Key words:
AUD, Fetal Alcoholic Spectrum Disorder, toxicity, binge, addiction, withdrawal
Abstract
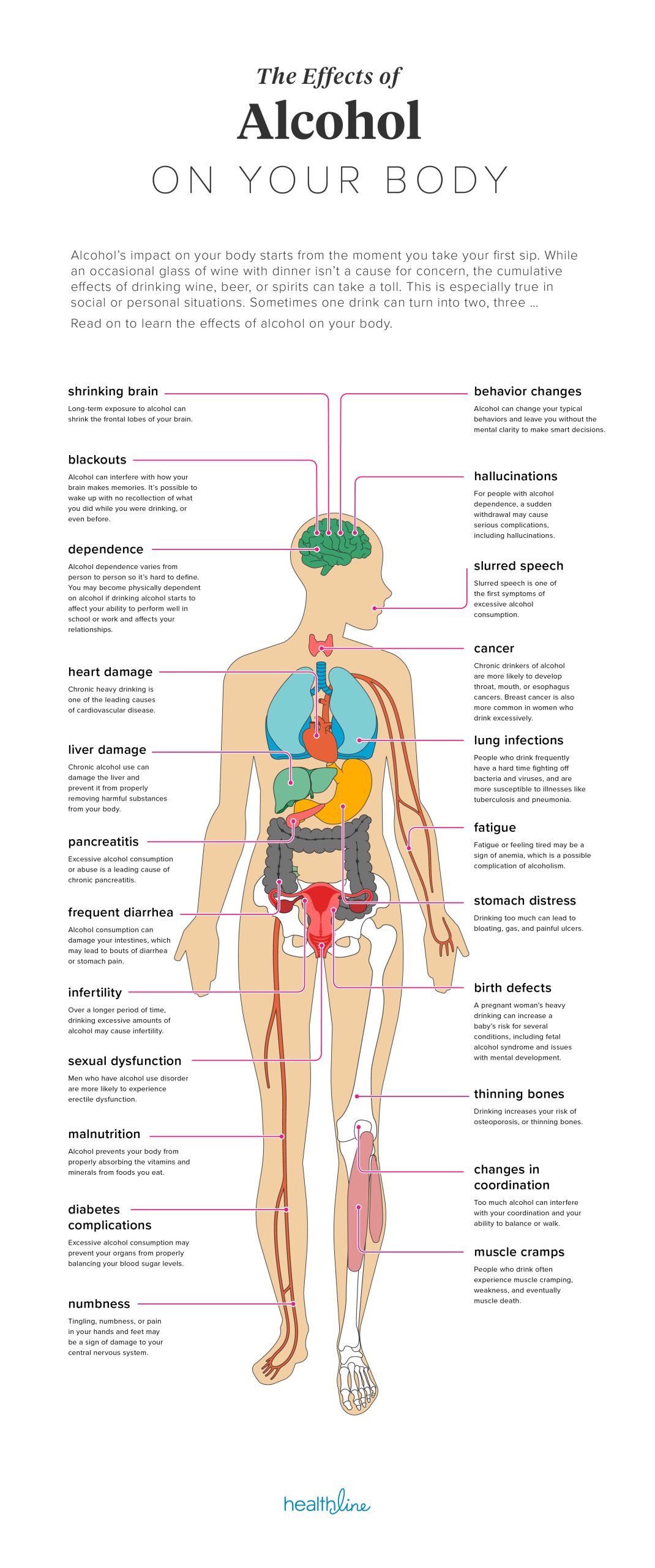
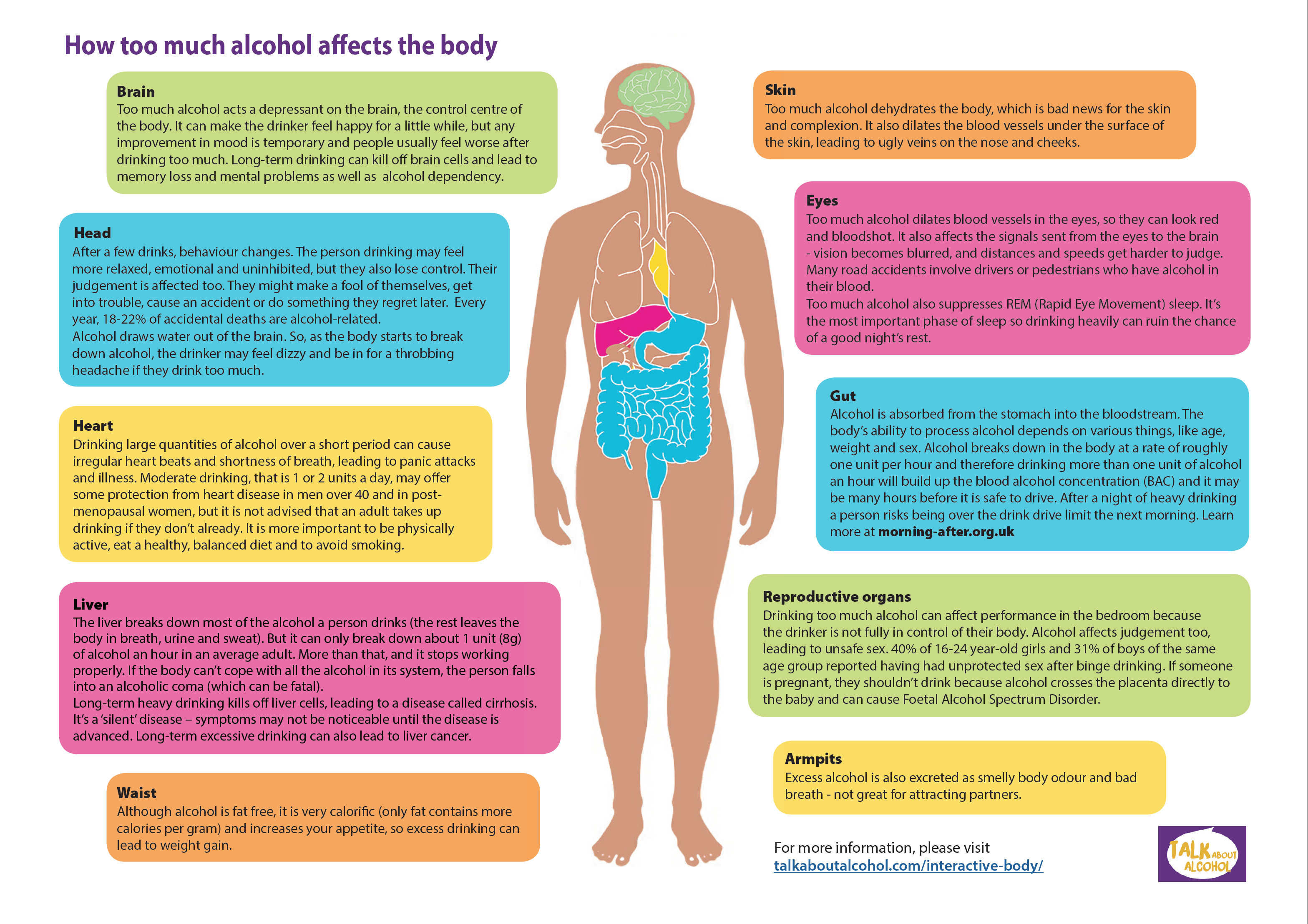
Alcohol is a legal and yet detrimental psychoactive substance, capable of establishing addiction and impacting the physical, mental, social, and economic health of people. Alcohol intake causes a large variety of tissue damages severely impacting the nervous system, digestive and cardiovascular systems and causing oral cavity, oropha- ryngeal, hypopharyngeal, esophageal, colon-rectal, laryngeal, liver and intrahepatic bile duct, and breast cancers. Alcohol can also play a role in the pathogenesis of diabetes mellitus, cardiomyopathy and hemorrhagic strokes. When drunk during pregnancy it is proved to be responsible for serious damage to fetuses causing a wide range of pathological conditions from miscarriage to Fetal Alcoholic Spectrum Disorder (FASD). Acute ethanol intoxication happens when the amount of alcohol consumed is greater than the disposal capacity of the liver, causing an accumulation of its metabolites displayed by initial dys- phoria and disinhibition. Nausea, vomiting, memory loss could hap- pen. Although, it can lead to more serious conditions like impaired speaking, impaired coordination, unstable gait, nystagmus, stupor, or coma. Respiratory depression and death could also happen in such cases. Unfortunately, diagnosis of acute alcohol intoxication is difficult because most of the drinkers deny or minimize their assumption. It is dramatically important to assess when the last intake happened to avoid withdrawal syndrome. Alcohol acute intoxication can be considered a serious harm to health and a relevant issue for healthcare provid- ers working in emergency rooms. Differential diagnosis is crucial to avoid serious outcomes. There is no consensus about therapies for acute intoxication, but supportive and symptomatic treatments were proved effective. The repercussions of alcohol misuse over drinkers’ social, familiar, economical and working life enhance the importance of a multidisciplinary approach in such cases.

