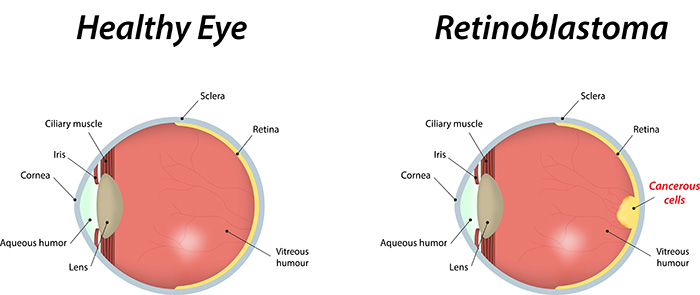
Retinoblastoma is rare and so your child will go to a specialist centre for treatment. There are different treatments such as freezing and laser therapy, chemotherapy, radiotherapy and surgery. The treatment your child has depends on several things including the size of the cancer and if it is in one or both eyes.
Treatment centres
There are 2 specialist retinoblastoma centres in England and they are:
- The Royal London Hospital
- Birmingham Children’s Hospital
These 2 centres serve all parts of the UK including Wales, Scotland and Northern Ireland. They have teams of specialists who know a lot about retinoblastoma and how to treat it. Your child may have some of their treatment in their local cancer unit which is overseen by one of the specialist retinoblastoma centres.
There is a lot to think about as a parent and you’re likely to worry about getting the best treatment for your child. Talk to the doctors or specialist nurses about any worries that you have. They might also be able to put you in touch with other parents of children who have already been through diagnosis and treatment.
Deciding which treatment your child needs
A team of doctors and other professionals discuss the best treatment and care for your child. They are called a multidisciplinary team (MDT).
The aim of the treatment is to get rid of the cancer, save the eye or eyes, and provide the best possible vision for your child. The doctors also want to provide treatment with the least possible side effects, both in the short and long term.
Treatment planning for your child depends on several factors including:
- where the cancer is
- if the cancer is in one or both eyes
- the size of the cancer
- how far it has spread
- the number of sites of cancer in the eye
Your child’s doctor will talk to you about the treatment, its benefits and the possible side effects.
Treatment overview
Treatment for your child might include one or more of the following:
- freezing therapy (cryotherapy)
- laser therapy
- chemotherapy
- radiotherapy
- surgery
Children usually have their treatment while they are asleep under general anaesthetic  . They’ll be awake if they’re having chemotherapy into their bloodstream (systemic chemotherapy).
. They’ll be awake if they’re having chemotherapy into their bloodstream (systemic chemotherapy).
Types of treatment:
Freezing therapy (cryotherapy)
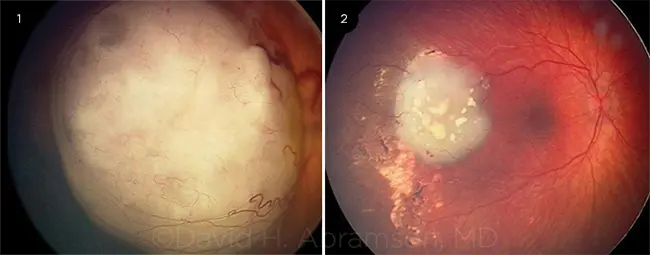
Cryotherapy is a treatment that uses extreme cold to destroy cancer cells. It’s a local treatment, which means that it only affects the area where you have the treatment. It doesn’t treat any cancer cells in other parts of the body. Cryotherapy is best for retinoblastomas that are in the outer edge of the retina.
The doctor uses a metal probe that’s cooled to an extremely low temperature. The probe then freezes the cancer cells and kills them.
Laser therapy
There are 2 types of laser treatment for retinoblastoma:
- photocoagulation
- thermotherapy (transpupillary thermal therapy (TTT)) or heat therapy
A laser is a very thin, focused beam of light that destroys the tissue it’s directed at. The doctor aims the beam through the dark centre of the eye called the pupil.
Photocoagulation laser treatment is different to thermotherapy. This is because the laser delivers the light at different strengths. Photocoagulation laser treatment destroys tissues.
Thermotherapy is another type of laser treatment. This treatment uses an infrared light. The doctor aims this light at the cancer and slowly burns away the cancer cells, destroying them by heat.
Your child usually has laser treatment if the cancer is small and at the back of the eye. They also might have laser treatment with or after chemotherapy.
Radiotherapy
Doctors treat some retinoblastomas with radiotherapy. Radiotherapy means the use of radiation to treat cancer cells.
