Background
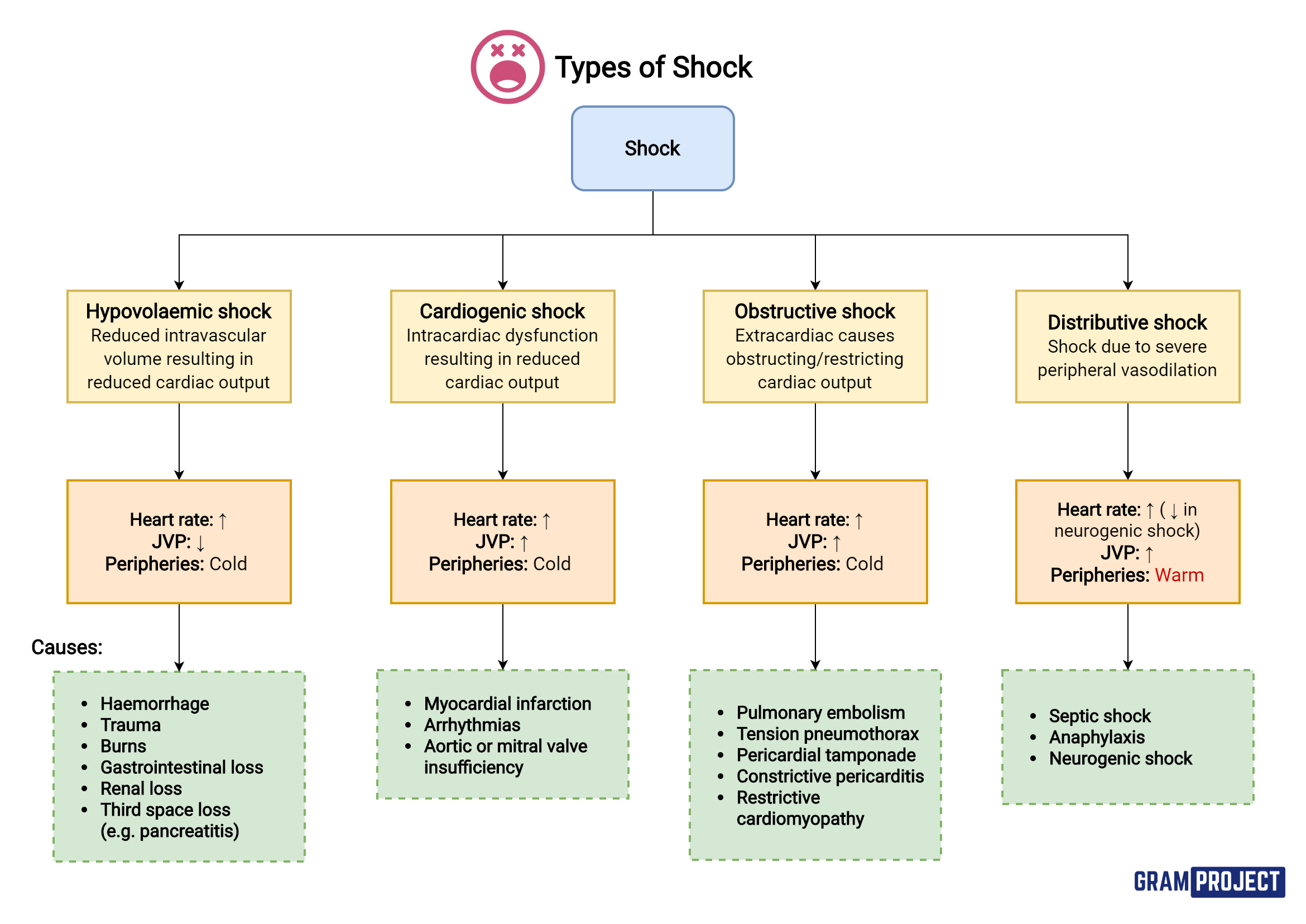
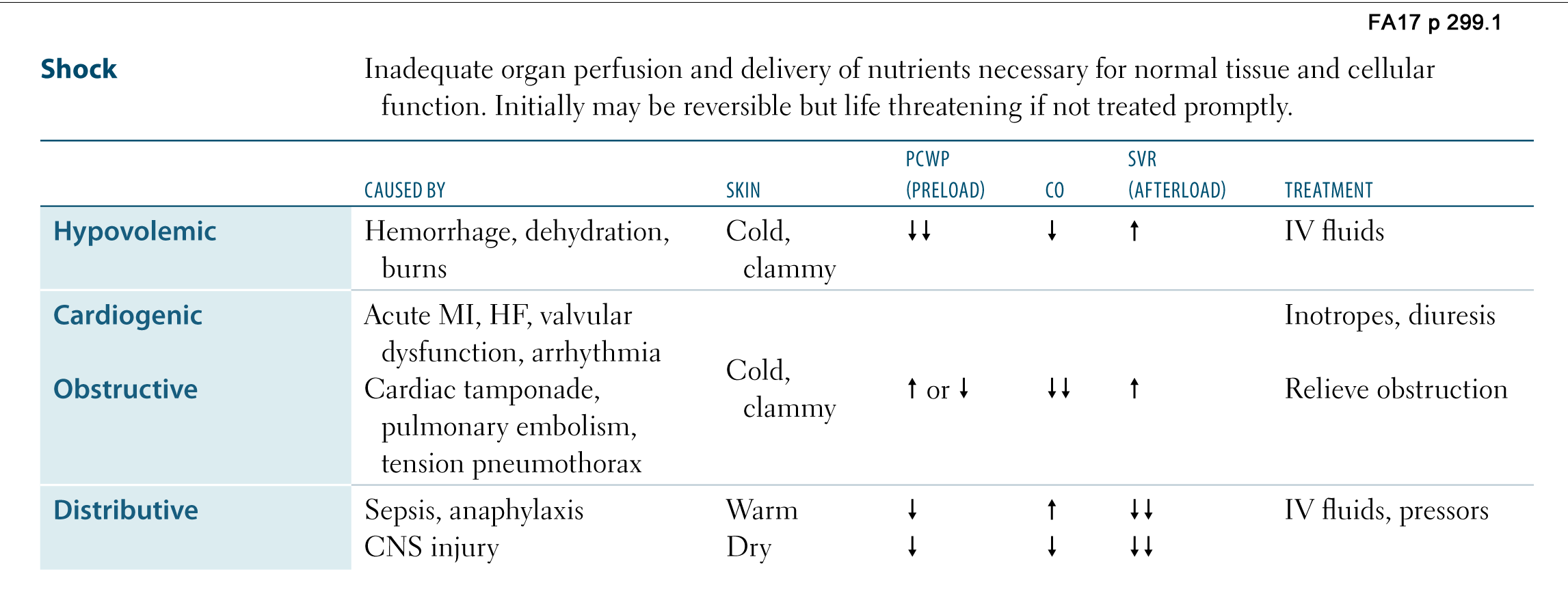
Hypovolemic shock refers to a medical or surgical condition in which rapid fluid loss results in multiple organ failure due to inadequate circulating volume and subsequent inadequate perfusion.
Endothelium plays a critical role in vascular physiological, pathophysiological, and reparative processes. The functions of the endothelium are highly altered following hypovolemic shock due to ischemia of the endothelial cells and by reperfusion due to resuscitation with fluids. Due to oxygen deprivation, endothelial cell apoptosis is induced following hypovolemic shock.
Most often, hypovolemic shock is secondary to rapid blood loss (hemorrhagic shock).
Acute external blood loss secondary to penetrating trauma and severe GI bleeding disorders are 2 common causes of hemorrhagic shock. Hemorrhagic shock can also result from significant acute internal blood loss into the thoracic and abdominal cavities.
Two common causes of rapid internal blood loss are solid organ injury and rupture of an abdominal aortic aneurysm. Hypovolemic shock can result from significant fluid (other than blood) loss. Two examples of hypovolemic shock secondary to fluid loss include refractory gastroenteritis and extensive burns. The remainder of this article concentrates mainly on hypovolemic shock secondary to blood loss and the controversies surrounding the treatment of this condition. The reader is referred to other articles for discussions of the pathophysiology and treatment for hypovolemic shock resulting from losses of fluid other than blood.
