What is thalassaemia?
Thalassaemia is an inherited genetic disorder that affects the blood and causes lifelong anaemia.
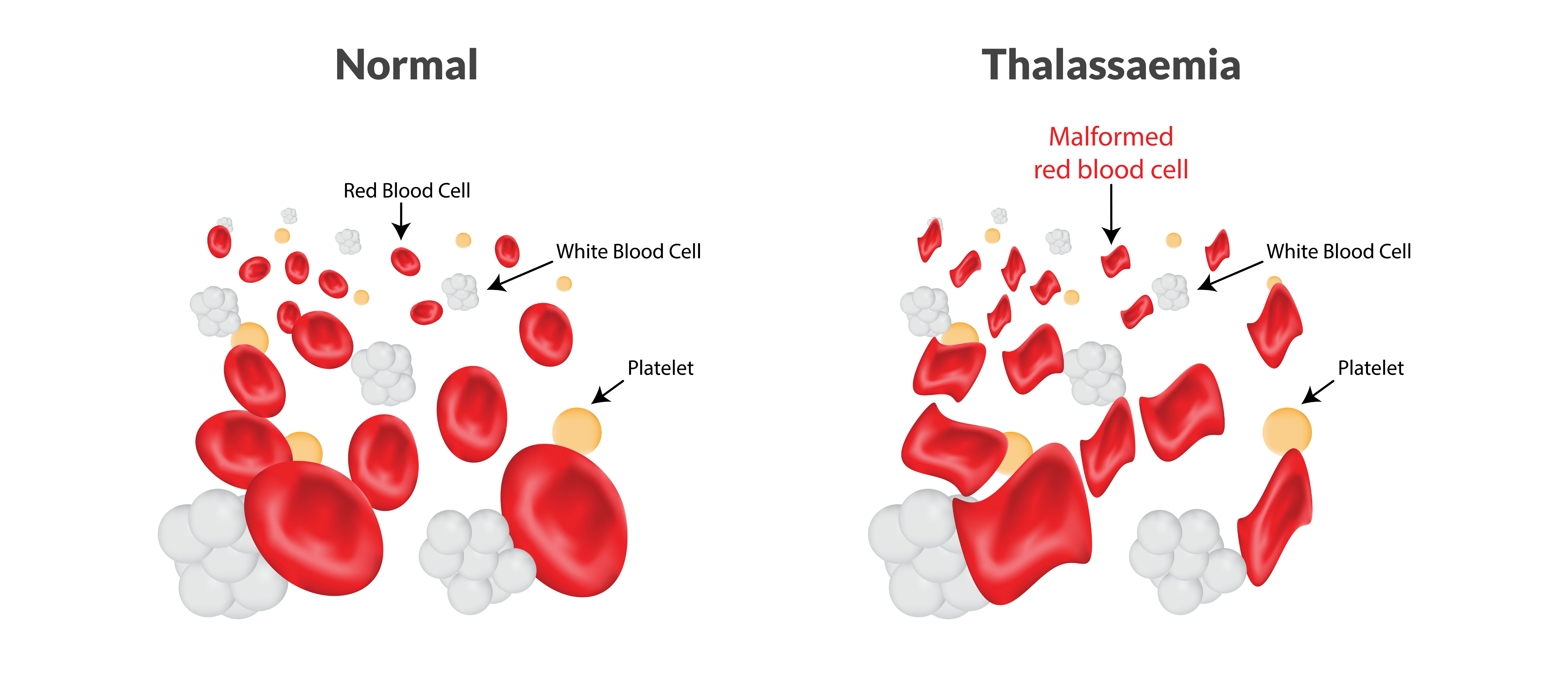
People with thalassaemia do not produce enough healthy haemoglobin, which makes their blood cells small and pale. Haemoglobin is a protein found in red blood cells that carries oxygen from the lungs to the rest of the body.
People born with thalassaemia cannot move oxygen around the body properly. Depending on the type of thalassaemia they have, they may need regular blood transfusions to stay alive.
What causes thalassaemia?