Introduction
The World Health Organization (WHO) included the use of alcohol and other psychoactive substances in the manual for the “International Statistical Classification of Diseases and Health Problems” (ICD9 – CM). The “Statistical Dia- gnostic Manual of Mental Disorders” (DSM-5). The Ame- rican Psychological Association (APA) (1) includes alcohol in the chapter “Substance-Related Disorders and Addiction Disorders”. In particular, the chapter “Alcohol-Related Di- sorders” includes Alcohol Intoxication, Abstinence Syndro- me, Alcohol Use Disorder, Other Alcohol-Induced Disorders and Unspecified Alcohol-Related Disorders.
Alcohol is a legal and socially accepted drug, but it is also very deleterious because of its psychoactive powers. This substance can induce a very strong addiction in people who use it establishing a negative bond that affects the lifestyle of a drinker, impacting their physical, mental, family and social health (2–12). Finally, alcohol is a teratogenic substance in- ducing cancer and other severe diseases (13–17), that is also capable of developing malformations when future mothers are exposed during pregnancy (18-21). This can result in the birth of a baby with severe birth defects, including a wide range of deformities and disabilities identified as “Fetus Al- coholic Syndrome (FAS)” or a “spectrum” of abnormalities that can have a wide degree of variability from mild to very severe (Fetal Alcohol Spectrum Disorders, FASD) (22) as also shown in animal models (23-28).
Acute ethanol intoxication happens when the amount of alcohol consumed is greater than the disposal capacity of the liver, causing an increase in the concentration of alcohol and its metabolites and it causes changes in the behavioral spherebothinaddictedandnon-addictedpeople.Veryoften, the resulting clinical manifestations (initially dysphoria and disinhibition), are not taken into adequate consideration by both medical professionals and common laypeople especially because these effects subside spontaneously over time. When alcohol and its metabolites accumulate in the blood faster than they can be metabolized by the body, symptoms ranging from dysphoria to disinhibition may appear, up to coma, respiratory depression and death in the most serious cases. There is not an internationally recognized cut-off for blood alcohol concentration to define acute intoxication. The acute effects of alcohol depend on the amount ingested, the time, the speed of absorption and the speed with which the detoxification/metabolization systems act. The Italian High- way Code considers, for legal purposes only, that the subject drives while intoxicated if the blood alcohol concentration (BAC) is> 0.5 g / l. Moreover, changes in psychomotor and cognitive activity and changes in behavior are also appre- ciable for values of 0.2-0.4 g / l. In individuals who have not developed tolerance, a night of deep but disturbed sleep can be observed, already with concentrations of 0.15 g / l, while death can occur at levels between 3 – 4 g / l. In the case of excessive intakes prolonged over time, a greater tolerance is developed and people with a BAC of 4-5 g / l can present only mild dysphoric notes. Type of drink, the time in which it is taken by the subject, the concomitant use of other psy- choactive substances or drug therapies, the general condition of the person and his state of health are factors that could influence the rapidity of upcoming signs and symptoms. Lastly, the degree of personal tolerance in people with addiction influences tolerance: enzyme induction causes faster metabolism, with the need to take larger quantities of alcohol to reach a state of intoxication. This condition not
only affects alcoholics but anyone who is exposed to risk behaviors, especially “binge drinkers” (meaning people who drink 4 or more Alcoholic Units (AU) in women, 5 or more AU in men, taken on the same occasion).
Acute and chronic effects of ethanol on systems, equipment and organs
Alcohol is mainly absorbed through the small intestine. Only 10-20% of the alcohol consumed is absorbed by the stomach. The intestinal mucosa begins to absorb alcohol within 10 minutes of consumption and the maximum serum concentration of alcohol in the blood is reached between 30 and 90 minutes (29). One Alcohol Unit (AU) increases the concentration of alcohol in the blood of a man by 70 kg by 15-20 mg / dL, while in the woman, for the same amount of AU taken, the blood concentration is higher. 90% of the absorbed alcohol is metabolized in the liver at an average of 15-20 mg / dL / h. Therefore, alcohol consumption in excess accumulates in the body and induces symptoms of intoxication. This also happens because the use of other alcohol elimination systems (mainly the microsomal etha- nol oxidizing system) use NADPH instead of NADH as an acceptor of hydrogen in the reaction of transformation of alcohol into Acetaldehyde. This reaction produces free radi- cals (including superoxide) which can damage any organ and apparatus, with vulnerability at the neurological, gastrointe- stinal, cardiovascular and respiratory levels (Fig. 1).