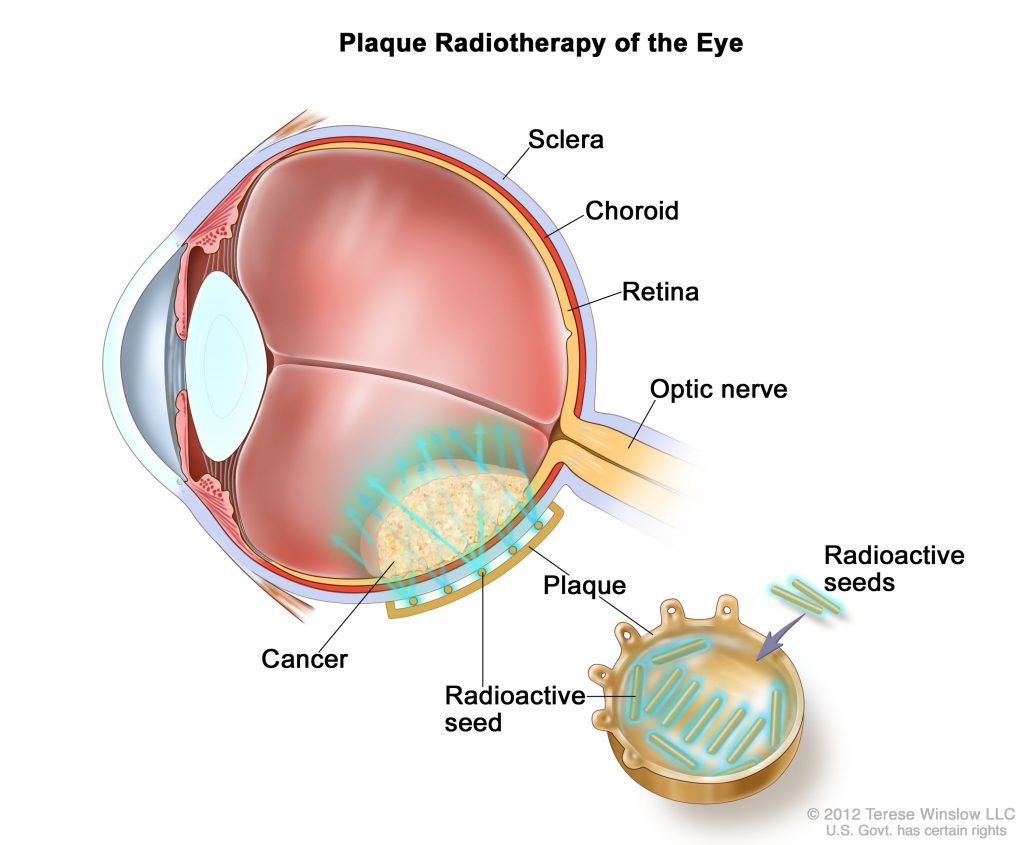
Your child might have a type of radiotherapy called brachytherapy. This means your child has a small radioactive disc called a plaque stitched directly over the cancer. The plaque works by continually delivering a high amount of radiation to a small area (the part of the eye it covers). You might hear it called localised radiotherapy. Your child will have the plaque in place for a set number of days. The doctor then removes the plaque.
Proton beam radiotherapy is a type of external radiotherapy. Your child might have this if the cancer has spread to the optic nerve in the socket of the eye. Proton beam therapy uses a different type of radiation to brachytherapy known as proton radiation. The proton beams are aimed precisely at the cancer. This type of radiation reduces the risk of damage to the surrounding healthy eye tissue.
We have more information about radiotherapy to the eye area. It’s aimed at adults with eye cancer.
Surgery
Your child might need surgery to remove the eye (enucleation) if the cancer is large and the eye is no longer working. If your child has cancer in both eyes, they might remove the worst affected eye.
It can be devastating to find out your child needs to have their eye removed. Your child will usually recover and adapt quickly. And it doesn’t usually stop them from doing what they want to do.
After removal of the affected eye the surgeon fits an implant which is like a small ball to replace the lost eye. This will fill their eye socket. It’s attached to the muscles, so it moves in sync with the other eye.