The many life-threatening injuries experienced during the wars of the 1900s have significantly affected the development of the principles of hemorrhagic shock resuscitation. During World War I, W.B. Cannon recommended delaying fluid resuscitation until the cause of the hemorrhagic shock was repaired surgically. Crystalloids and blood were used extensively during World War II for the treatment of patients in unstable conditions. Experience from the Korean and Vietnam wars revealed that volume resuscitation and early surgical intervention were paramount for surviving traumatic injuries resulting in hemorrhagic shock. These and other principles helped in the development of present guidelines for the treatment of traumatic hemorrhagic shock. However, recent investigators have questioned these guidelines, and today, controversies exist concerning the optimal treatment of hemorrhagic shock.
The prognosis is dependent on the degree of volume loss.
Pathophysiology
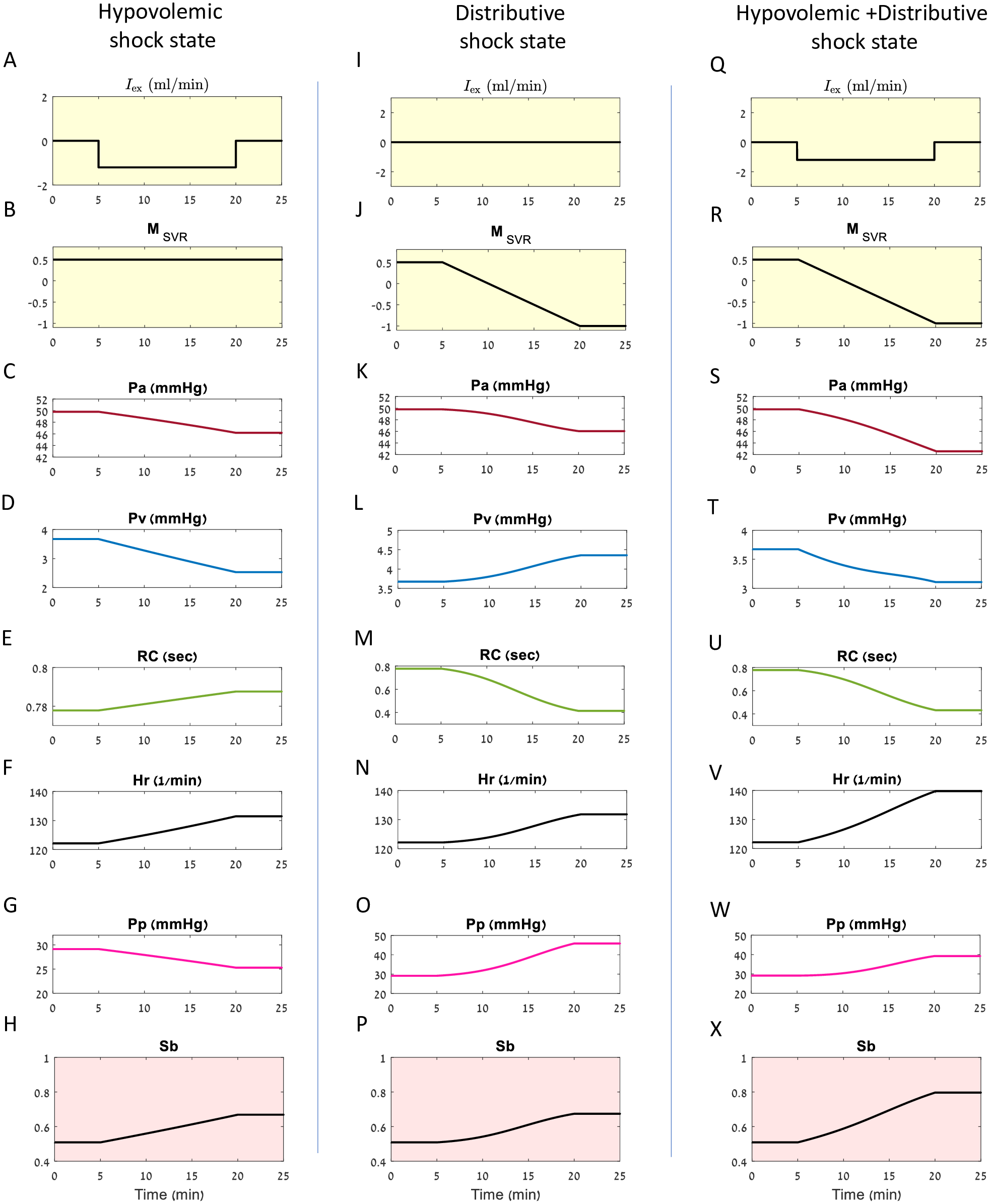
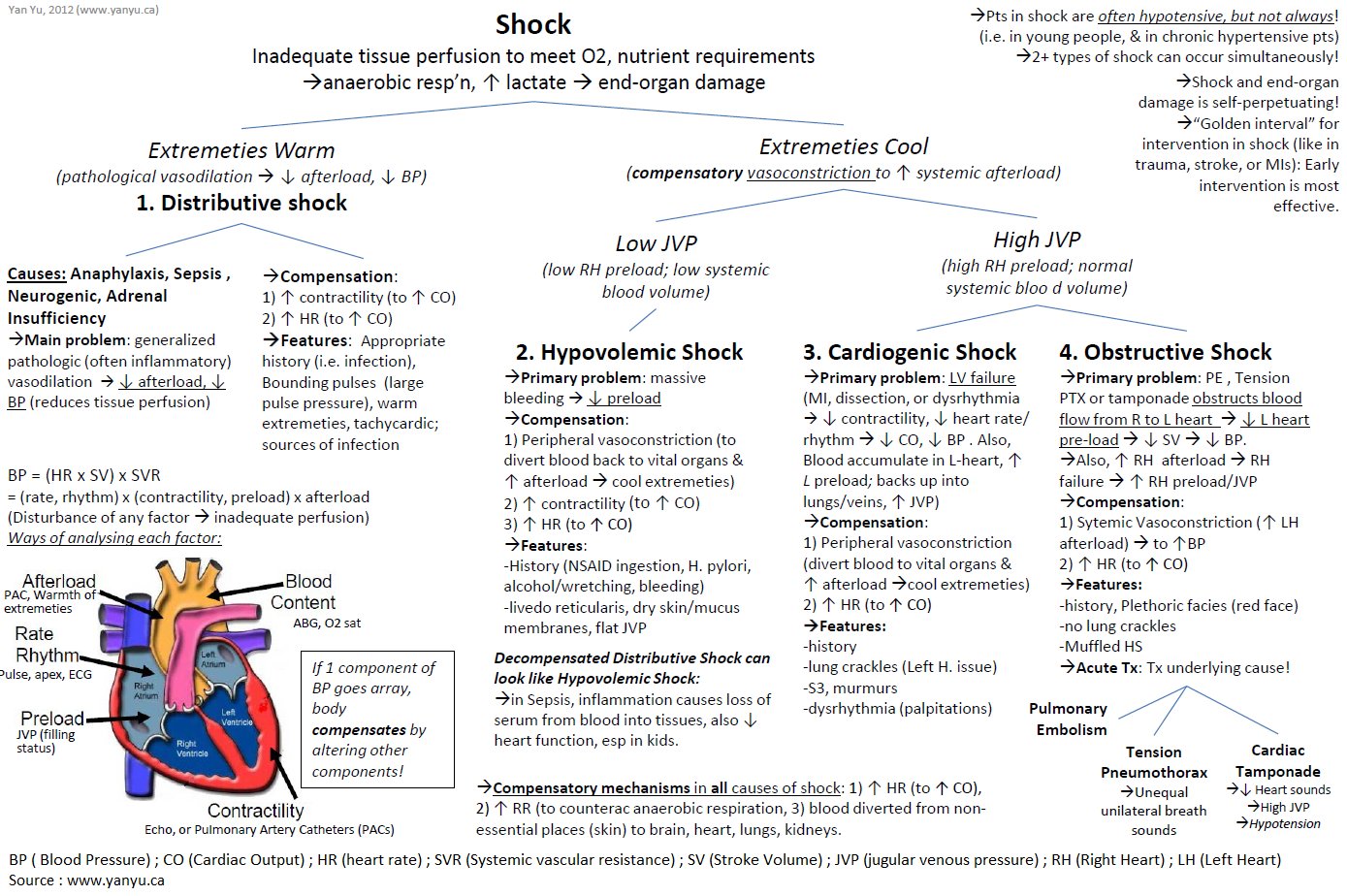
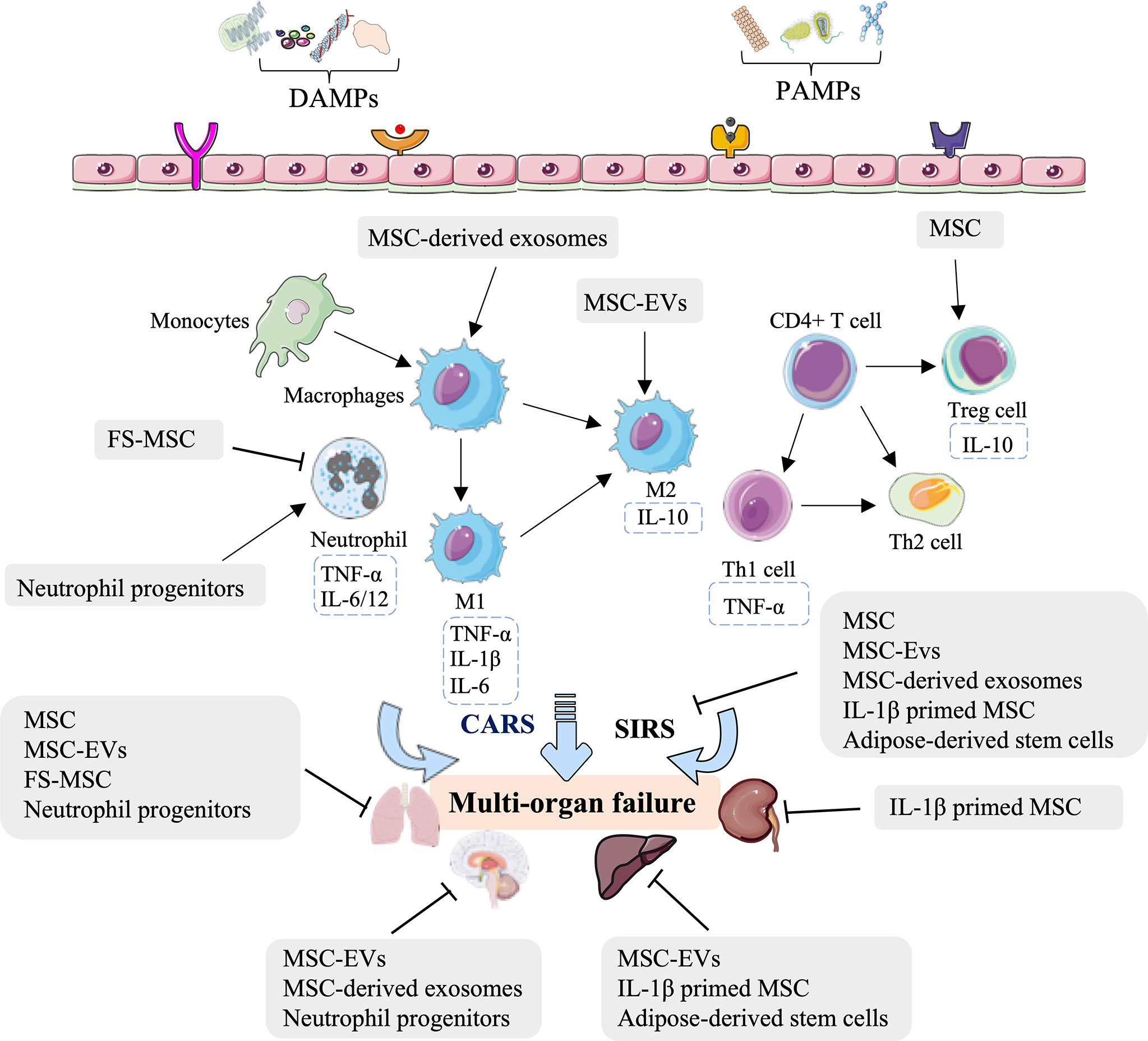
The human body responds to acute hemorrhage by activating the following major physiologic systems: the hematologic, cardiovascular, renal, and neuroendocrine systems.
The hematologic system responds to an acute severe blood loss by activating the coagulation cascade and contracting the bleeding vessels (by means of local thromboxane A2 release). In addition, platelets are activated (also by means of local thromboxane A2 release) and form an immature clot on the bleeding source. The damaged vessel exposes collagen, which subsequently causes fibrin deposition and stabilization of the clot. Approximately 24 hours are needed for complete clot fibrination and mature formation.
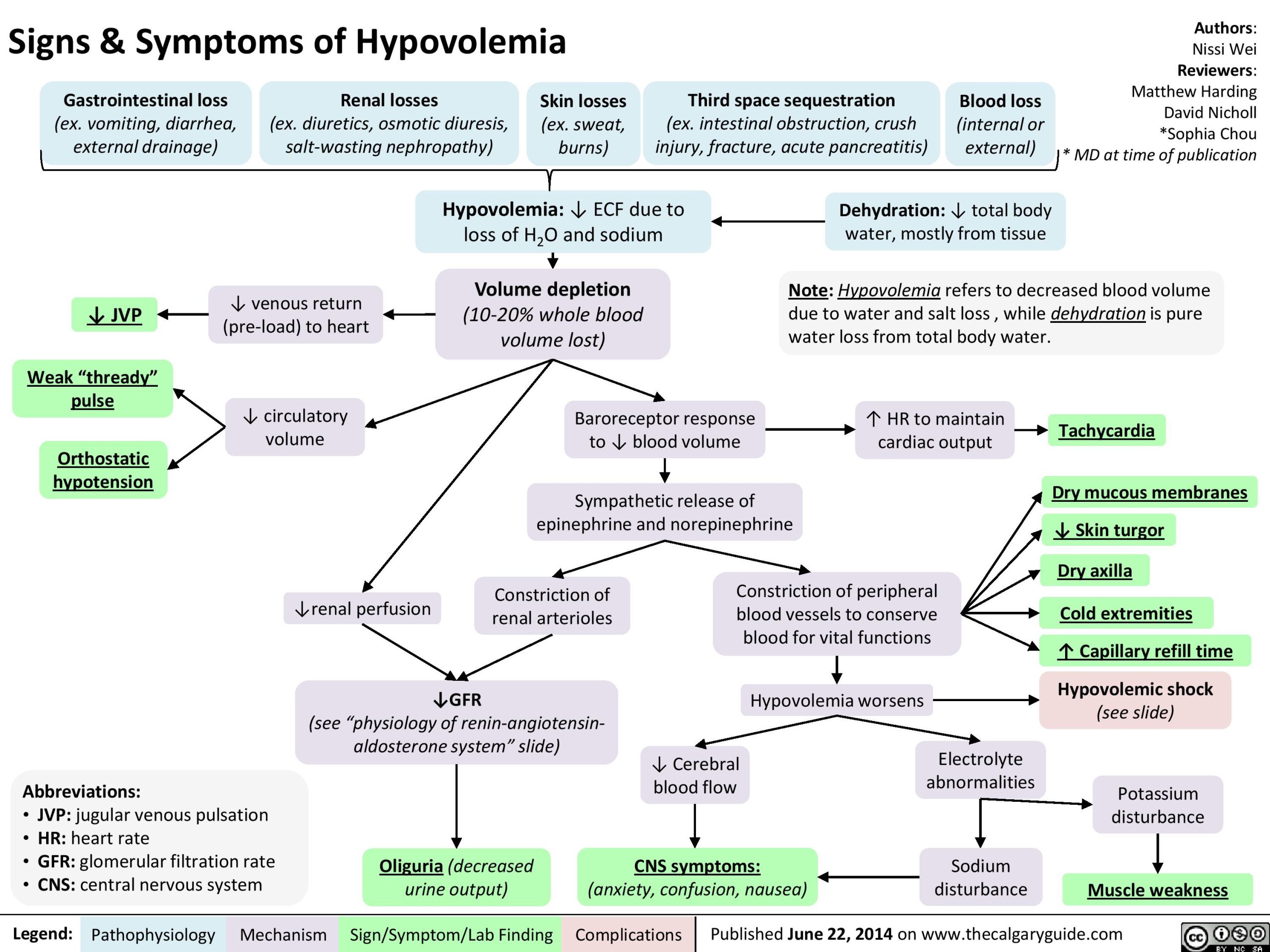
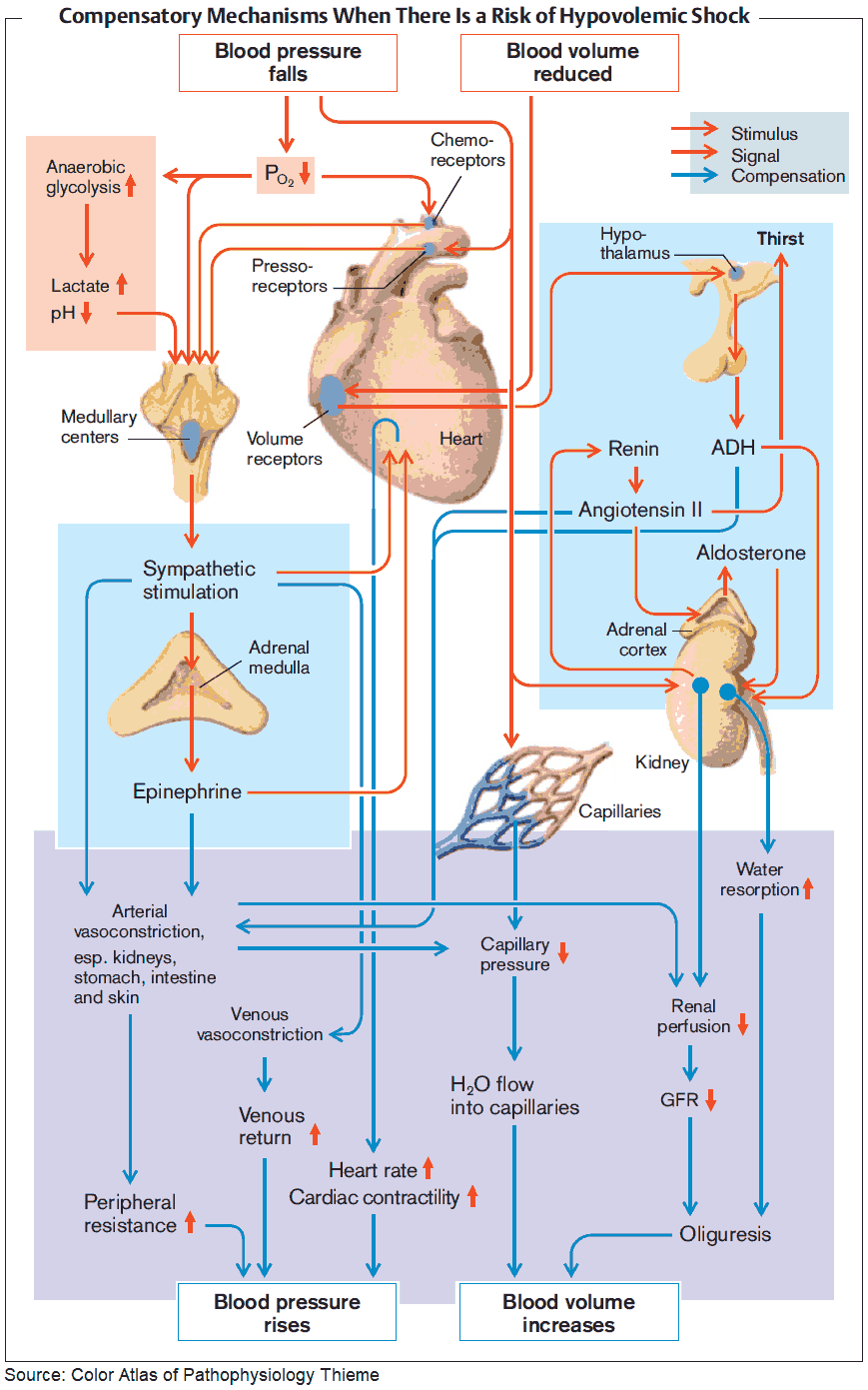
The cardiovascular system initially responds to hypovolemic shock by increasing the heart rate, increasing myocardial contractility, and constricting peripheral blood vessels. This response occurs secondary to an increased release of norepinephrine and decreased baseline vagal tone (regulated by the baroreceptors in the carotid arch, aortic arch, left atrium, and pulmonary vessels). The cardiovascular system also responds by redistributing blood to the brain, heart, and kidneys and away from skin, muscle, and GI tract.