Fig. 1 – Alcoholic oxidation. Alcohol is oxidized by alcohol and aldehyde dehydrogenase to acetyl CoA. Depending on the nutritional, hormonal, energy state, acetyl-CoA is converted into the indicated products (NAD – Nicotinamide adenine dinucleotide; ADH – Alcohol dehydrogenase; ALDH – Aldehyde dehydrogenase; AMP – Adenosin monophosphate; PPi – Pyrophosphate; ACSS1/2 – Acyl-CoA synthetase 1/2).
There are more than 100 gene families that encode the P450. The P450s are arranged in families based on sequence homologies. CYP2E1 is a P450 that has the highest oxidation activity of alcohol to Acetaldehyde. In addition to ethanol, CYP2E1 is capable of oxidizing many other compounds (acetone, benzene and other alcohols). At low alcohol con- centrations, CYP2E1 can reach about 10% of the liver’s total alcohol oxidation capacity. Moreover, since it has a higher Michaelis-Menten constant (Km), so its activity increases with the increase in the concentration of alcohol in the blood. CYP2E1, like many other P450s, is induced by its substrate, allowing more alcohol to be eliminated, playing an important role in alcohol metabolism in subjects with DUA and with chronic high alcohol consumption. Diet supplementation with antioxidant compounds may reduce or counteract the risk of oxidative stress induced by alcohol abuse as disclosed in humans and animal models (9, 30-37).
Alcohol-Drug Interactions
Ethanol is not the only substance that is oxidized by CYP2E1; other drugs also use this metabolic pathway and compete with alcohol. Drinkers often have a greater sensiti- vity to certain drugs because alcohol competes with them for the use of CYP2E1, prolonging the half-life of these drugs and, therefore, their action. On the contrary, when there is a chronic high consumption, able to induce the activity of CYP2E1, the metabolism of drugs, which also share the condition of the substrate of CYP2E1, is increased so that their elimination is faster. The decrease in the half-life con- sequently leads to a decreased effectiveness of the drug when alcohol concentrations vary in size. The catalytic activity of CYP2E1 leads to the production of large quantities of reactive oxygen intermediates such as superoxide radicals and hydrogen peroxide. This production may be important in the mechanisms of alcoholic liver damage involving oxidative stress (38).
Nervous system
Affecting the nervous system, alcohol intoxication is characterized by anterograde, temporary amnesia, usually referred to as a “blackout”, in which the person is unable to remember what happened during a drinking episode (39). The blackout results from a rapid increase in blood alcohol concentration that blocks the consolidation of short-term memory into long-term memory, a process involving the hippocampus and medial temporal structures (40). Intoxi- cated people may have relatively efficient remote memory and are often unaware that they have specific recent memory problems and cannot remember events that occurred a few minutes earlier (41-42). Temporary blackouts should be di- stinguished from chronic global (antegrade and retrograde) amnesia associated with Korsakoff syndrome (43).
Another common consequence of alcohol intoxication is the lack of perception of impaired motor and cognitive functions so that the risk of car accidents during alcohol intoxicationincreases.Verbalfunctions,visuospatialmemo- ry, information processing, inhibitory control and working
memory are compromised (44). It is commonly misbelieved that alcohol consumption promotes sleep: actually, alcohol has the only effect of promoting sleep by actioning on the Gabaergic system. Alcohol causes a shortening of the duration of a deep sleep, and the REM phase, resulting in a fragmentation of sleep that does not allow for true rest and affects the progress of daily life. Alcohol exacerbates obstructive sleep apnea by relaxing the pharynx muscles, with narrowing of the upper airways (45-46). After an epi- sode of intoxication, chronic alcoholics often report signs of peripheral neuropathy, such as numbness in the limbs, tingling, burning sensations, and paranesthesia. The signs are generally bilateral and are more pronounced distally than proximally. A well-known mechanism of action of alcohol abuse is the impact that drinking alcohol has on the phy- siology of neurotrophins as nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF) (47-51), proteins playing subtle roles in nerve cells growth, development, nu- trition, death and in the regulation of the behavior in normal and pathological conditions (52-69).