Thalassaemia is caused when someone inherits gene mutations (‘spelling errors’ in the DNA in genes) from one or both parents. These gene mutations make the body lose red blood cells more quickly than normal and result in less haemoglobin.
There are different types of thalassaemia. The type someone has depends on which gene mutations they inherit.
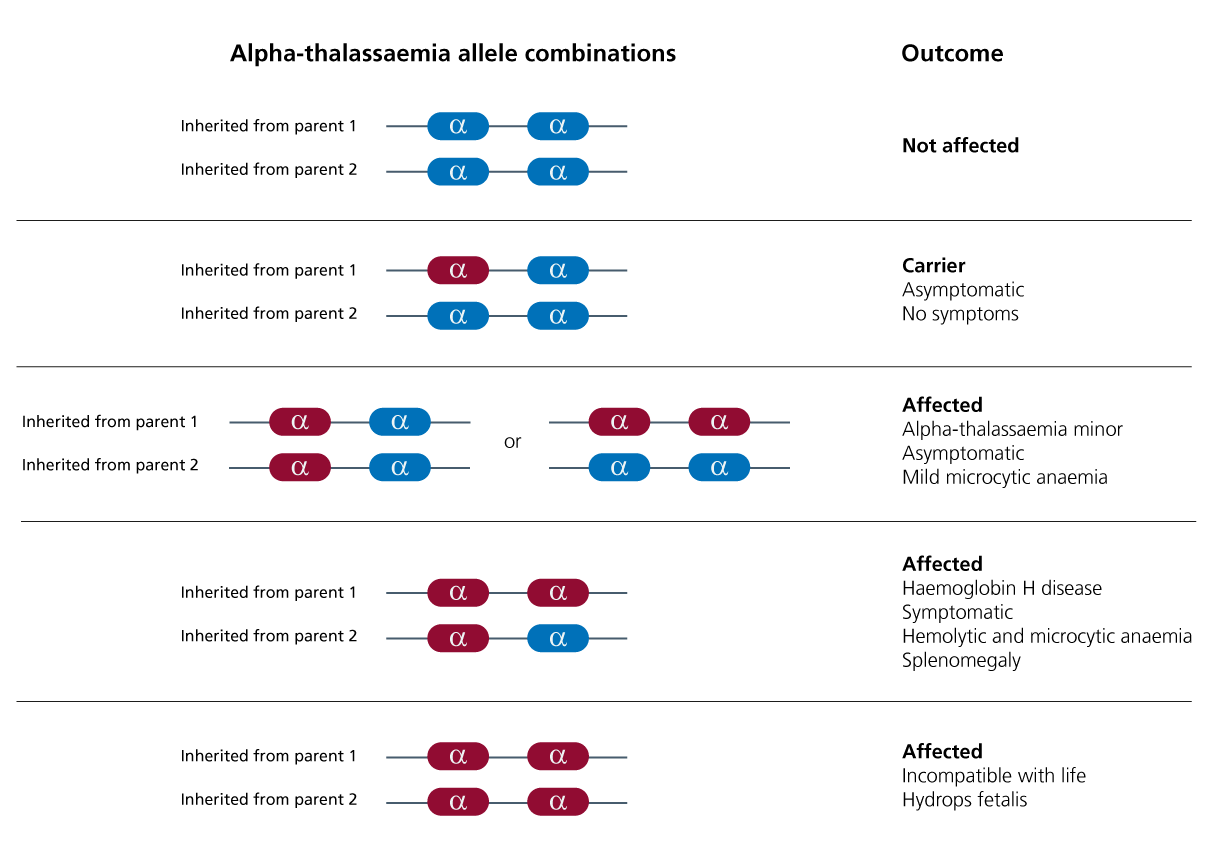
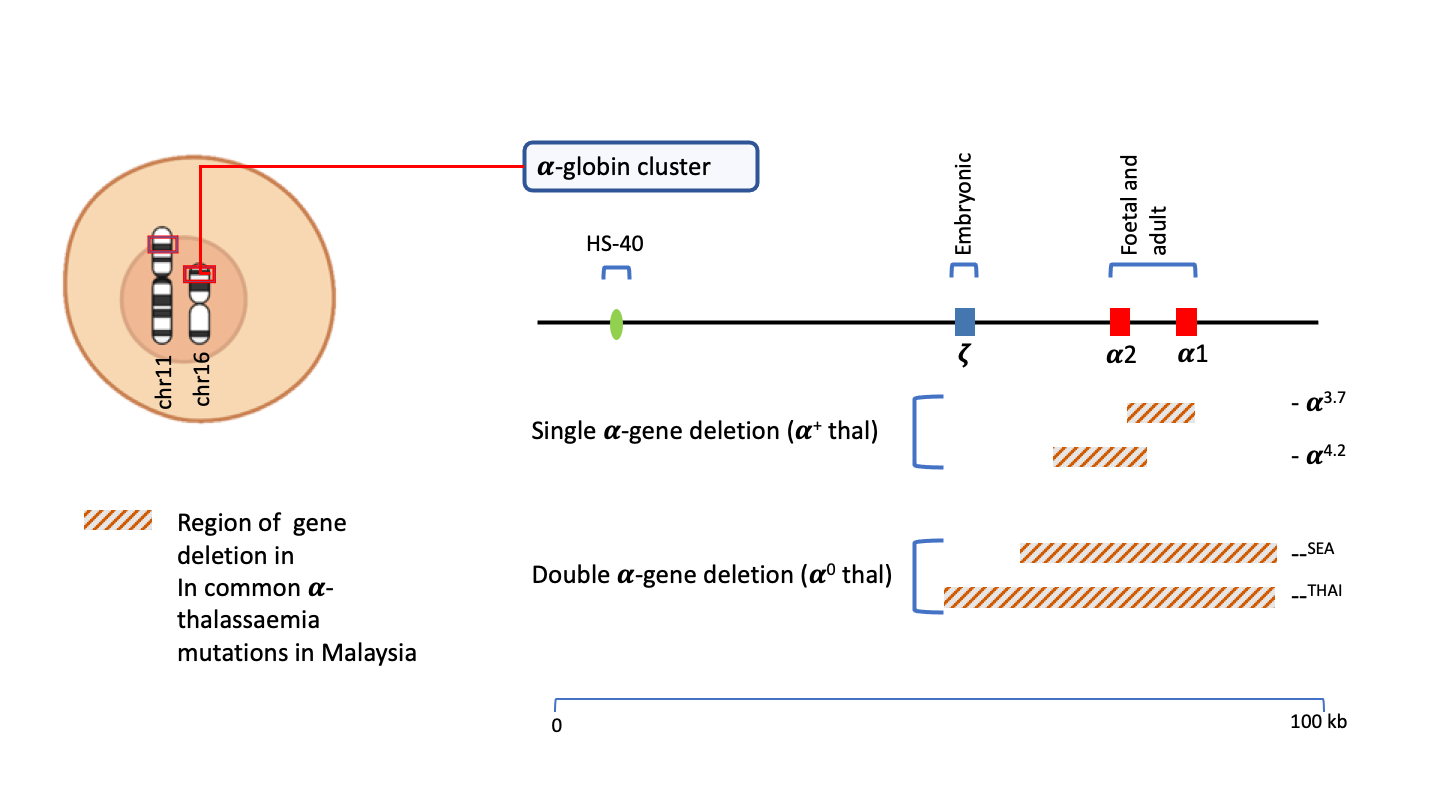
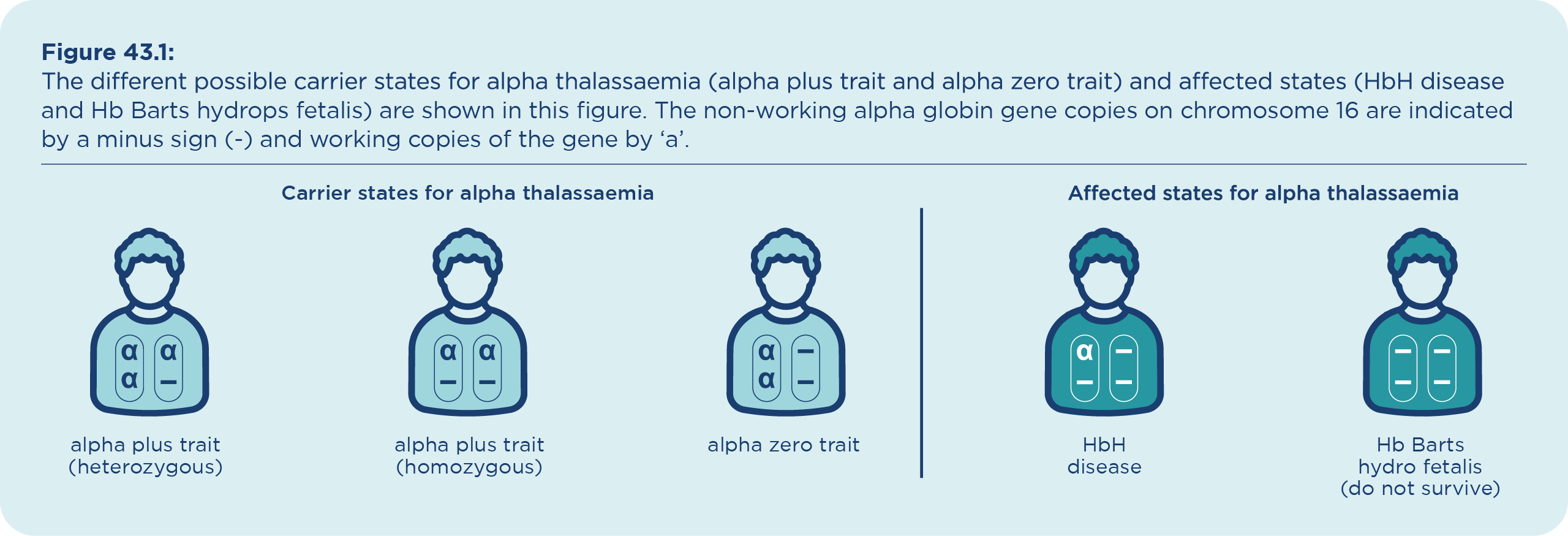
Alpha thalassaemia: This is caused by a problem in 1 or more of 4 genes called alpha globin genes.
