Prehabilitation (prehab) means getting ready for cancer treatment in whatever time you have before it starts. It is a programme of support and advice that some NHS hospitals are using. It covers three particular parts of your health:
- what you’re eating and your weight
- physical activity or exercise
- mental wellbeing
Stopping smoking and cutting down on alcohol can also help. It helps while you’re having treatment, with your recovery, as well as improving your overall health.
How does prehabilitation help?
At diagnosis, your medical team should screen you for any problems in the three areas above. Research shows that if you get support early on and are as healthy as possible, you are more likely to:
- leave hospital sooner after surgery
- cope better with the side effects of cancer treatment
- have fewer side effects
- have more treatment choices
- have better long-term health
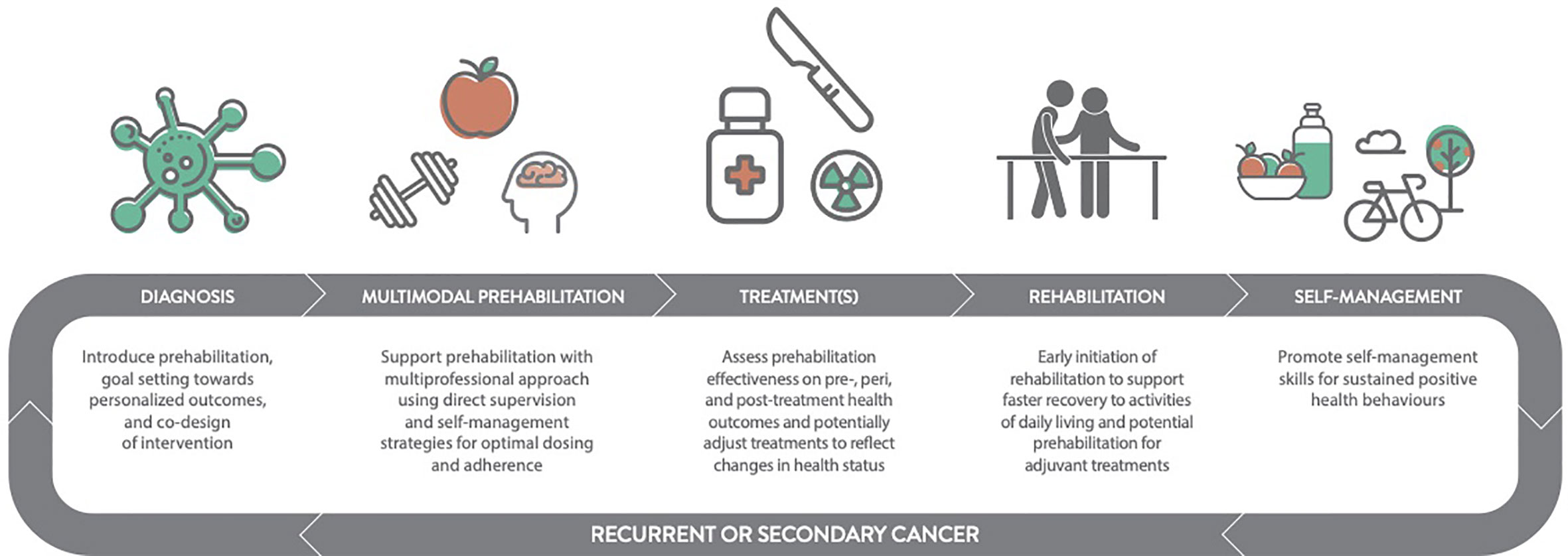
Prehabilitation plays a role in all your cancer care. That includes diagnosis, treatment and follow up. It continues as rehabilitation as part of your recovery package.
Feeling more in control
Following a prehabilitation programme can help you feel more in control of your physical and mental health. You can cope better during treatment and recover better if you are in control. By continuing to take care of your diet, physical fitness and mental health, you can live well in the long term.
Is there prehabilitation in every hospital?
At the moment, not everyone having cancer treatment will have prehabilitation. Research shows that it is helpful for people having surgery. But researchers think it might also help people having other cancer treatments. These are treatments such as chemotherapy and radiotherapy.
You might have prehabilitation at your cancer hospital or a local leisure centre as part of a:
- NHS programme or service
- research trial
Some hospitals offer it to people with certain types of cancers. These cancers include:
- upper GI (gastrointestinal)
- lung
- bowel
- prostate
But it is not available in every hospital at the moment. And there are differences depending on which UK nation you live in.
What happens if I’m not offered prehabilitation?
Not having prehabilitation will not affect the treatment you have for your cancer. You will still have the best possible treatment. Knowing about it can help you see what you can do to be in the best health possible before starting treatment.
So, before you start treatment, talk to your doctor, specialist nurse or other members of your healthcare team. Tell them if you’re worried about your diet, physical fitness or mental health. They can give advice or may refer you to a specialist.
How does prehabilitation work?
There are 4 stages to prehabilitation:
- screening
- assessment
- intervention
- monitoring
Screening
Screening means the team caring for you will look at:
- your weight, whether you have had any weight loss or weight gain recently, as well as your ability to eat and drink
- how physically active and strong you are
- your mental well being
Screening aims to find problems as early as possible and get you as fit as possible for treatment. This means that you might have screening for prehabilitation at the same time as you are having tests to diagnose your cancer.