Gastrointestinal system
Alcohol intake can irritate the esophagus and stomach and promote relaxation of the lower esophageal sphincter: these are the reasons why esophagitis, gastritis, gastric ul- cers, esophageal and fundus tumors are frequent in subjects with addiction. High concentrations of alcohol can cause pyloric spasms, resulting in nausea and vomiting. Violent retching can induce hematemesis due to a longitudinal tear in the mucosa at the gastroesophageal junction (Mallory-Weiss syndrome, or even can lead to a rupture of the esophagus (Boerhaave syndrome). Other consequences of excessive drinking can be inflammation of the pancreas which can lead to acute pancreatitis. Alcohol impairs gluconeogenesis and the oxidation of fatty acids in the liver, resulting in steatosis. The steatotic liver is reversible if abstinence is maintained and generally does not cause serious harm; however, repe- ated episodes of excessive drinking can cause acute alco- holic hepatitis, liver cirrhosis and liver cancer (70). Alcohol consumption could lead to alterations in the gut microbiota composition, even before liver disease development. These modifications worsen with progressing disease and could be complicit in disease evolution. It has been demonstrated even in the presence of cirrhosis and alcoholic hepatitis that microbial function, especially associated with bile acid metabolism, could modulate alcohol-associated injury. Mi- crobiota might also affect brain function, and the gut-brain axis might be a potential target to reduce alcoholic relapse risk (71-73).
Cardiovascular system
The relationship between alcohol intake and cardiovascu- lar disease is complex, as it appears to have both protective and harmful roles (33-74). Moreover, the excessive daily consumption of alcoholic beverages causes a linear increase in dose-dependent blood pressure, which tends to normalize within two weeks of alcohol abstention (75-76). Excessive, chronic, alcohol drinkers have a greater risk of dilated car- diomyopathy. Cardiomyopathy contributes to arrhythmias, left ventricular compromise, mitral valve regurgitation with associated thrombus and congestive heart failure. Arrhythmias (including atrial and ventricular fibrillation) can occur temporarily after episodes of excessive drinking even in individuals who show no evidence of heart disease (77). Alcohol abuse affects also the relationship between the cardiovascular system and neurotrophins since both NGF and BDNF possess fundamental roles in the mechanisms of atherosclerosis formation (78-89).
Other alcohol-related diseases
The main life-threatening consequence of acute intoxi- cation with high blood alcohol concentrations is respiratory depression. In these conditions, intoxication also reduces the sensitivity of the airways and the reflex block of foreign bodies, increasing the risk of aspiration of the same, as well as of food. Chronic alcohol consumption, combined with the frequent nutritional deficiencies in people with addiction, can lead to inhibition of the bone marrow, resulting in a reduction in the production of red blood cells (anemia), white blood cells (neutropenia) and platelets (thrombocytopenia). There is also an increase in the volume of red blood cells (increase in mean corpuscular volume, MCV) due to a lack of vitamin. B12 and Folic Acid (90). Thrombocytopenia increases the risk of excessive bleeding (for example, hemorrhagic stroke), especially in subjects who have deficient prothrombin activi- ty. Regardless of peripheral neuropathy, chronic alcoholics may have muscle weakness or cramps caused by acute (91) and chronic (92) alcoholic myopathy.
Alcohol also interferes with the absorption and metabo- lism of calcium in the skeletal system. Chronic alcoholics may show lower bone density and reduced growth in the epi- physis, resulting in an increased risk of fractures concerning falls and osteonecrosis of the femoral head (93-94).
Excessive alcohol consumption during adolescence can disrupt normal sexual development and alter the onset and progress of puberty. Even in the absence of liver cirrhosis, in chronic alcoholism, men can show testicular atrophy, gynecomastia, decreased ejaculate volume and altered hair disposition of the body (95). In women, alcohol can chan- ge the levels of sex hormones and alter ovarian function, resulting in amenorrhea, infertility and an increased risk of miscarriage (96).
In acute alcohol intoxication, cortisol levels and diuresis increase (by inhibition of vasopressin). Decreases the secre- tion of serum thyroxine and triiodothyronine.
Diagnostic criteria for alcohol intoxication
Diagnosis
The diagnosis can usually be based on the medical hi- story and physical examination. Unfortunately, intoxicated patients may deny or underestimate their maladaptive pat- tern of alcohol use. Therefore, the person’s history should be investigated by acquiring information from relatives or friends whenever possible.
It is very important to be sure of the last alcohol intake
to prevent and manage symptoms of alcohol withdrawal, which can develop as early as 6-8 hours after stopping al- cohol consumption. However, doctors should be aware that laboratory analyzes do not always show signs of intoxication with diriment values.
Clinical features
According to the DSM 5, alcohol intoxication is a clini- cal diagnosis based on the presence of clinically significant problems and behavioral or psychological changes, accom- panied by physiological signs of intoxication, including con- fusing language, incoordination, unstable gait, nystagmus, conjunctival injection, impaired attention or memory, stupor or coma (DSM-5, see table).