The renal system responds to hemorrhagic shock by stimulating an increase in renin secretion from the juxtaglomerular apparatus. Renin converts angiotensinogen to angiotensin I, which subsequently is converted to angiotensin II by the lungs and liver. Angiotensin II has 2 main effects, both of which help to reverse hemorrhagic shock, vasoconstriction of arteriolar smooth muscle, and stimulation of aldosterone secretion by the adrenal cortex. Aldosterone is responsible for active sodium reabsorption and subsequent water conservation.
The neuroendocrine system responds to hemorrhagic shock by causing an increase in circulating antidiuretic hormone (ADH). ADH is released from the posterior pituitary gland in response to a decrease in BP (as detected by baroreceptors) and a decrease in the sodium concentration (as detected by osmoreceptors). ADH indirectly leads to an increased reabsorption of water and salt (NaCl) by the distal tubule, the collecting ducts, and the loop of Henle.
The pathophysiology of hypovolemic shock is much more involved than what was just listed. To explore the pathophysiology in more detail, references for further reading are provided in the bibliography. These intricate mechanisms list above are effective in maintaining vital organ perfusion in severe blood loss. Without fluid and blood resuscitation and/or correction of the underlying pathology causing the hemorrhage, cardiac perfusion eventually diminishes, and multiple organ failure soon follows.
History
In a patient with possible shock secondary to hypovolemia, the history is vital in determining the possible causes and in directing the workup. Hypovolemic shock secondary to external blood loss typically is obvious and easily diagnosed. Internal bleeding may not be as obvious as patients may complain only of weakness, lethargy, or a change in mental status.
Symptoms of shock, such as weakness, lightheadedness, and confusion, should be assessed in all patients.
In the patient with trauma, determine the mechanism of injury and any information that may heighten suspicion of certain injuries (eg, steering wheel damage or extensive passenger compartment intrusion in a motor vehicle accident).
If conscious, the patient may be able to indicate the location of pain.
Vital signs, prior to arrival in the ED, should also be noted.
