P and QRS
» P & QRS are independent of each other
Look For : Complete dissociation of P waves and QRS complexes.
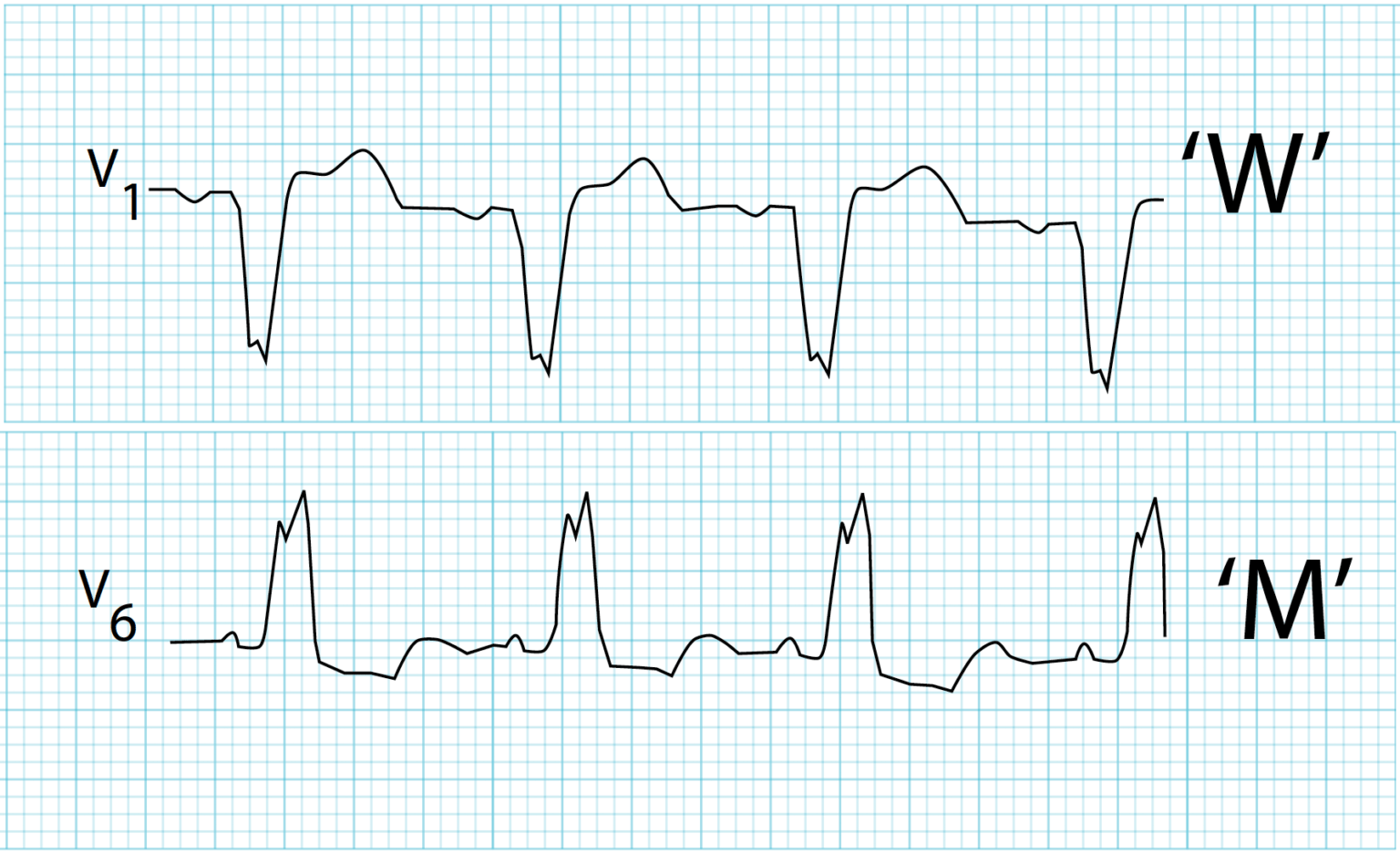
Bundle Branch Block – BBB
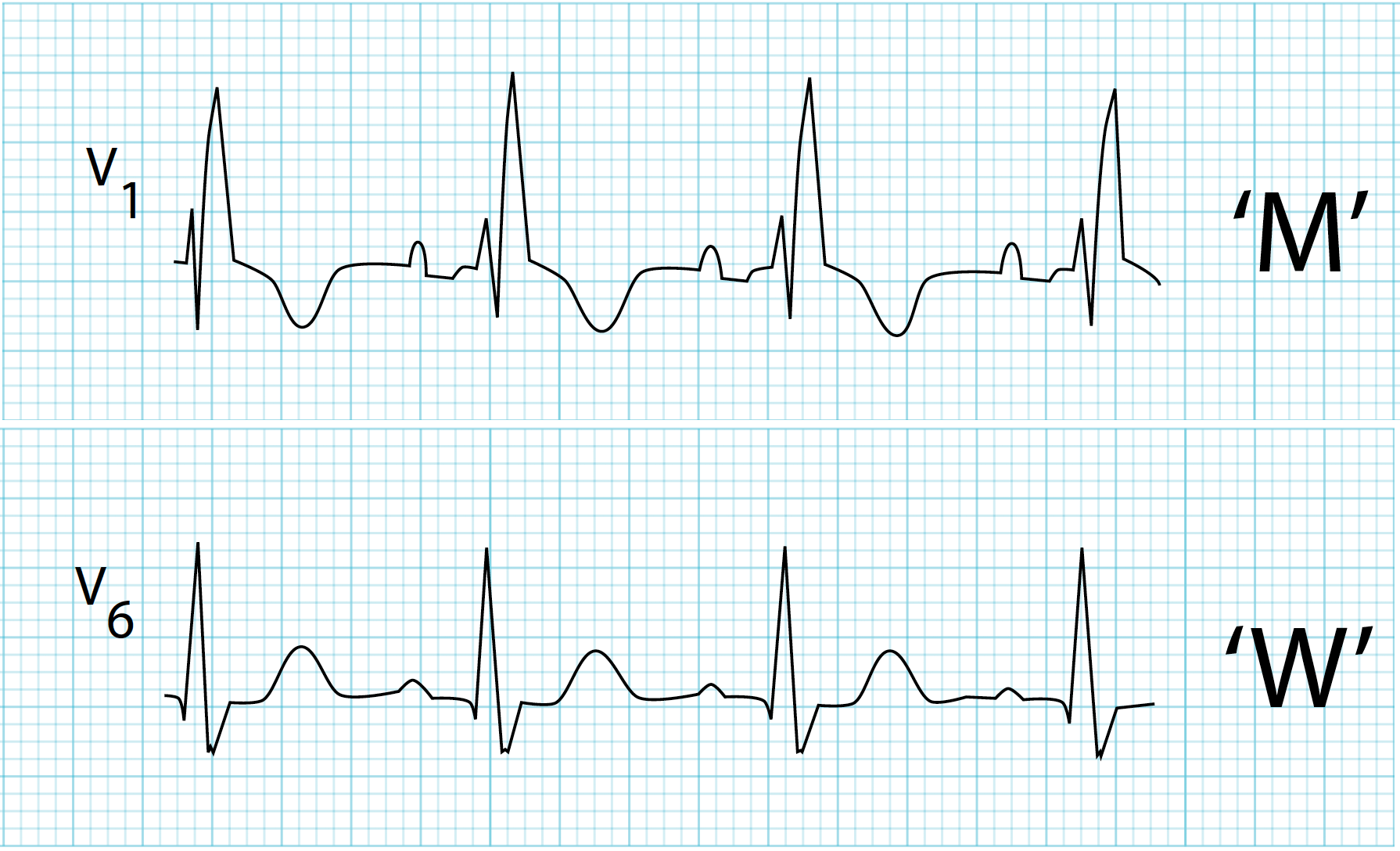
Right Bundle Branch Block – RBBB
» Changes in V1 and V2: rSR, RSR, rSr, rRs.
» The time of internal deviation is 0.06-0.08 (at a rate of 0.03).
» These changes are usually associated with ST depression and negative T.
» In the left chest leads – wide, with a rounded apex, often shallow S.
» If the QRS width is no more than 0.12 sec, then the right branch blockade is incomplete. If more than 0.12 sec, then its complete RBBB