Effects of alcohol
Effects of alcohol are related to the concentration of alcohol in the blood (Table 2), although other factors may change the absorption and kinetics of alcohol (individual body weight, sex, age, volume ingested, percentage of alco- hol in the drink and whether alcohol was taken on an empty stomach or with food, type of food, etc ….). Tolerance can develop in addicted subjects, but also in those who regularly drink hazardously. The effects shown in table 2 refer to users of moderate or abstained amounts of alcohol. Furthermore, individual differences in signs and symptoms may also vary based on genetic susceptibility (97).
Clinical conditions, which may accompany acute alcohol intoxication, in particular, those associated with chronic alcohol consumption
The patient in acute alcohol intoxication is often suffe- ring from medical comorbidities related to chronic alcohol abuse. For this reason, expanding investigations should always be considered to identify potential problems that require specific interventions on organs and systems, con- sidering the patient’s clinical characteristics and the genesis of organic alcohol injury. Particular attention should be paid to changes in mental status, which could range from mild euphoria and disinhibition to lethargy and coma. Likewise, mental states inconsistent with history information should require clinical attention and further evaluation.
Various conditions can mimic or be covered by the alte- ration of the mental state due to acute alcohol intoxication (Table 3).



Hepatic encephalopathy
Hepatic encephalopathy is defined as an affection of central nervous system functioning (mental confusion, altered level of consciousness and coma) due to liver failure. Hepatic encephalopathy is a complication of liver cirrhosis in which the liver is no longer able to eliminate ammonia from the blood, which accumulates and affects brain neu- rotransmission. It is often determined acutely, following a precipitating event (gastrointestinal bleeding, anemia, electrolyte alterations, etc….). Sudden mood changes, episodes of mental confusion, personality changes must make one suspect the presence of hepatic encephalopathy. Frequent the presence of Flapping tremor, or Asterissi, ob- servable by asking the subject to stretch the arms forward and flex the hands dorsally, opening the fingers in a fan. In this position, in subjects with encephalopathy, coarse tre- mors appear characterized by large arrhythmic jolts, called “butterfly beating”, due to intermittent loss of muscle tone. These signs are potentially reversible with the correction of precipitating factors and rest contributing to the impro- vement of liver function (98). In advanced stages, however, it can eventually evolve into hepatic coma and death. The diagnosis of hepatic encephalopathy is confirmed by the laboratory when the blood ammonia values are abnormal. Moreover, ammonia levels can be normal in 10% of patients with hepatic encephalopathy (99). Alcohol intoxication can precipitate hepatic encephalopathy by exacerbating under- lying problems such as electrolyte disturbances, infection and dehydration. Therefore, hepatic encephalopathy should always be suspected when an intoxicated patient exhibits changes in mental status simultaneously with potential precipitating events (100).
Wernicke – Korsakoff syndrome
Alcoholism remains the most common cause of thiami- ne deficiency in industrialized countries. Alcoholics are at risk of thiamine deficiency due to poor nutritional intake, impaired intestinal absorption and its use (101). Wernicke’s encephalopathy is an acute neurological disorder characte- rized by changes in mental status, ataxia (mainly affecting gait) and a variety of ocular motility abnormalities due to thiamine deficiency. The most common symptoms of Wer- nicke’s encephalopathy are non-specific and range from apathy to inability to concentrate, confusion and, if not treated properly, coma. Nystagmus and ophthalmoplegia are common signs. Ataxia is characterized by an uncoordinated gait (102-103). Clinical diagnosis may not be simple: as early as 1986, Harper and colleagues reported that 80% of patients with Wernicke-Korsakoff syndrome, found during autopsy exams, had not been diagnosed as such during life. Only 16% had the classic clinical triad and 19% had no documented clinical signs. The cited authors suggested that at least some cases of Wernicke-Korsakoff syndrome may be the result of repeated subclinical episodes of vitamin B 1 deficiency. Therefore, physicians must pay close attention to the patient group to make a diagnosis.
The clinical diagnosis is mainly supported by the dra- matic improvement of neurological signs with parenteral administration of thiamine (500 mg x 3 / day, in our ex- perience, in which thiamine is administered only intramu- scularly, even 200-300 mg in the same syringe x 3 / day). Therapy must be started as early as possible, including to prevent Korsakoff syndrome (104). In fact, if Wernicke’s encephalopathy is not treated, 80% of patients can progress to Korsakoff’s syndrome.