Your child also has an artificial eye (prosthesis) made to cover the implant. This will match their original eye and is like a large contact lens. Your child usually has this fitted a few weeks after surgery.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. Your child might have their chemotherapy in one or more of the following ways:
- into their bloodstream (intravenous) through a long flexible plastic tube (systemic chemotherapy)
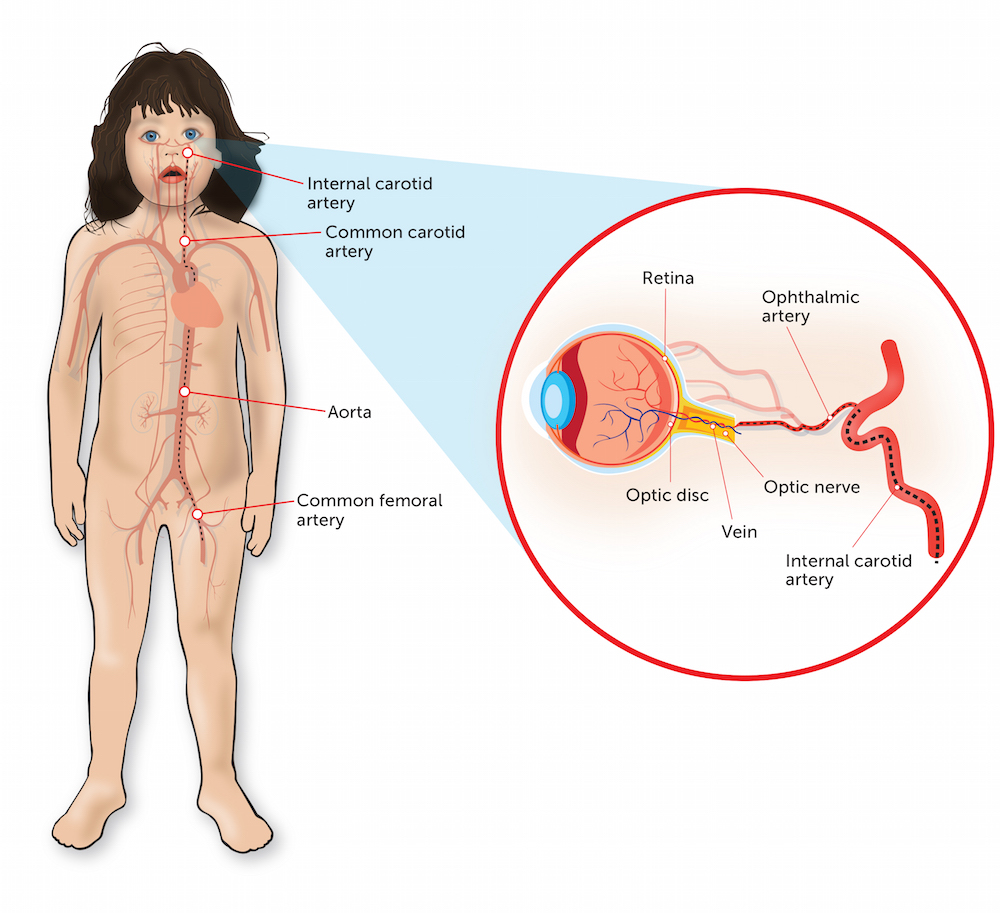
- through a blood vessel (artery) to the affected eye (intra arterial chemotherapy or IAC)
- as an injection directly into the jelly part of the eye (vitreous)
Your child might have chemotherapy to try and shrink the cancer first if it is large. They might have this before a local treatment such as laser therapy.
Your child’s doctor might suggest chemotherapy if there is any risk that the cancer might have spread. They usually have a combination of chemotherapy drugs. Doctors commonly use a combination called CEV also known as JOE. This includes:
- carboplatin
- etoposide
- vincristine
This combination is given in cycles  of treatment. Your child might have between 4 to 6 cycles. Each cycle lasts between 3 to 4 weeks.
of treatment. Your child might have between 4 to 6 cycles. Each cycle lasts between 3 to 4 weeks.
Other chemotherapy drugs used for systemic chemotherapy include:
- cyclophosphamide
- ifosfamide
- doxorubicin
- topotecan
If your child is having chemotherapy into a blood vessel or as an injection directly into the jelly part of the eye, they commonly have one of the following:
- melphalan
- carboplatin
- topotecan
Your child usually has chemotherapy into the blood vessel every 3 weeks. They have between 2 to 4 cycles. If they are having it into the jelly part of the eye, your child has between 2 to 6 cycles. The injection is every 7 to 14 days.
Side effects
The side effects of having chemotherapy into the artery or vitreous of the eye can be different to those intravenous chemotherapy. These might include side effects such as:
- inflammation
- droopy eyelid
- squint
These are usually temporary. There can also be a risk of reduced vision.
Your child’s doctor will go over the possible risks of having chemotherapy into the eye with you.
Going to sleep (general anaesthetic)
Your child will receive most of their treatment, tests or scan while they are asleep, unless they are having systemic chemotherapy.
To get your child to sleep a nurse or doctor puts a small tube (cannula) into your child’s hand or arm. The nurse first puts some local anaesthetic cream on the area to numb it. Your child might still feel the needle go in, but it shouldn’t be painful.
You can usually go with your child to theatre before the operation or examination. You wait with your child in a room next to the theatre, called the anaesthetic room. You can give your child a cuddle and reassure them until they are beginning to fall asleep.