Chest, abdominal, or back pain may indicate a vascular disorder.
The classic sign of a thoracic aneurysm is a tearing pain radiating to the back. Abdominal aortic aneurysms usually result in abdominal, back pain, or flank pain.
In patients with GI bleeding, inquiry about hematemesis, melena, alcohol drinking history, excessive nonsteroidal anti-inflammatory drug use, and coagulopathies (iatrogenic or otherwise) is very important. The chronology of vomiting and hematemesis should be determined. The patient who presents with hematemesis after multiple episodes of forceful vomiting is more likely to have Boerhaave syndrome or a Mallory-Weiss tear, whereas a patient with a history of hematemesis from the start is more likely to have peptic ulcer disease or esophageal varices.
If a gynecologic cause is being considered, gather information about the following: last menstrual period, risk factors for ectopic pregnancy, vaginal bleeding (including amount and duration), vaginal passage of products of conception, and pain. All women of childbearing age should undergo a pregnancy test, regardless of whether they believe that they are pregnant. A negative pregnancy test typically excludes ectopic pregnancy as a diagnosis.
Physical
The physical examination should always begin with an assessment of the airway, breathing, and circulation. Once these have been evaluated and stabilized, the circulatory system should be evaluated for signs and symptoms of shock.
Do not rely on systolic BP as the main indicator of shock; this practice results in delayed diagnosis. Compensatory mechanisms prevent a significant decrease in systolic BP until the patient has lost 30% of the blood volume. More attention should be paid to the pulse, respiratory rate, and skin perfusion. Also, patients taking beta-blockers may not present with tachycardia, regardless of the degree of shock.
Classes of hemorrhage have been defined, based on the percentage of blood volume loss. However, the distinction between these classes in the hypovolemic patient often is less apparent. Treatment should be aggressive and directed more by response to therapy than by initial classification.
Class I hemorrhage (loss of 0-15%)
In the absence of complications, only minimal tachycardia is seen. Usually, no changes in BP, pulse pressure, or respiratory rate occur.