Korsakoff’s syndrome is defined as a notable weake- ning of declarative memory, compared to other aspects of cognitive function. Initially, the disorder gives variable manifestations; persistent memory impairment in the past could have resulted from non-alcoholic causes, presumably from more severe nutritional deficiencies. Some studies suggest that the circuitry involving the mammillary bodies, the mammillary-thalamic tract and the anterior thalamus are important for the formation of new memories. Neuroimaging studies confirmed the metabolic and structural abnormalities detected on necropsy, particularly in the frontal lobes.
The main feature of Korsakoff’s syndrome is the extent of the impairment of declarative memory compared to other cognitive functions, which becomes increasingly evident with the resolution of the confusional state of Wernicke’s encephalopathy (43).
Idiosyncratic or pathological intoxication
This condition is characterized by a marked aggressive- ness, which develops rapidly after the ingestion of an amount of alcohol normally insufficient to induce intoxication. Ho- wever, the validity, as a diagnostic entity, of idiosyncratic alcohol intoxication is still under discussion (105).
Treatment of acute alcohol intoxication
Pre-hospital assistance
In the case of acute intoxication observed in a territorial service, the operator who intercepts it must try to give as much information as possible on the circumstances in which the first intervention took place, the place, the presence and the number of empty containers and the type of drink that was contained in them; the patient’s blood sugar and mental status.
Emergency Room (ER)
The admissions to the emergency room of people with alcohol-related disorders are very frequent. Around 30% of people who access ERs have problems directly or indirectly related to alcohol (106). In our experience, this percentage is very similar (26%, (107)), and more frequently concerns injuries (108), trauma and accidents (50%, (109). The state of intoxication is frequently accompanied by psychiatric ma- nifestations and other organic disorders. These data should prompt emergency room workers to pay greater attention in trying to identify problems related to alcohol use and to implement appropriate responses (108). Another problem to be addressed is the high frequency with which alcohol- related hospitalizations are linked to social, professional, family problems (109). These situations make the overall picture of the individual’s health even more complicated: in such cases a multidisciplinary approach is fundamental.
However, a lack of training and awareness of doctors and hospital staff on the problems of addiction is quite frequent. Health professionals do not recognize or do not
give the appropriate importance to the problems caused by alcohol while patients refuse to consider themselves sick (110-111).
Pharmacological therapy
In case of emergency, it is a priority to prevent alcohol withdrawal and treat any psychiatric disorders that may be present in comorbidities (112-114).
As for all patients who go to the Emergency Department, the initial treatment is aimed at maintaining a patent airway, supporting breathing and cardiovascular function. Gastric lavage is only rarely necessary: the exception occurs when the patient presents immediately after the ingestion of alco- hol, that is, in a time, that is, in which one could reasonably expect to eliminate a significant amount through aspiration employing a nasogastric tube.
It is advisable to start a treatment of rehydration and reintegration of deficient vitamins:
– Infusion of 1.5 L / day, (be careful to administer at least 100 mg of i.m. thiamine, before infusing glucosate solutions);
– Vitamins of group B: the vitamins of group B (folic acid, pyridoxine, thiamine) are often deficient in alcohol abu- sers (115) and can be useful, in selected cases, to reduce the toxicity of metabolites alcohol).
Treatment of ethanol intoxication is predominantly
supportive and symptomatic (116).
The first step includes a complete assessment of the
patient’s medical situation, including the history of alcohol consumption. Or other substances that may interfere with his medical condition
If the use of gastric lavage is deemed useful, the patient must be placed in lateral decubitus to prevent aspiration into the bronchi of liquids or foods. Dehydration should be corrected immediately and electrolyte and blood sugar levels checked. Hyponatremia must be managed with care because rapid correction can induce central pontine mye- linolysis (117).
To prevent Wernicke’s encephalopathy thiamine must be administered parenterally before any glucose administration (118). Antiemetic drugs can be useful in patients with nausea and vomiting. Prolonged vomiting could indicate a head injury that is not properly appreciated, so in the suspicion of a cerebral hemorrhage, it is advisable to carry out thorough investigations. Slurred speech, ataxia, altered mental status, and other neurological signs of alcohol intoxication can pose some difficulties in differential diagnosis with other medical conditions; therefore, ongoing re-evaluation of mental status and neurological symptoms is required.
There is no antidote for alcohol intoxication, just as we have no effective remedies for the prevention or treatment of an alcohol hangover (119).