People who inherit just 1 gene may not have any symptoms, but they can still pass the disorder onto their children. 2 genes cause mild symptoms, 3 genes (called Haemoglobin H disease) cause more severe symptoms, and babies who inherit 4 genes (called alpha thalassaemia major or hydrops fetalis) are usually very sick and do not live for long after they are born.
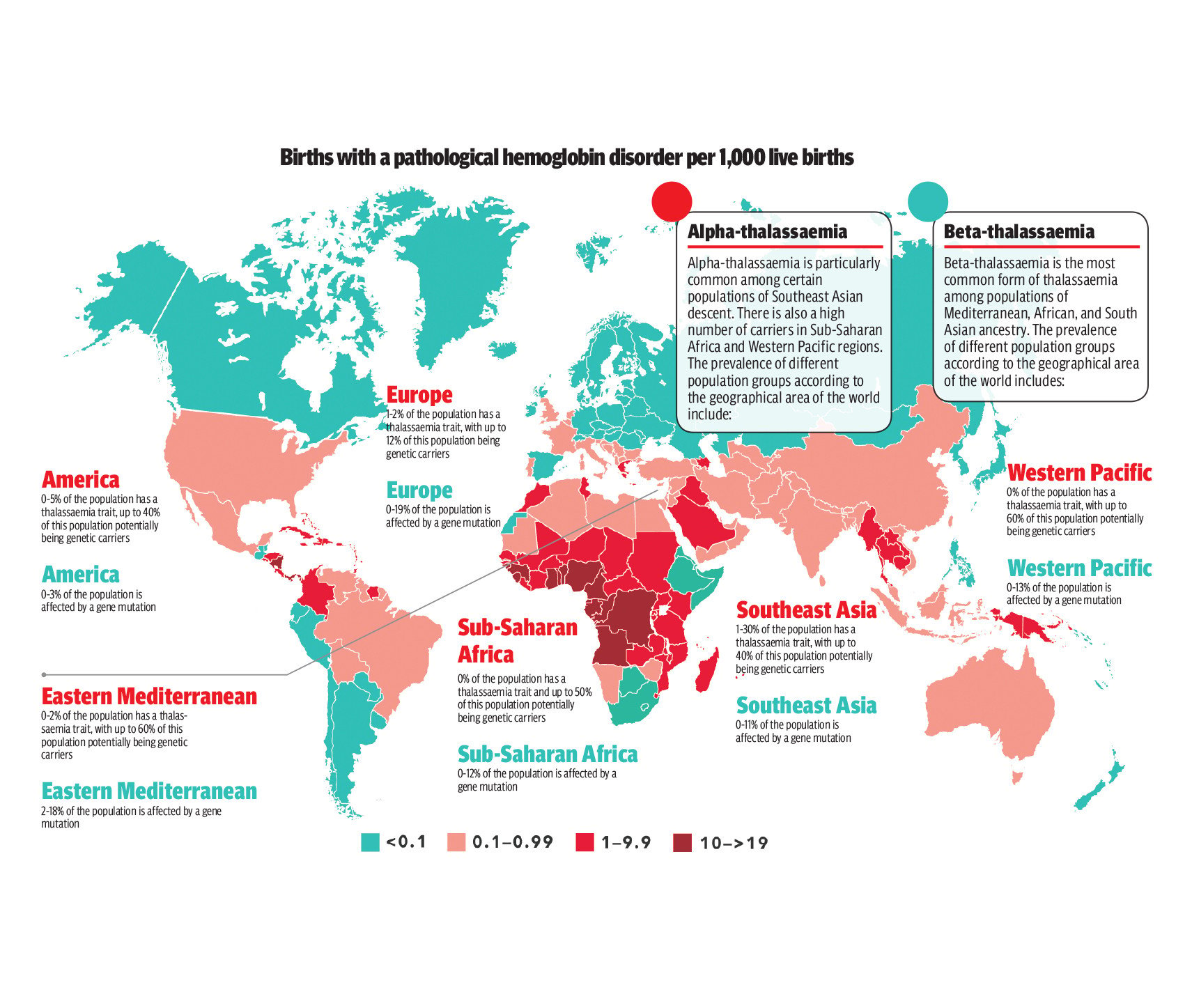
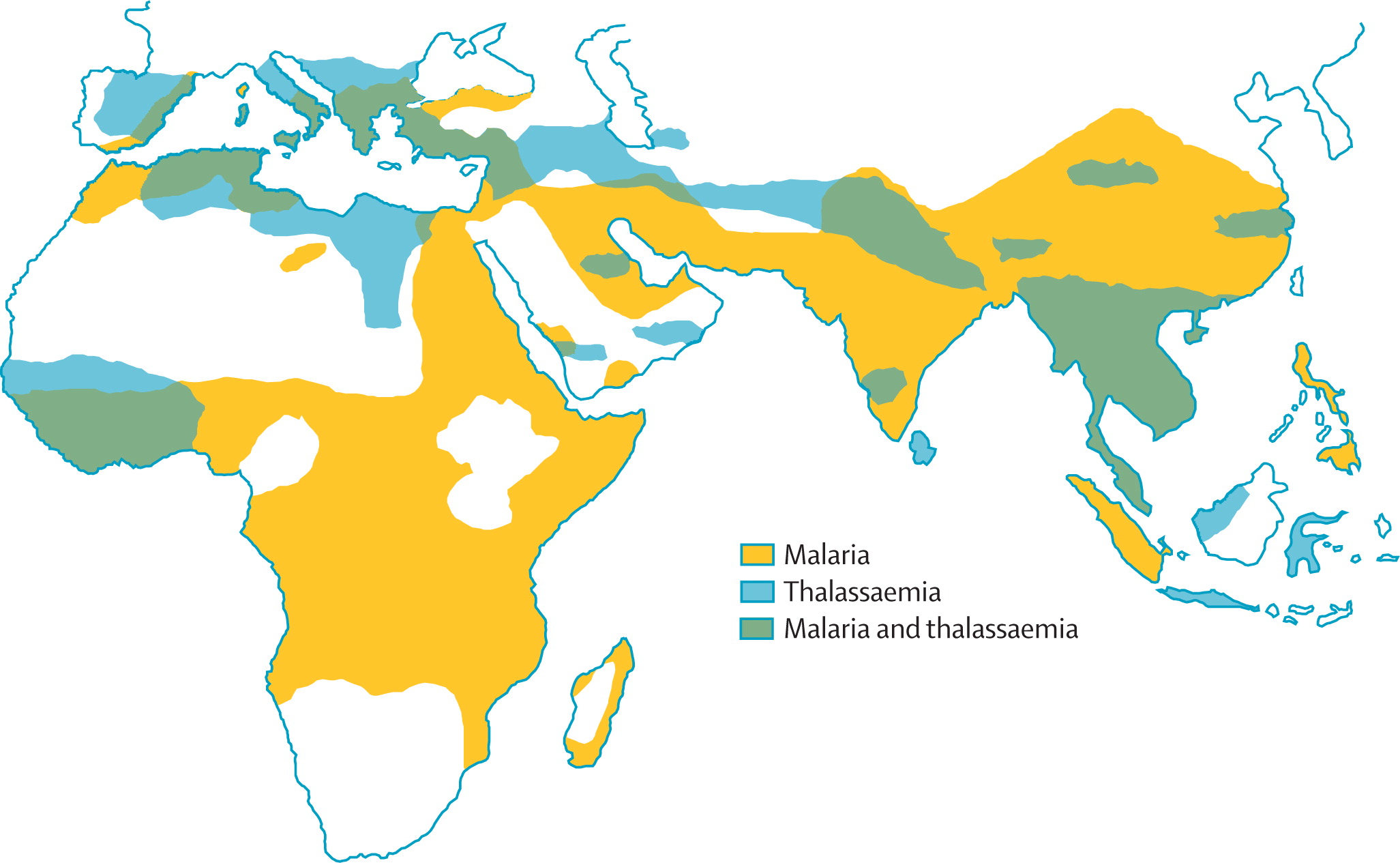
Alpha thalassaemia more common in people of Southeast Asian, Southern Chinese, Middle Eastern, Indian, African or Mediterranean descent.
Beta thalassaemia: This is caused by mutations in 1 or 2 genes called beta globin genes.