The anaesthetist  gives your child the anaesthetic
gives your child the anaesthetic  through the cannula in their hand. Or, they gently place a mask over your child’s mouth and your child breathes in the anaesthetic gas until they fall asleep. A member of the team lets you know when the treatment, test or scan has finished.
through the cannula in their hand. Or, they gently place a mask over your child’s mouth and your child breathes in the anaesthetic gas until they fall asleep. A member of the team lets you know when the treatment, test or scan has finished.
It’s not unusual to feel very emotional seeing your child drift off to sleep. The theatre or ward team will take your mobile number to call you as soon as they are awake.
Side effects
Your child’s doctor will talk to you about the possible side effects. The side effects your child might have depend on the type of treatment they are having. Some of the possible side effects include:
Loss or changes to eyesight
Most parents worry about whether their child will lose their sight. Whenever possible, the doctor will try to keep the sight of the eye. Removing the affected eye will not cause sight loss in the other eye. Children learn to adapt very quickly and live a normal life, often going to mainstream school.
If your child has retinoblastoma in both eyes it’s possible that your child will lose some sight. This might mean they need to have visual impairment support, either within a mainstream school or in a specialist school.
Some treatments such as laser treatment might cause changes to their sight. Your child might complain that it’s not as bright as before. Other comments might be that they can see dots or lines (floaters) and flashes of light. Let their team know straight away if this happens.
Increased risk of infection
Chemotherapy can cause a drop in your child’s white blood cells. Symptoms include a change in temperature, aching muscles, headaches, feeling cold and shivery and generally unwell. Your child might have other symptoms depending on where the infection is.
You should contact your child’s advice line urgently if you think they have an infection.
Hearing changes
Some chemotherapy drugs such as carboplatin and cisplatin can cause changes to your child’s hearing. They might have hearing tests before these types of drugs. Let your child’s doctor or nurse know if you or your child notices anything different with their hearing.
A second cancer
Although the risk is very small, chemotherapy can cause them to develop a second cancer many years into the future. If your child has an inherited retinoblastoma second cancers can occur in later life. Your child’s doctor will talk this through with you and answer any questions you may have about it.
Trilateral retinoblastoma is very rare type of cancer and children with inherited retinoblastoma can develop this. It starts in the centre of the brain, from the pineal gland  . The pineal gland is just behind the brain stem. It makes the hormone melatonin that controls sleep. Symptoms include headaches and feeling and being sick.
. The pineal gland is just behind the brain stem. It makes the hormone melatonin that controls sleep. Symptoms include headaches and feeling and being sick.
Your doctor will talk to you about this if your child is at risk. They will monitor your child very closely.
Retinoblastoma that has come back or not gone away
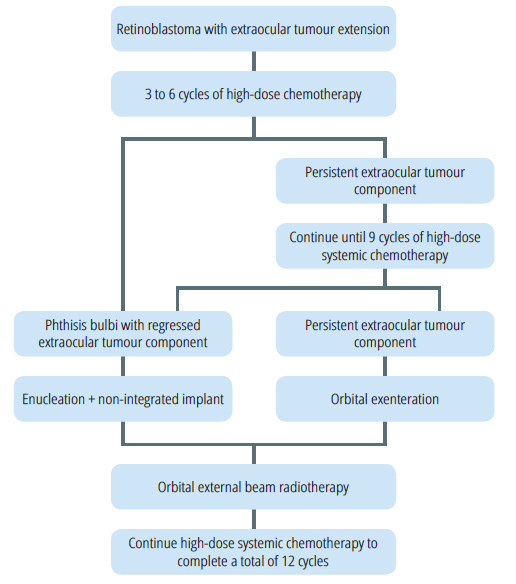
Almost all retinoblastomas are successfully treated. But some cancers can come back again (recurrence or relapse) or don’t go away (refractory). Your child’s doctors will develop a treatment plan. This will depend on:
- what treatment they have already had
- where the cancer is
- the size of the cancer
- how far it has spread
- your child’s general health
Your child’s healthcare team will explain the different treatment options and support you through this difficult time.
Follow up
Your child will have regular follow up appointments with their specialist. They are very close together to start with and then get gradually further apart as time goes on. These appointments are to check:
- how they are recovering
- their development
- if they are having any problems following treatment
- if there are any signs the retinoblastoma has come back
These appointments usually include your child having a general anaesthetic for a close look at their eyes.
Coping when your child has cancer
It is understandably devastating when a child is diagnosed with cancer. Although many children with cancer are successfully treated, it is a difficult time for everyone affected.
As well as the doctors and nurses on the ward, you and your child will be supported by a number of professionals during and after treatment. These include your GP, cancer nurse specialists, social workers, play specialists and a psychologist or psychotherapist.
Talking to other people who are experiencing the same thing can also help. Our discussion forum Cancer Chat is a place for anyone affected by cancer. You can share experiences, stories and information with other people who know what you are going through.