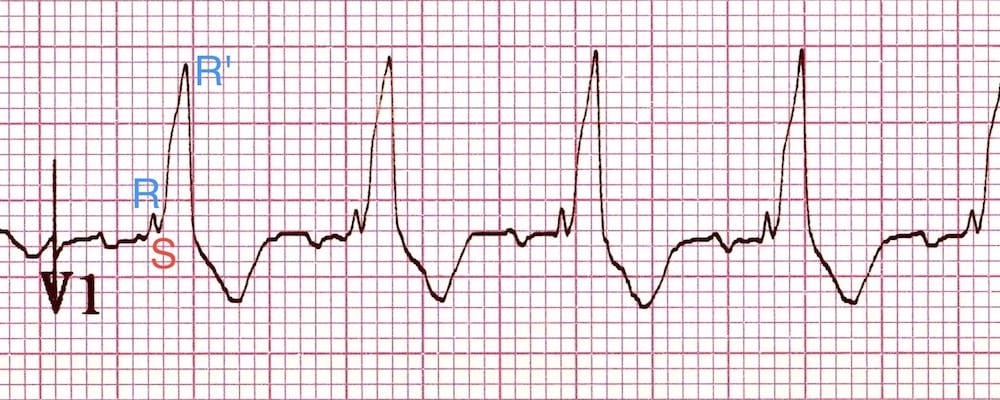

Left Bundle Branch Block – LBBB
» High, wide, deformed QRS complexes in I, aVL, V5-V6.
» The internal deviation time in V5 – V6 is greater than 0.05.
» These changes are usually associated with ST depression and negative T.
» In III, aVF, V1-V2, the ventricular complexes look like rS or QS, ST is displaced upward.
» If the QRS width is no more than 0.12 s, then the left branch block is incomplete.
» If more than 0.12 sec, then its complete LBBB



RA : Right Atrium
LA : Left Atrium
RV : Right Ventricle
LV : Left Ventricle
RCA : Right coronary artery
Rt : Right
Lt : Left
mv : Milli volt
MI : Myocardial Infarction
bpm : beat per minute
LI : Lead 1
LII : Lead 2
LIII : Lead 3
LAD : Left anterior descending coronary artery
aVR : Augmented Voltage on Right arm
aVL : Augmented Voltage on Left arm
aVF : Augmented Voltage on Foot
Lcx : Left circumflex coronary artery