There are hundreds of possible mutations and symptoms depend on which mutation a person has. People with just 1 faulty gene usually have minimal symptoms but they can pass thalassaemia onto their children. People with 2 faulty genes (called thalassaemia major) often have life-threatening symptoms. Some people with 2 abnormal genes may still have milder symptoms and only need occasional blood transfusions.
Beta thalassaemia usually affects people of Mediterranean, Asian or African descent.
What are the symptoms of thalassaemia?
People with thalassaemia can:
- feeel tired, weak, dizzy and short of breath
- grow more slowly than usual as children
- be pale or have yellow skin colouring (jaundice)
- have dark urine
- have a swollen belly
- have slight deformity of their facial bones
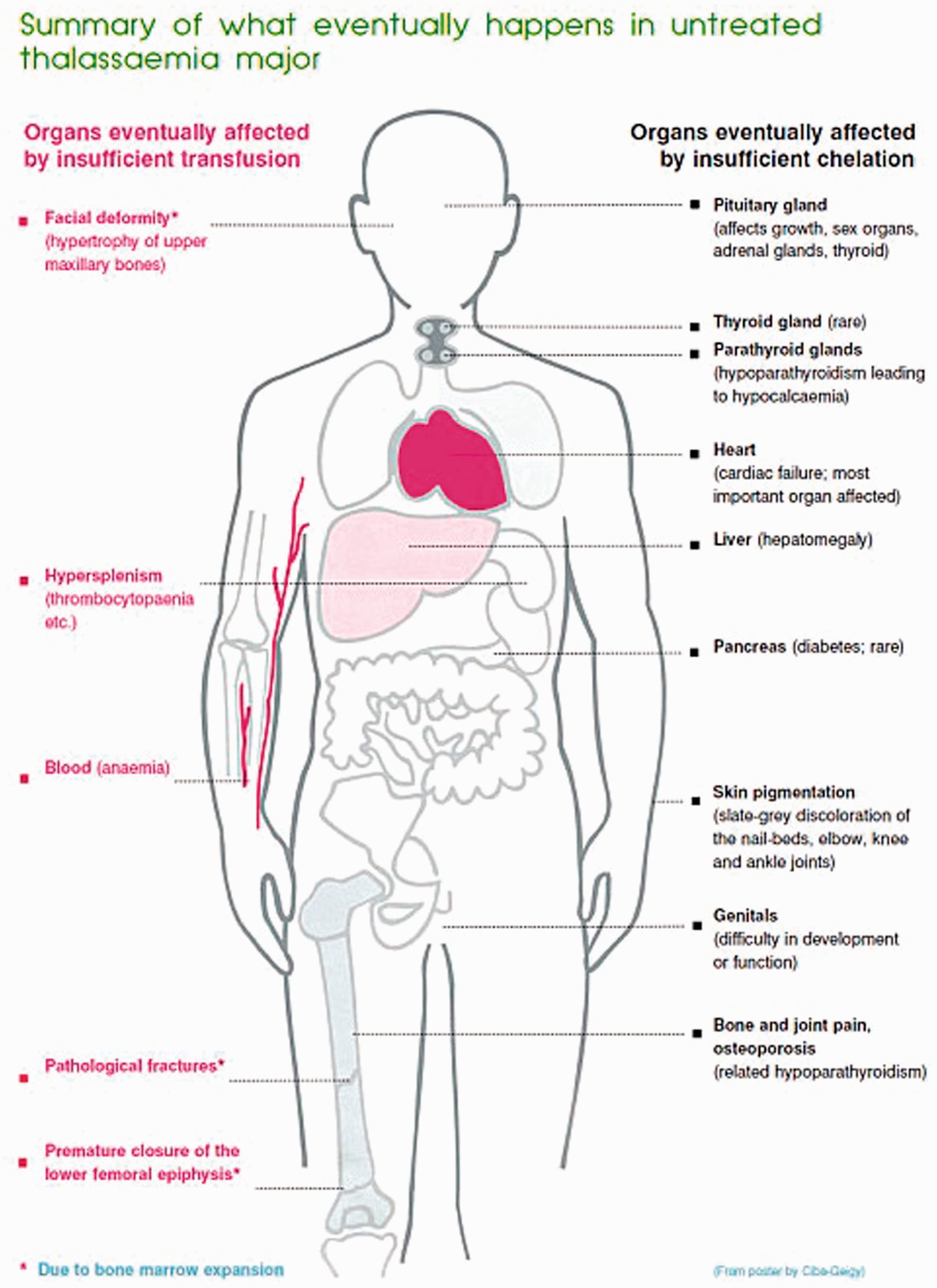
If it’s not treated, thalassaemia can lead to heart failure and infections.