A delay in capillary refill of longer than 3 seconds corresponds to a volume loss of approximately 10%.
Class II hemorrhage (loss of 15-30%)
Clinical symptoms include tachycardia (rate >100 beats per minute), tachypnea, decrease in pulse pressure, cool clammy skin, delayed capillary refill, and slight anxiety.
The decrease in pulse pressure is a result of increased catecholamine levels, which causes an increase in peripheral vascular resistance and a subsequent increase in the diastolic BP.
Class III hemorrhage (loss of 30-40%)
By this point, patients usually have marked tachypnea and tachycardia, decreased systolic BP, oliguria, and significant changes in mental status, such as confusion or agitation.
In patients without other injuries or fluid losses, 30-40% is the smallest amount of blood loss that consistently causes a decrease in systolic BP.
Most of these patients require blood transfusions, but the decision to administer blood should be based on the initial response to fluids.
Class IV hemorrhage (loss of >40%)
Symptoms include the following: marked tachycardia, decreased systolic BP, narrowed pulse pressure (or immeasurable diastolic pressure), markedly decreased (or no) urinary output, depressed mental status (or loss of consciousness), and cold and pale skin.
This amount of hemorrhage is immediately life threatening.
Issues to consider
A study found substantial variability between blood loss and clinical signs. This study concluded that it was difficult to establish specific cutoff points for clinical signs that could be used as triggers for clinical interventions.
In the patient with trauma, hemorrhage usually is the presumed cause of shock. However, it must be distinguished from other causes of shock. These include cardiac tamponade (muffled heart tones, distended neck veins), tension pneumothorax (deviated trachea, unilaterally decreased breath sounds), and spinal cord injury (warm skin, lack of expected tachycardia, neurological deficits).
The 4 areas in which life-threatening hemorrhage can occur are as follows: chest, abdomen, thighs, and outside the body. Note the following:
The chest should be auscultated for decreased breath sounds, because life-threatening hemorrhage can occur from myocardial, vessel, or lung laceration.
The abdomen should be examined for tenderness or distension, which may indicate intraabdominal injury.
The thighs should be checked for deformities or enlargement (signs of femoral fracture and bleeding into the thigh).
The patient’s entire body should then be checked for other external bleeding.
In the patient without trauma, the majority of the hemorrhage is in the abdomen. The abdomen should be examined for tenderness, distension, or bruits. Look for evidence of an aortic aneurysm, peptic ulcer disease, or liver congestion. Also check for other signs of bruising or bleeding.
In the pregnant patient, perform a sterile speculum examination. However, with third-trimester bleeding, the examination should be performed as a “double set-up” in the operating room. Check for abdominal, uterine, or adnexal tenderness.
Causes
The causes of hemorrhagic shock are traumatic, vascular, GI, or pregnancy related, as follows:
Traumatic causes can result from penetrating and blunt trauma. Common traumatic injuries that can result in hemorrhagic shock include the following: myocardial laceration and rupture, major vessel laceration, solid abdominal organ injury, pelvic and femoral fractures, and scalp lacerations.
Vascular disorders that can result in significant blood loss include aneurysms, dissections, and arteriovenous malformations.
GI disorders that can result in hemorrhagic shock include the following: bleeding esophageal varices, bleeding peptic ulcers, Mallory-Weiss tears, and aortointestinal fistulas.
Pregnancy-related disorders include ruptured ectopic pregnancy, placenta previa, and abruption of the placenta. Hypovolemic shock secondary to an ectopic pregnancy is common. Hypovolemic shock secondary to an ectopic pregnancy in a patient with a negative urine pregnancy test is rare but has been reported.
Diagnostic Considerations
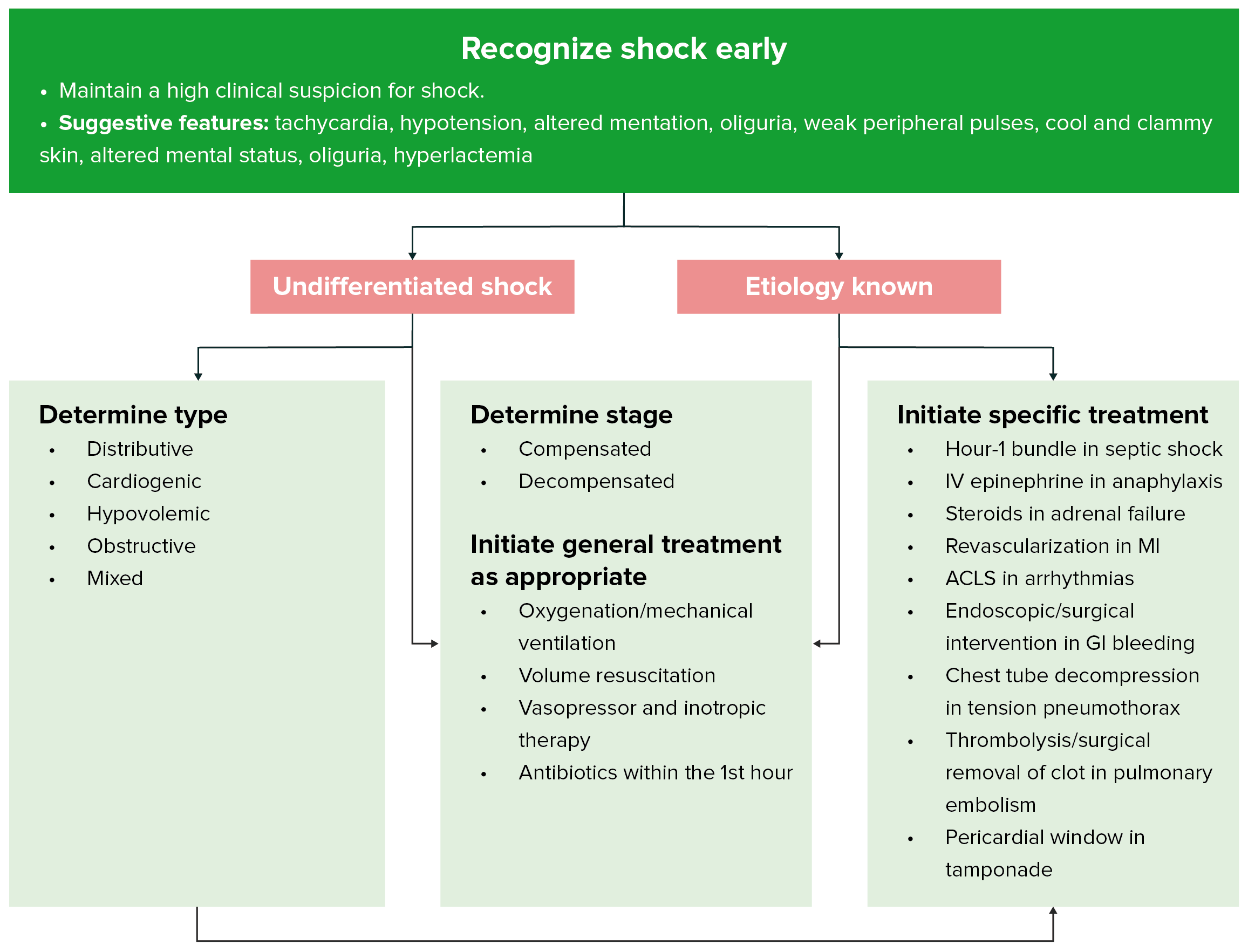
A common error in the management of hypovolemic shock is failure to recognize it early, often caused by a reliance on BP or initial hematocrit level, rather than signs of decreased peripheral perfusion, to make the diagnosis. This error leads to delay in diagnosing the cause and in resuscitating the patient.
Also note the following:
Injuries in patients with trauma can be missed, especially if the examiner focuses on more obvious injuries. This error can be avoided by completing a full physical examination, continuously and closely monitoring the patient’s status, and performing serial examinations.
Elderly individuals have less tolerance for hypovolemia compared with the rest of the general population. Aggressive therapy should be instituted early to prevent potential complications, such as myocardial infarction and stroke.
In patients who require extensive volume resuscitation, care should be taken to prevent hypothermia, because this can contribute to arrhythmia or coagulopathy. Hypothermia can be prevented by warming the intravenous fluids prior to their administration.