The utility of metadoxine therapy (pyridoxol L-2-pyr- rolidone-5-carbohydrate) has been reported for its ability to accelerate ethanol metabolism due to several mechanisms, including increased acetaldehyde dehydrogenase activity, the plasma clearance of ethanol and acetaldehyde and the urinary elimination of ketones (120-122). However, these data have not yet reached an adequate level of clinical evidence. Recently, an attempt has been made to use the nanocomplex technique, in which enzymes important for certain reactions are encapsulated within a thin polymer shell, trying to emulate organisms that have sophisticated subcellular compartments containing enzymes, effective in chemical transformation and elimination of toxic metabo- lic wastes (123,124). These nanocomplexes exhibit better catalytic efficiency and greater stability than free enzymes. Nanocomplexes containing alcohol oxidase and catalase are being investigated to reduce blood alcohol levels by offering an alternative and prophylactic antidote for alcohol intoxication (125).
Discussion
Although Alcohol use is legal and socially acceptable (33), alcohol misuse can undoubtedly be considered one of the most relevant challenges in Western Countries (126-129). Indeed, around 2.3 billion people in the world drink alcoholic beverages (130) and more than 3 million people died as a result of harmful use of alcohol in 2016 (131).
Alcohol intake can play a detrimental effect on health, causing a large variety of tissue damages. The most affected systems are the nervous system, digestive and cardiovascular systems (Global status report on alcohol and health 2018). The International Agency for Research on Cancer (IARC) has determined that alcohol consumption is causally related to the oral cavity, oropharyngeal, hypopharyngeal, esopha- geal, colon, rectal, laryngeal, liver and intrahepatic bile duct, and breast cancers (13,132-135). However, chronic alcohol consumption has been observed to disrupt glucose home- ostasis and lead to insulin resistance, resulting in a higher risk of diabetes mellitus in drinkers (136-138). Alcohol has a clear impact on hemorrhagic strokes, causing 9.5% of all hemorrhagic stroke deaths, hypertensive heart disease, causing 7.4% of all hypertension deaths, cardiomyopathy, causing 6.8% of all cardiomyopathy deaths, and ischemic heart disease, causing 2.7% of all ischemic heart disease deaths (131). Alcohol is causally related to an increase in the risk of both liver cirrhosis and pancreatitis (139), cau- sing an estimated 637 thousand digestive disease deaths in 2016. Within the burden of alcohol-attributable digestive diseases, alcohol-attributable liver cirrhosis caused 607 thousand deaths, while alcohol-attributable pancreatitis resulted in 30 thousand deaths (131). Moreover, alcohol can affect the innate and the acquired immune system and, thus, increase vulnerability to infectious diseases (138). An association between infectious diseases and alcohol assum- ption was found (137). Alcohol consumption was proved to push people into adventurous sexual behaviors and to increase the likelihood of unprotected sex, contributing to the spread of venereal diseases (139,141). There are also evidences that in the alcohol use disorder population, 50.3% of patients had psychiatric comorbidity during their lifetime (113,114,142–144).
Alcohol assumption during pregnancy is proved to be responsible for serious damage to fetuses causing a wide range of pathological conditions like miscarriage (145- 147), stillbirth (147-148), morphology (22) and growth impairments (149), premature birth (147-148) and neonatal
sequelae related to FASD (150-152). This condition can result in physical abnormalities and neurodevelopmen- tal impairments such as typical facial deformities (153), behavioral disorders (154), lowered functional IQ score (155) and poor performances at school (156). Fetal Al- cohol Syndrome (FAS) is a completely avoidable form of developmental disability (157-158) resulting from alcohol consumption during pregnancy. Data from different study groups showed that even the father’s alcohol assumption is relevant (159-161). Nowadays, it is not possible to establish a safe threshold of alcohol consumption, therefore, the safest recommendation for pregnant women and couples that are looking for a pregnancy (19,162-163) is to avoid alcohol use during pregnancy (164) and breastfeeding (165).
Alcohol acute intoxication can be considered a serious harm to health and a relevant issue for healthcare providers working in the emergency rooms and territorial facilities. Alcohol intoxication signs and symptoms could be mi- sunderstood or underestimated (166-169). Differential diagnosis is crucial to avoid coma, respiratory distress and death in patients with acute intoxication. There is no una- nimous consensus about therapies for acute intoxication, but supportive and symptomatic treatments based on clini- cal expertise were proved effective. The repercussions of alcohol misuse over drinkers’ social, familiar, economical and working life, enhance the complexity of such situations make the overall picture of the individual’s health even more complicated: in such cases a multidisciplinary approach is fundamental.