The symptoms can show up in babies and small children if the condition is severe, usually in the first 2 years of life.
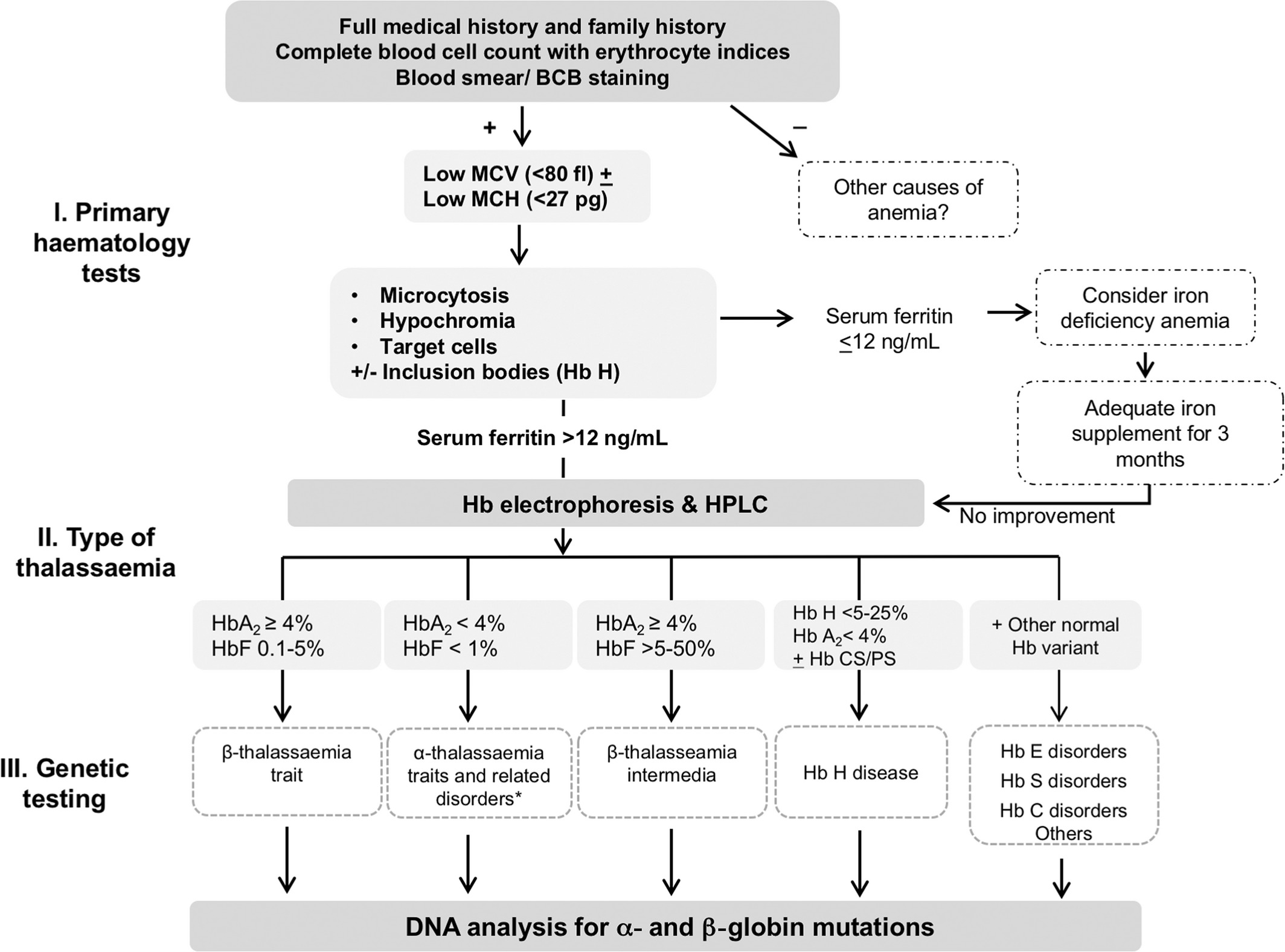
How is thalassaemia diagnosed?