Everyone with a cancer diagnosis has a Holistic Needs Assessment (HNA). The HNA is a questionnaire that looks at your needs as a whole person and not just your cancer. The HNA shows what needs you might have during your cancer treatment. Your medical team can use it as part of prehabilitation screening.
You will also have screening with several other questionnaires.
If your screening shows that you are fine, your team will ask you to focus on three lifestyle behaviours until you start cancer treatment. These are also called universal interventions (see below). They are:
- eating a wide range of foods in the right proportions, also called a varied diet
- being more physically active and doing exercises
- looking after your mental wellbeing
Assessment
Depending on the results of your screening, your medical team will assess your needs. They might ask you more about your history, examine you or do other special tests if they want to know more.
They may refer you to specific ‘prehab’ teams. They can be in the hospital or community. They will do the assessments. The teams can include:
- exercise specialists
- physiotherapists
- occupational therapists
- dietitians
- other NHS staff
So, if your screening shows that you might not be very fit, you will have a physical fitness assessment. This might be:
- a 6 minute walk test
- an incremental shuttle walk test – a test that looks at how far you can walk, with the pace increasing gradually every minute at the sound of a beep
And if it shows you could have problems to do with your diet, you will have a nutritional assessment. This is to make sure you are getting enough of the types of food necessary for good health.
The team will also want to know your weight and the amount of fat and muscle (body composition) in your body. This is so that your body is in the best condition possible before treatment.
You will have an assessment of your psychological needs if it shows that your mental health is at risk. Your HNA will give the team more information on these needs.
The results of these assessments will show your medical and prehab teams:
- what your needs are
- how much support you might need
- what the best methods are for improving your physical, nutritional and mental health in the time before treatment
Intervention
An intervention means helping you to cope with and recover from treatment. Not everyone will have the same needs. And how much support you need might also differ from others. So, your team will look at your specific situation.
There are 3 types of interventions you might have:
- universal
- targeted
- specialist
Universal interventions
Universal interventions are for anyone with cancer and their families. It focuses on three lifestyle changes, namely diet, physical activity and mental health. It also focuses on other areas of your health which you can change when living with cancer. Focusing on your behaviour in these areas can help you to live well in the long term.
The other areas of health are:
- keeping to a healthy weight
- stopping smoking
- drinking alcohol within the suggested limits
This might include your team talking to you about a particular area of your health. They might give you information or signpost you elsewhere, such as a stop smoking service. Or they might ask you to look at websites, use apps or watch videos.
It might be that you only need universal interventions to support you.
Targeted interventions
A targeted intervention is planned support from an expert. They aim to help you make a change in a particular area of your health. They are for people with cancer who:
- are at risk of long-term (late) effects of treatment
- have other long-term health conditions
- need extra support to successfully do their recommended prehab activities
Your team might refer you to an exercise class if you need support with physical activity. This might be a group class or a one to one class. The class might be at a local gym with a cancer exercise specialist. Or it might be doing exercises with someone through a video call.
For problems with diet, a dietitian can tell you what to do and guide you. They can help with diet problems because of your cancer or conditions such as diabetes.
Good muscle strength is important before you start treatment. The advice on diet and exercise will help with this.
Some people need support to help them deal with specific areas of mental health. This might include dealing with anxiety, a low mood or problem solving. A healthcare professional with training in one of these areas can support you.
Exercise and continuing your daily activities can help support your mental health when dealing with a cancer diagnosis.
Specialist interventions
Specialist interventions are for people with cancer whose assessment showed you:
- have complex needs
- are having major treatment
- have severe changes because of treatment
- have a disability
- are at higher risk of having problems if they try to do the prehab activities
So, if you can’t do much physical activity, you might need specialist support. A qualified cancer exercise professional and physiotherapist at the hospital or a local leisure centre can help you.
Some people might have more complex diet problems, such as:
- difficulty swallowing
- weight loss
- changes to how their digestive system works
In these situations, a dietitian might prescribe you diet support. These can be:
- food through a tube into their stomach (enteral nutrition)
- intravenous (drip) feeds called parenteral nutrition (PN)
A counsellor or psychologist can offer help if you have problems to do with your mental health. Some people need specialist therapy or psychiatric support. Support from a specialist is important if you have been suffering from a mental health problem before your cancer diagnosis.
You might need a mix of different levels of support. Universal interventions might support some of your needs. But other problems might need targeted or specialist interventions. You might also move between interventions over time.
It is important that your prehab team know how much you can do, as well as what your needs and wishes are. They will adapt your prehab activities accordingly.
Monitoring
Monitoring your progress when doing the prehab activities is important. This is before and after treatment. It will help the prehab team to understand:
- what changes (if any) are happening
- how this relates to your cancer treatment
- whether they need to change anything
How much monitoring you need will depend upon whether you are doing your prehab interventions:
- independently (universal)
- with regular support from your prehab team (targeted or specialist)
Prehab teams are interested to know how the activities have been helping you. This will help them to show the importance of it and that more people should have it.
So, monitoring not only helps to understand what is happening to you, but can help other people affected by cancer in the future.