Patients taking beta-blockers or calcium-channel blockers and those with pacemakers may not have a tachycardic response to hypovolemia; this lack of response may lead to a delay in the diagnosis of shock. To minimize this potential delay, history taking should always include questioning about medications. The examiner should also rely on signs of decreased peripheral perfusion other than tachycardia.
Coagulopathies can occur in patients receiving large amounts of volume resuscitation. This is due to dilution of platelets and clotting factors but is rare within the first hour of resuscitation. Baseline coagulation studies should be drawn and should guide the administration of platelets and fresh frozen plasma.
Complications
Complications include neurologic sequelae and death.
Differential Diagnoses
Emergent Management of Abruptio Placentae
Emergent Management of Ectopic Pregnancy
Femoral Shaft Fractures in Emergency Medicine
Gastrointesting bleeding
Hemorrhagic Shock Management in the ED
Hypovolemic Shock
Iron Toxicity
Pelvic Fracture Management in the ED
Penetrating trauma
Peptic Ulcer Disease
Placenta Previa Imaging
Postpartum Hemorrhage in Emergency Medicine
Pregnancy Trauma
Thoracic Aneurysm
Laboratory Studies
After the history is taken and the physical examination is performed, further workup depends on the probable cause of the hypovolemia, as well as on the stability of the patient’s condition.
Initial laboratory studies should include analysis of the CBC, electrolyte levels (eg, Na, K, Cl, HCO3, BUN, creatinine, glucose levels), lactate, prothrombin time, activated partial thromboplastin time, ABGs, urinalysis (in patients with trauma), and a urine pregnancy test. Blood should be typed and cross-matched.
Imaging Studies
Patients with marked hypotension and/or unstable conditions must first be resuscitated adequately. This treatment takes precedence over imaging studies and may include immediate interventions and immediately taking the patient to the operating room.
The workup for the patient with trauma and signs and symptoms of hypovolemia is directed toward finding the source of blood loss.
The atraumatic patient with hypovolemic shock requires ultrasonographic examination in the ED if an abdominal aortic aneurysm is suspected. If GI bleeding is suspected, a nasogastric tube should be placed, and gastric lavage should be performed. An upright chest radiograph should be obtained if a perforated ulcer or Boerhaave syndrome is a possibility. Endoscopy can be performed (usually after the patient has been admitted) to further delineate the source of bleeding.
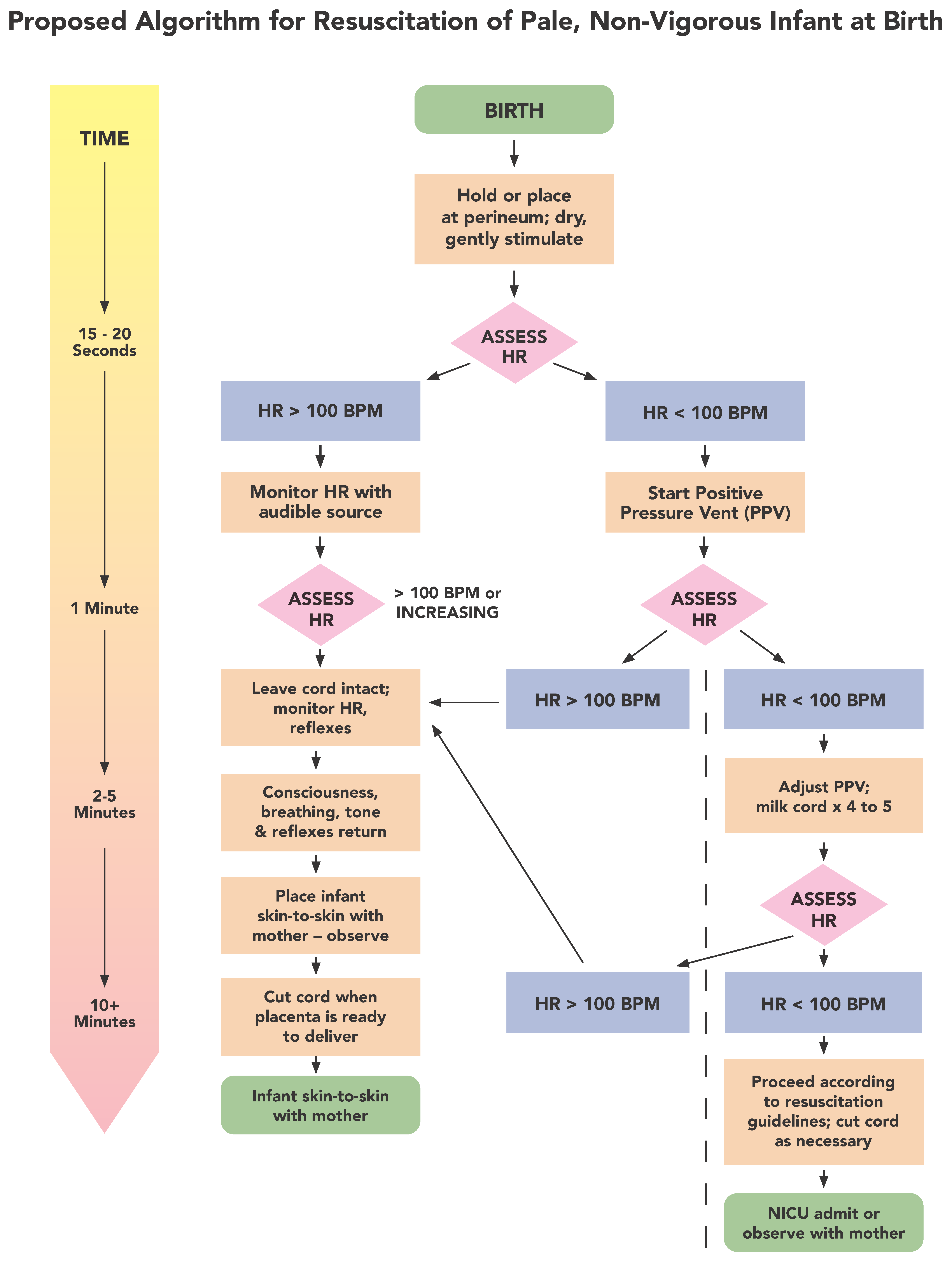
A pregnancy test should be performed in all female patients of childbearing age. If the patient is pregnant and in shock, surgical consultation and the consideration of bedside pelvic ultrasonography should be immediately performed in the ED. Hypovolemic shock secondary to an ectopic pregnancy is common. Hypovolemic shock secondary to an ectopic pregnancy in a patient with a negative pregnancy test, although rare, has been reported.
If thoracic dissection is suspected because of the mechanism and initial chest radiographic findings, the workup may include transesophageal echocardiography, aortography, or CT scanning of the chest.
If a traumatic abdominal injury is suspected, a focused abdominal sonography for trauma (FAST) ultrasonography examination may be performed in the stable or unstable patient. Computed tomography (CT) scanning typically is performed in the stable patient.
If long-bone fractures are suspected, radiographs should be obtained.
Prehospital Care
The treatment of patients with hypovolemic shock often begins at an accident scene or at home. The prehospital care team should work to prevent further injury, transport the patient to the hospital as rapidly as possible, and initiate appropriate treatment in the field. Direct pressure should be applied to external bleeding vessels to prevent further blood loss.
Prevention of further injury applies mostly to the patient with trauma. The cervical spine must be immobilized, and the patient must be extricated, if applicable, and moved to a stretcher. Splinting of fractures can minimize further neurovascular injury and blood loss.
Although in selected cases stabilization may be beneficial, rapid transport of sick patients to the hospital remains the most important aspect of prehospital care. Definitive care of the hypovolemic patient usually requires hospital, and sometimes surgical, intervention. Any delay in definitive care, eg, such as delayed transport, is potentially harmful.
Most prehospital interventions involve immobilizing the patient (if trauma is involved), securing an adequate airway, ensuring ventilation, and maximizing circulation.
In the setting of hypovolemic shock, positive-pressure ventilation may diminish venous return, diminish cardiac outcome, and worsen the shock state. While oxygenation and ventilation are necessary, excessive positive-pressure ventilation can be detrimental for a patient suffering hypovolemic shock.