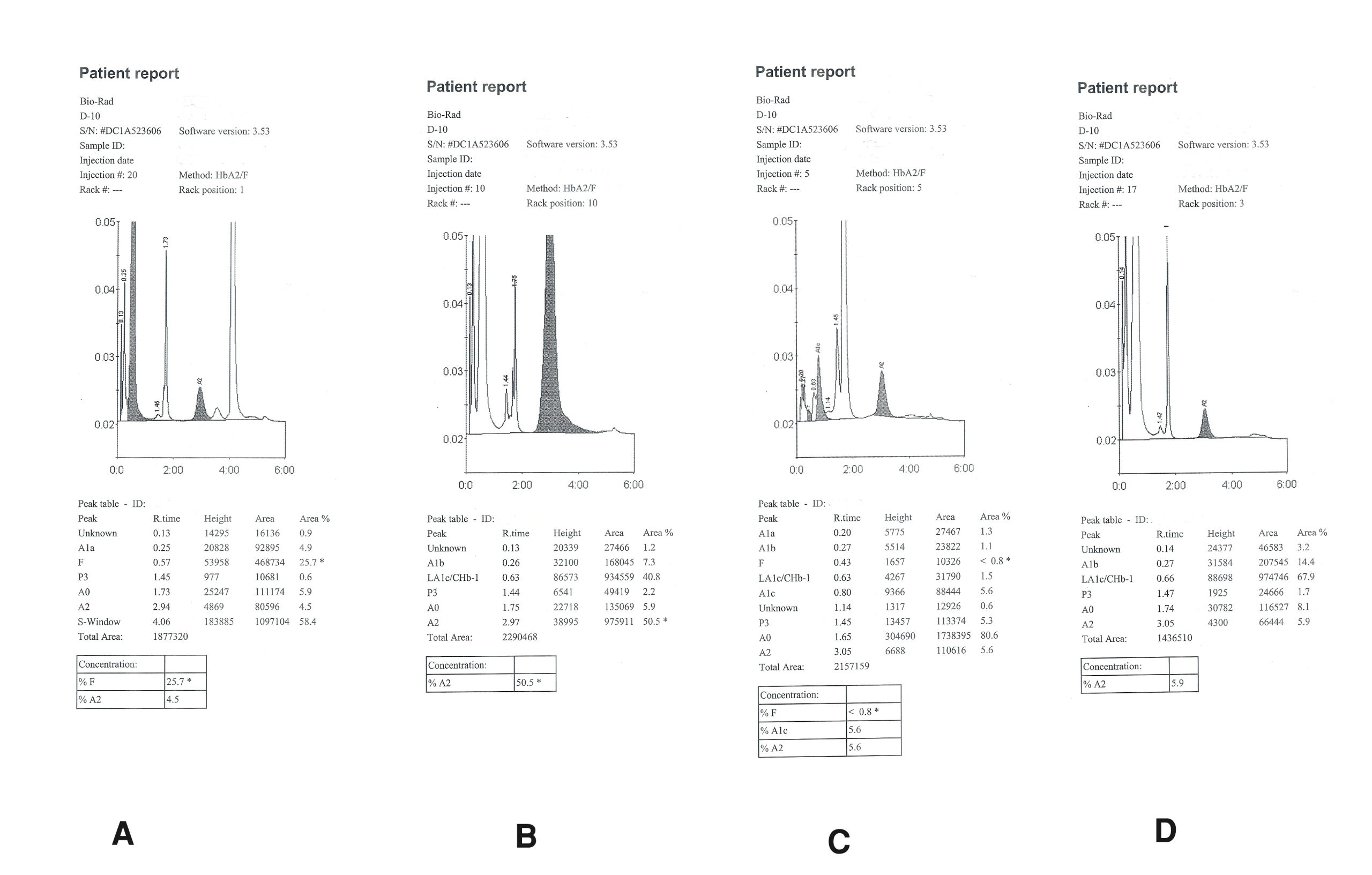
Some people find out they have thalassaemia because they are unwell. Their doctor talks to them, examines them and carries out blood tests. They may also have genetic tests.
Other people find out they have thalassaemia by chance, when a blood test done for other reasons shows something unusual.
There are times when doctors suggest a blood test to check for thalassaemia. This includes if:
- you are planning to have a child
- you have a relative with thalassaemia
- you or your relatives have unexplained anaemia (low haemoglobin)
- your family came from a region where thalassaemia is common
Unborn babies can also be tested for thalassaemia.
How is thalassaemia treated?
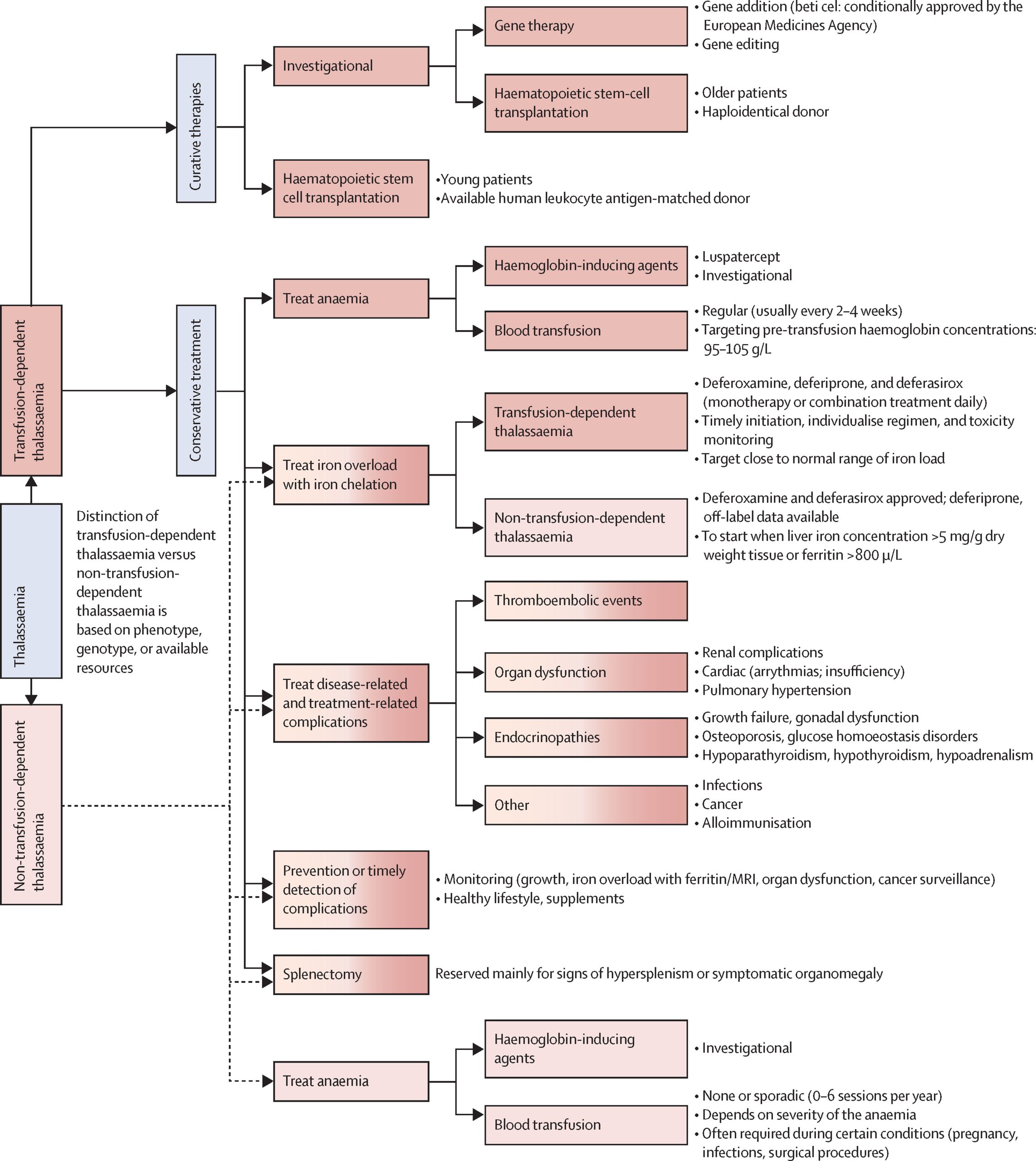
If you have thalassaemia, you might or might not need any treatment. It depends on how severe your symptoms are.
People with severe thalassaemia may need blood transfusions every 3 to 4 weeks. People with less severe thalassaemia might need blood transfusions only occasionally, or not at all.