Appropriate treatment usually can be initiated without delaying transport. Some procedures, such as starting intravenous (IV) lines or splinting of extremities, can be performed while a patient is being extricated. However, procedures in the field that prolong transportation should be delayed. Benefits to giving IV fluids prior to departure from the scene are not clear; however, IV lines and fluid resuscitation should be started and continued once the patient is en route to definitive care.
In recent years, there has been considerable debate regarding the use of military antishock trousers (MAST). MAST were introduced in the 1960s and, based mostly on anecdotal reports of success, their use became standard therapy in the prehospital treatment of hypovolemic shock in the late 1970s. By the 1980s, the American College of Surgeons Committee on Trauma included their use in the standard of care for all patients with trauma and signs or symptoms of shock. Since that time, studies have failed to show improved outcome with the use of MAST. The American College of Surgeons Committee on Trauma no longer recommends the use of MAST.
Emergency Department Care
Three goals exist in the emergency department treatment of the patient with hypovolemic shock as follows:
(1) maximize oxygen delivery – completed by ensuring adequacy of ventilation, increasing oxygen saturation of the blood, and restoring blood flow,
(2) control further blood loss, and
(3) fluid resuscitation. Also, the patient’s disposition should be rapidly and appropriately determined.
Maximizing oxygen delivery
The patient’s airway should be assessed immediately upon arrival and stabilized if necessary. The depth and rate of respirations, as well as breath sounds, should be assessed. If pathology (eg, pneumothorax, hemothorax, flail chest) that interferes with breathing is found, it should be addressed immediately. High-flow supplemental oxygen should be administered to all patients, and ventilatory support should be given, if needed. Excessive positive-pressure ventilation can be detrimental for a patient suffering hypovolemic shock and should be avoided.
Two large-bore IV lines should be started. The Poiseuille law states that flow is inversely related to the length of the IV catheter and directly related to its radius to the fourth power. Thus, a short large-caliber IV catheter is ideal; the caliber is much more significant than the length. IV access may be obtained by means of percutaneous access in the antecubital veins, cutdown of saphenous or arm veins, or access in the central veins by using the Seldinger technique. If central lines are obtained, a large-bore single-lumen catheter should be used. Intraosseous access has and continues to be used for hypotensive children younger than 6 years. Intraosseous access has also been used in hypotensive adults. [3] The most important factor in determining the route of access is the practitioner’s skill and experience.
Placement of an arterial line should be considered for patients with severe hemorrhage. For these patients, the arterial line will provide continuous blood pressure monitoring and also ease arterial blood gas testing.
The position of the patient can be used to improve circulation; one example is raising the hypotensive patient’s legs while fluid is being given. Another example of useful positioning is rolling a hypotensive gravid patient with trauma onto her left side, which displaces the fetus from the inferior vena cava and increases circulation. The Trendelenburg position is no longer recommended for hypotensive patients, as the patient is predisposed to aspiration. In addition, the Trendelenburg position does not improve cardiopulmonary performance and may worsen gas exchange.
Autotransfusion may be a possibility in some patients with trauma. Several devices that allow for the sterile collection, anticoagulation, filtration, and retransfusion of blood are available. In the trauma setting, this blood almost always is from a hemothorax collected by means of tube thoracostomy.
Controlling further blood loss
Control of further hemorrhage depends on the source of bleeding and often requires surgical intervention. In the patient with trauma, external bleeding should be controlled with direct pressure; internal bleeding requires surgical intervention. Long-bone fractures should be treated with traction to decrease blood loss.
In the patient whose pulse is lost in the ED or just prior to arrival, an emergency thoracotomy with cross-clamping of the aorta may be indicated to preserve blood flow to the brain. This procedure is palliative at best and requires immediate transfer to the operating room.
In the patient with GI bleeding, intravenous vasopressin and H2 blockers have been used. Vasopressin commonly is associated with adverse reactions, such as hypertension, arrhythmias, gangrene, and myocardial or splanchnic ischemia. Therefore, it should be considered secondary to more definitive measures. H2blockers are relatively safe but have no proven benefit.
Somatostatin and octreotide infusions have been shown to reduce gastrointestinal bleeding from varices and peptic ulcer disease. These agents possess the advantages of vasopressin without the significant side effects.
In patients with variceal bleeding, use of a Sengstaken-Blakemore tube can be considered. These devices have a gastric balloon and an esophageal balloon. The gastric one is inflated first, and then the esophageal one is inflated if bleeding continues. The use of this tube has been associated with severe adverse reactions, such as esophageal rupture, asphyxiation, aspiration and mucosal ulceration. For this reason, its use should be considered only as a temporary measure in extreme circumstances.
Virtually all causes of acute gynecological bleeding that cause hypovolemia (eg, ectopic pregnancy, placenta previa, abruptio placenta, ruptured cyst, miscarriage) require surgical intervention.
Early consultation and definitive care are the keys. The goal in the ED is to stabilize the hypovolemic patient, determine the cause of bleeding, and provide definitive care as quickly as possible. If transfer to another hospital is necessary, resources should be mobilized early.
In patients with trauma, if the emergency medical services personnel indicate potential serious injury, the surgeon (or trauma team) should be notified prior to the patient’s arrival. In a 55-year-old patient with abdominal pain, for example, emergency ultrasonography of the abdomen may be necessary to identify an abdominal aortic aneurysm before the vascular surgeon is notified. Every patient should be individually evaluated, because delaying definitive care can increase morbidity and mortality.
Resuscitation
Whether crystalloids or colloids are best for resuscitation continues to be a matter for discussion and research. Many fluids have been studied for use in resuscitation; these include isotonic sodium chloride solution, lactated Ringer solution, hypertonic saline, albumin, purified protein fraction, fresh frozen plasma, hetastarch, pentastarch, and dextran 70.
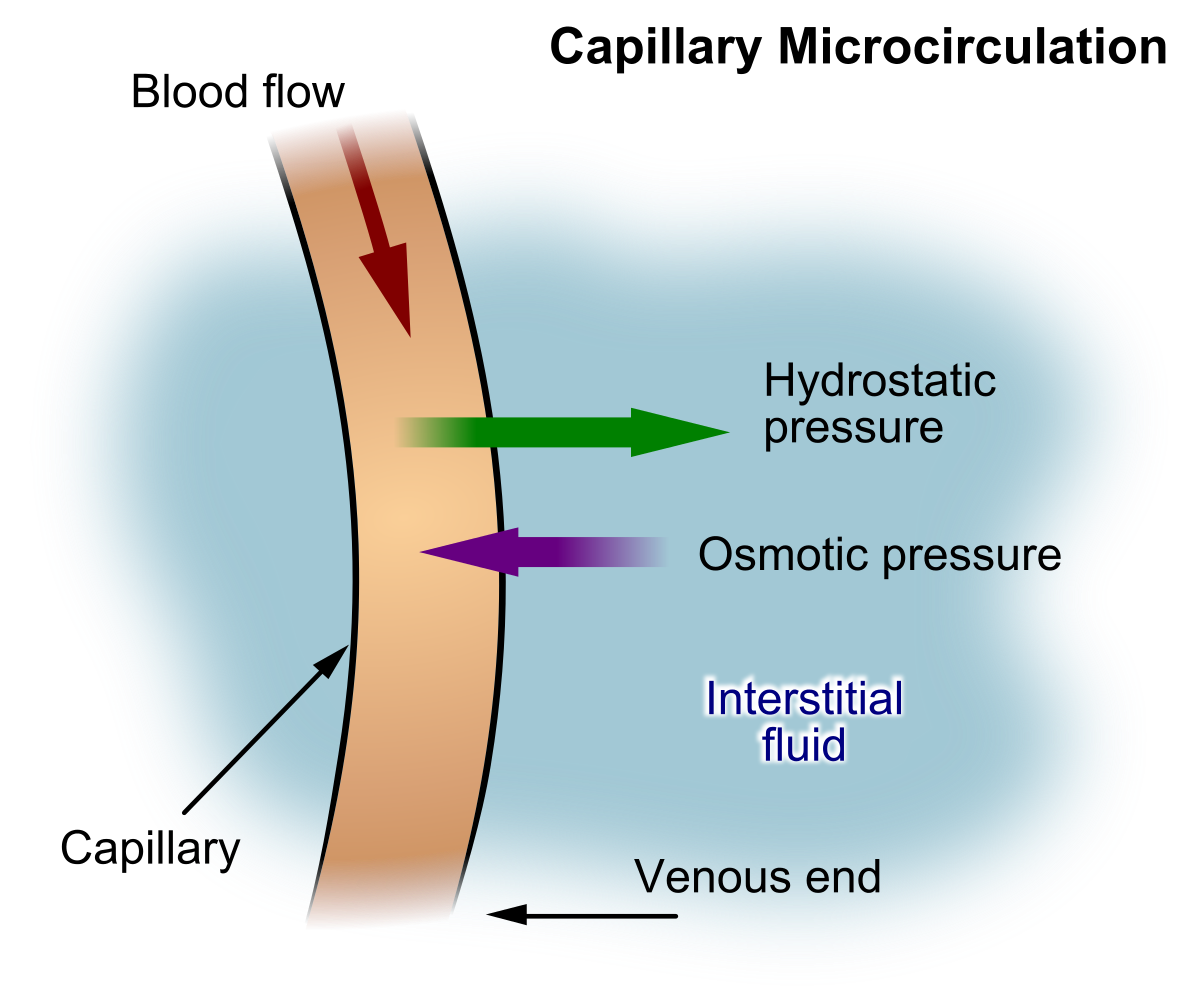
Proponents of colloid resuscitation argue that the increased oncotic pressure produced with these substances decreases pulmonary edema. However, the pulmonary vasculature allows considerable flow of material, including proteins, between the intravascular space and interstitium. Maintenance of the pulmonary hydrostatic pressure at less than 15 mm Hg appears to be a more important factor in preventing pulmonary edema.
Another argument is that less colloid is needed to increase the intravascular volume. Studies have shown this to be true. However, they still have not demonstrated any difference in outcome with colloids compared with crystalloids.
Synthetic colloid solutions, such as hetastarch, pentastarch, and dextran 70, have some advantages compared with natural colloids such as purified protein fraction, fresh frozen plasma, and albumin. They have the same volume-expanding properties, but because of their structures and high molecular weights, they remain mostly in the intravascular space, reducing the occurrence of interstitial edema. Although theoretic advantages exist, studies have failed to show a difference in ventilatory parameters, pulmonary function test results, days using a ventilator, total hospital days, or survival.
The European Society of Intensive Care Medicine (ESICM) advises against the use of colloids-hydroxyethyl starches (HES) in patients with severe sepsis or risk of acute kidney injury. Physicians should also avoid using colloids in patients with head injury and refrain from administering gelatins and HES in organ donors.
The combination of hypertonic saline and dextran also has been studied because of previous evidence that it may improve cardiac contractility and circulation. Studies in the US and Japan have failed to show any difference when this combination was compared with isotonic sodium chloride solution or lactated Ringer solution. Thus, despite the many available resuscitation fluids, current recommendations still advocate the use of normal saline or lactated Ringer solution. In the US, one reason for the predominant use of crystalloids over the other resuscitative fluids is cost.
Recent literature suggests that the early administration of FFP and platelets improves survival and decreases overall PRBC need in patients undergoing a massive transfusion.
Restoring normal circulating volume and BP prior to definitive control of bleeding
During World War I, Cannon observed and characterized patients in clinical shock. He later suggested a model of permissive hypotension in the treatment of torso wounds, with the intent of minimizing further bleeding.
Findings from early studies showed that animals that were bled had increased survival if they received fluid resuscitation. However, in these studies, bleeding was well controlled with ligation after the animals were bled.
During the Korean and Vietnam wars, much more aggressive fluid resuscitation, as well as rapid access to definitive care, was emphasized. It was noted that patients who were aggressively resuscitated tended to have better outcomes, and in the 1970s, these principles were widely adopted in civilian patients.
Since then, many studies have been conducted to determine if these principles are valid in patients with uncontrolled hemorrhage. Most of these studies revealed increased survival in the permissive hypotension or delayed treatment arms. The theory is that increased pressure causes more bleeding and disrupts initial clots, whereas extreme hypotension may increase the risk of cerebral perfusion.
The questions that have not been answered adequately are as follows: Which mechanisms and injury patterns are more amenable to the restoration of circulating blood volume? What BP is adequate but not excessive?
Although some data indicate that a systolic BP of 80-90 mm Hg may be adequate in penetrating truncal trauma without head injury, further studies are needed.
Current recommendations are for aggressive fluid resuscitation with lactated Ringer solution or normal saline in all patients with signs and symptoms of shock, regardless of underlying cause.
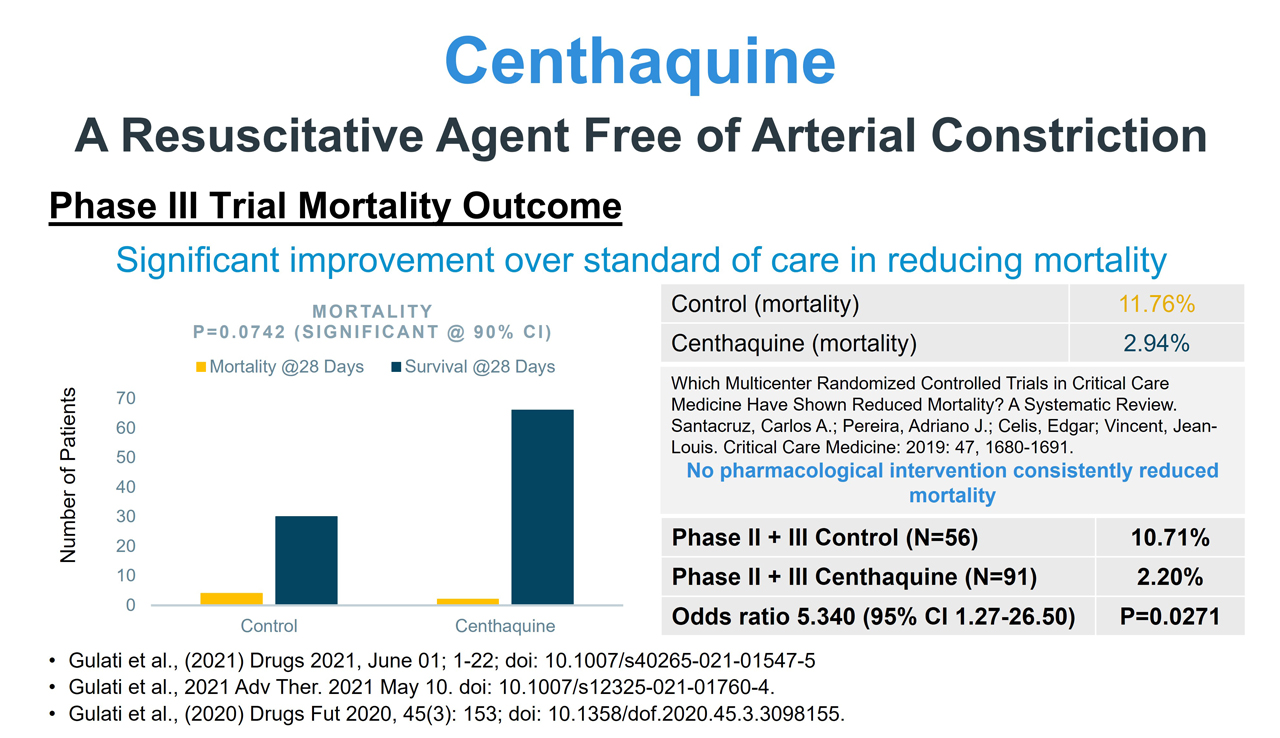
Medication Summary
The goals of pharmacotherapy are to reduce morbidity and prevent complications.
Antisecretory agents
Class Summary
These agents have vasoconstrictive properties and can reduce blood flow to portal systems.
Somatostatin (Zecnil)
Naturally occurring tetradecapeptide isolated from the hypothalamus and pancreatic and enteric epithelial cells. Diminishes blood flow to portal system because of vasoconstriction. Has similar effects as vasopressin but does not cause coronary vasoconstriction. Rapidly cleared from the circulation, with an initial half-life of 1-3 min.
Octreotide (Sandostatin)
Synthetic octapeptide. Compared to somatostatin, has similar pharmacological actions with greater potency and longer duration of action.
Used as adjunct to nonoperative management of secreting cutaneous fistulas of the stomach, duodenum, small intestine (jejunum and ileum), or pancreas.