Blood transfusions can cause a build-up of iron in the body, which can lead to heart and liver damage. People with frequent blood transfusions can take a medicine that helps bring the iron back to a safe level (called iron chelation).
A few people have so serious a problem that they are advised to have a transplantation of stem cells or bone marrow from a healthy donor. This can help, but it has risks and is only rarely needed.
Living with thalassaemia
If you have thalassaemia, it is important to attend all your medical appointments and to have blood transfusions when you need them. You will need to prevent infections by washing your hands often and avoiding people with colds or the flu.
Take care of yourself by eating healthily.
What are the complications of thalassaemia?
People with thalassaemia can develop other problems including:
- enlarged spleen
- blood infections
- bone problems such as deformities in the face or skull, or osteoporosis
- damage to the heart, liver or hormonal system, caused by too much iron in the blood
Can thalassaemia be prevented?
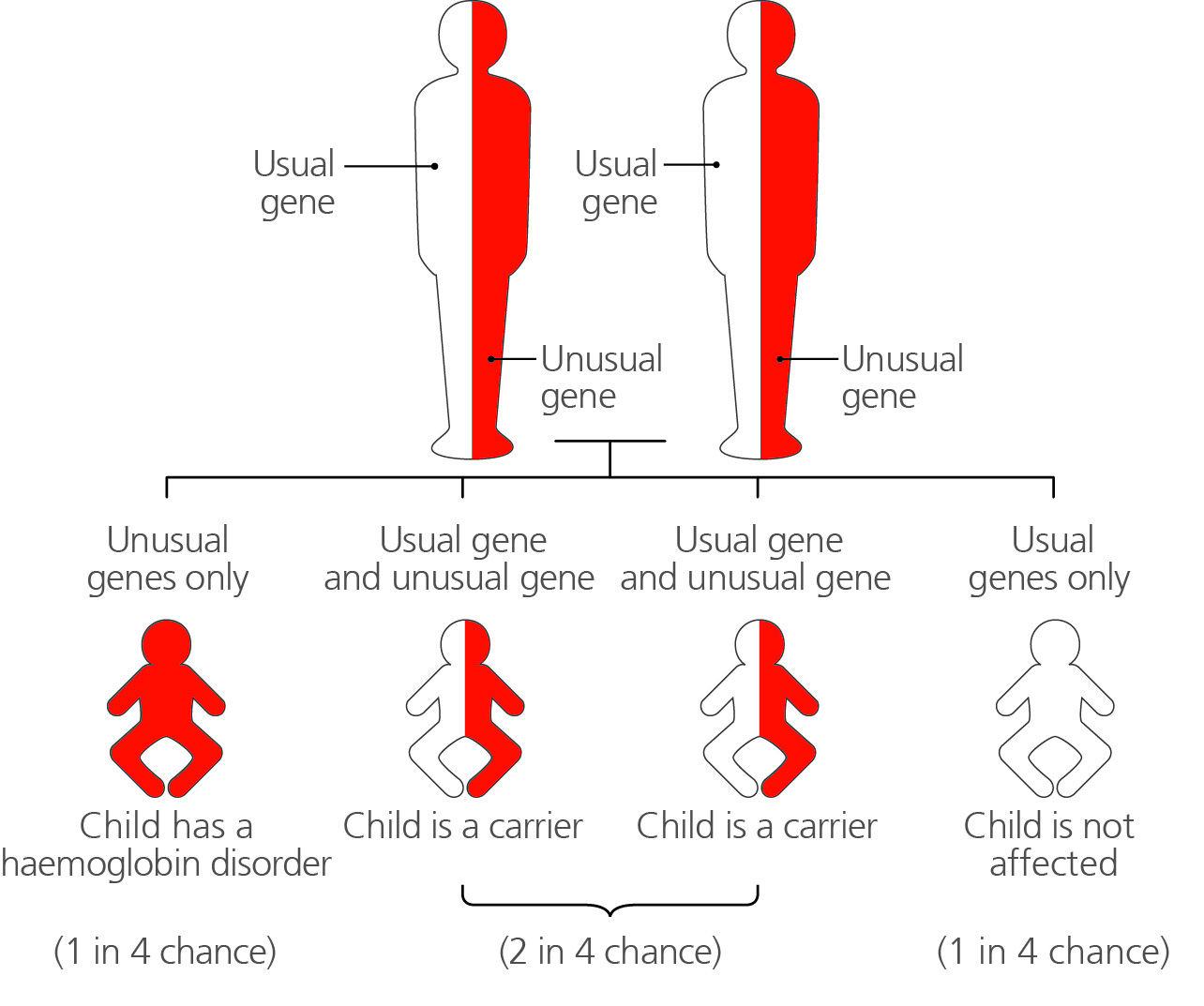
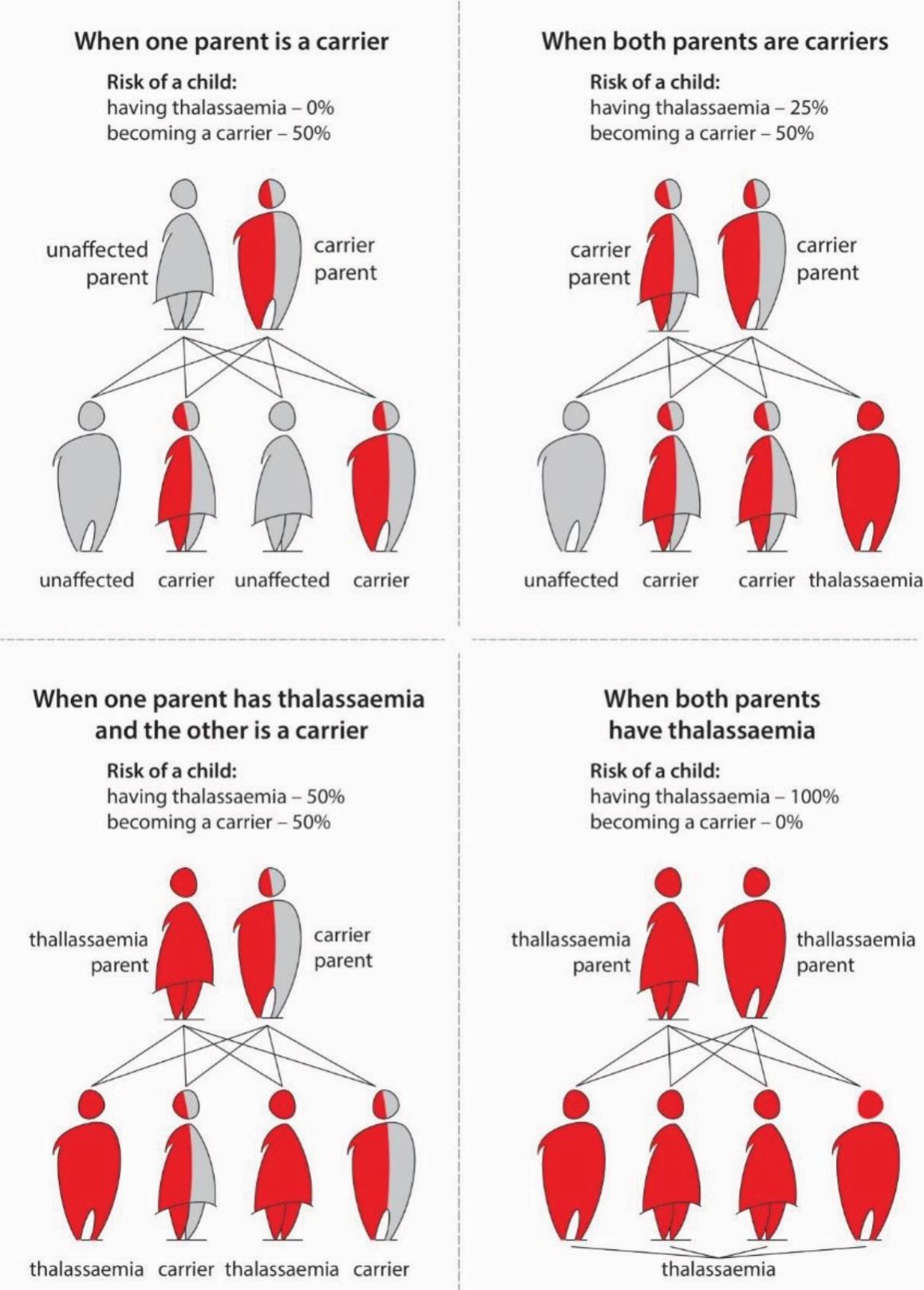
When someone is diagnosed with thalassaemia, their close relatives (parents, children, brothers and sisters) may also be offered genetic testing to see if they have the gene mutation. It is a simple blood test that is free and can be done by your doctor.
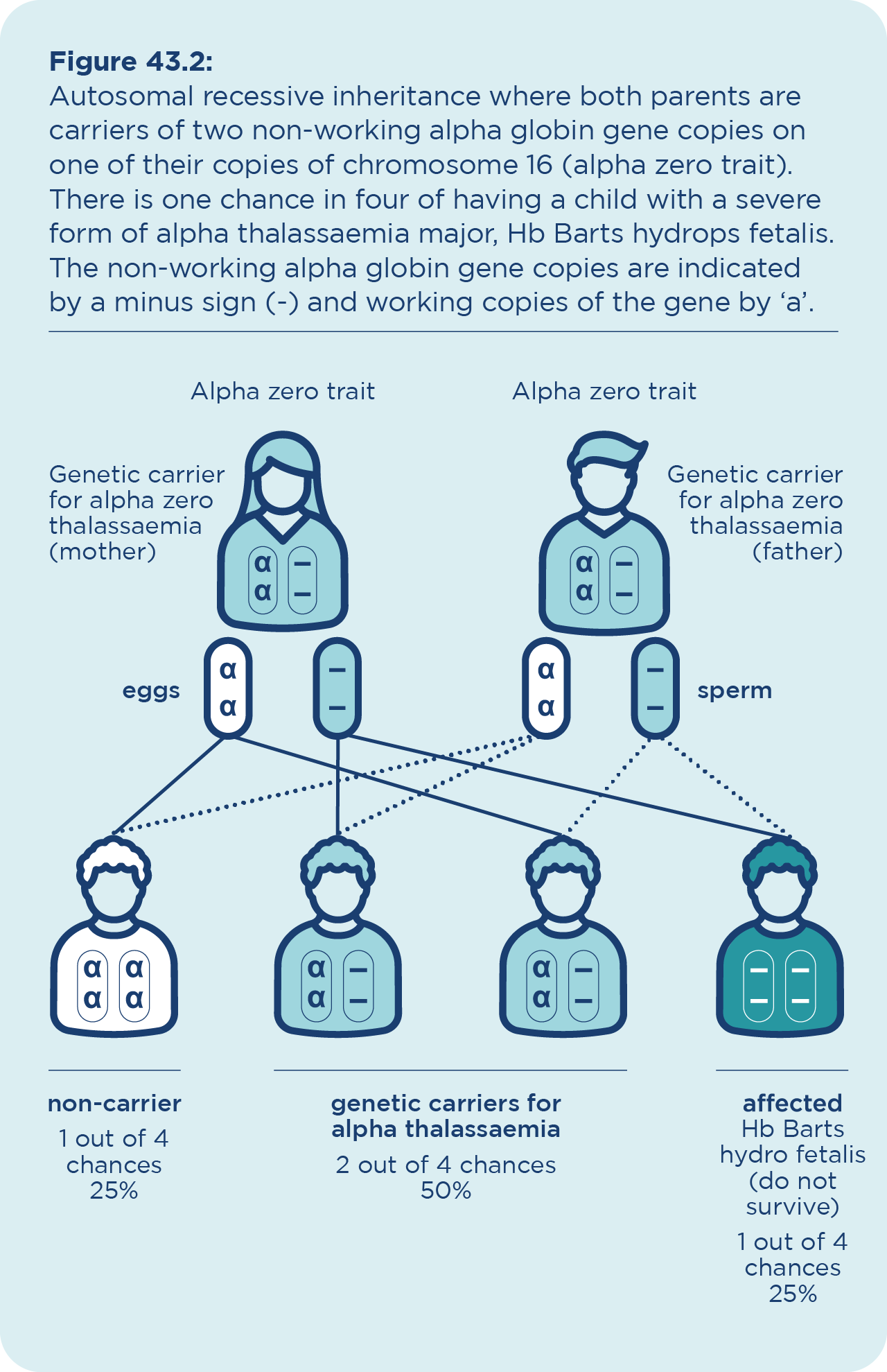
You might want to know whether you carry the gene so you can make informed choices about having a baby in future. A child is only at risk of having thalassaemia if both parents are carriers. If both parents are carriers, there is a 1 in 4 chance their child will have thalassaemia. There is a 1 in 2 chance they will be a carrier.
If you carry the thalassaemia gene and are thinking of having a child, you and your partner may decide to:
- have prenatal testing (a genetic test done during pregnancy) to see whether the child is affected
- think about your options for having a child. For example, you may decide to have a child through IVF, and have genetic screening of the embryo before it is implanted
- look out for symptoms of thalassaemia in your child
This Centre for Genetics Education fact sheet has more information about genetic screening in pregnancy for thalassaemia.