
Key facts
- Pneumonia is an infection in your lungs.
- Pneumonia can be life-threatening for babies, young children and people older than 70 years.
- Treatment will depend on whether your pneumonia is caused by bacteria or a virus.
- There are vaccinations available that can help prevent some types of pneumonia.
What is pneumonia?
Pneumonia is an infection of the lungs. The infection is usually caused by bacteria or a virus.
The infection causes inflammation (swelling) in your lungs. The air sacs in your lungs can fill up with fluid, making it harder for you to breathe.
There are many types of pneumonia. One of the most common is pneumococcal pneumonia. This is caused by the bacterium streptococcus pneumoniae.
Pneumonia can be a mild illness, or it can be much more serious. Pneumonia can be life-threatening, especially for:
- babies 12 months and under
- Aboriginal and/or Torres Strait Islander people
- people older than 70 years
If you are recovering well from a cold or flu that then becomes worse, it may be pneumonia.
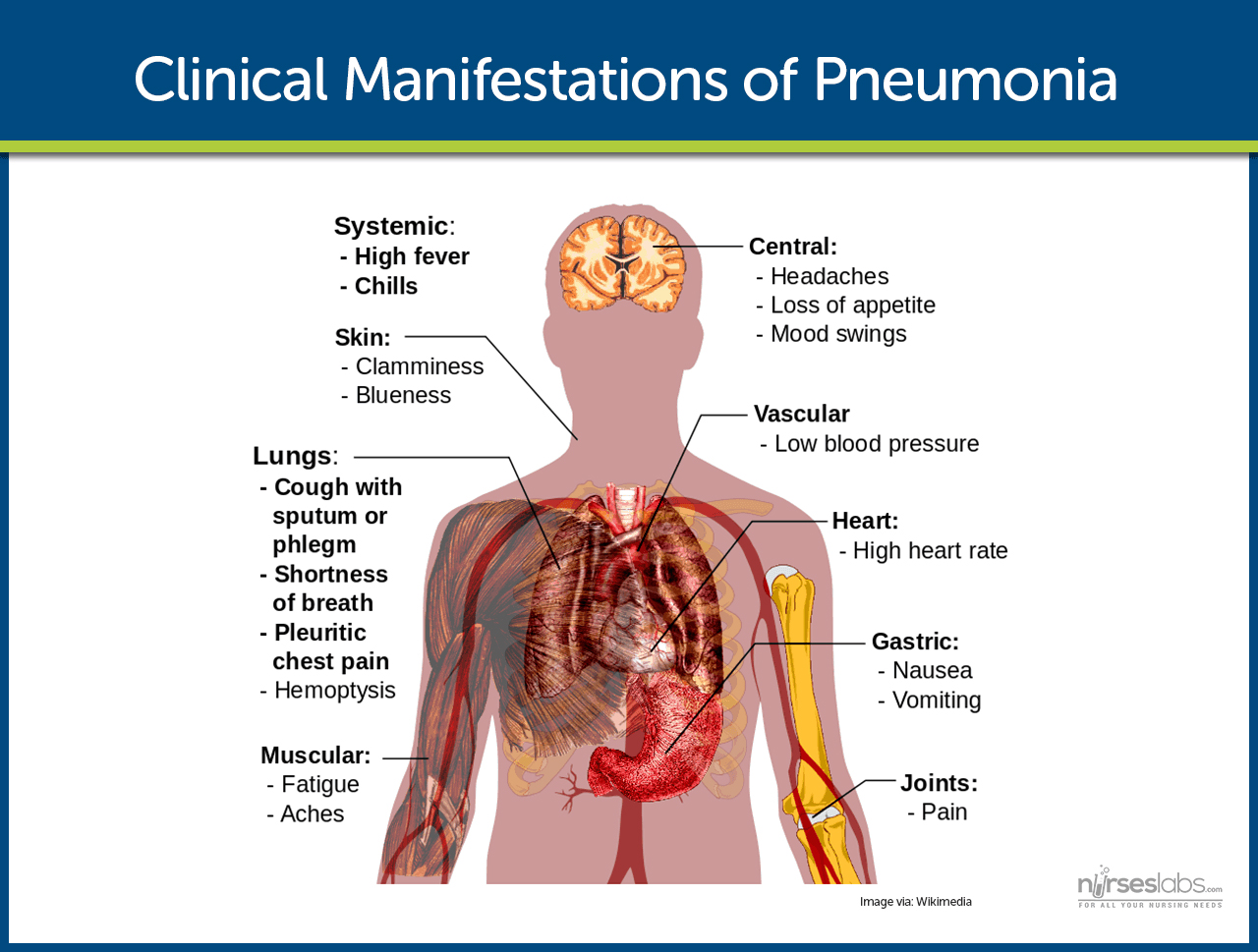
What are the symptoms of pneumonia?
The symptoms of pneumonia depend on:
- your age
- the cause and severity of your infection
- any existing immune system problems you may have
The most common symptoms of pneumonia are:
- fever — a temperature of 38℃ or higher
- cough — which can be dry or may produce thick mucus
- difficulty breathing or shortness of breath
- rapid breathing
- feeling generally tired and unwell
- loss of appetite
Your cough can last for several weeks after pneumonia has been treated successfully.
People with pneumonia may also:
- have a headache
- have pleurisy (chest pain that is worse with breathing)
- be confused or disorientated (especially older people) — due to lack of oxygen
- turn blue around the mouth (cyanosis) — due to lack of oxygen
If you have a bluish tinge to your lips or are confused call 000 for an ambulance right away.
Quite often, people with pneumonia have had cold or flu symptoms that have got worse, not better.
What causes pneumonia?
Pneumonia is caused by an infection of the lungs. Most infections are caused by bacteria or viruses.
Pneumonia can be triggered by a cold or the flu, which allows the germs to access to your lungs.
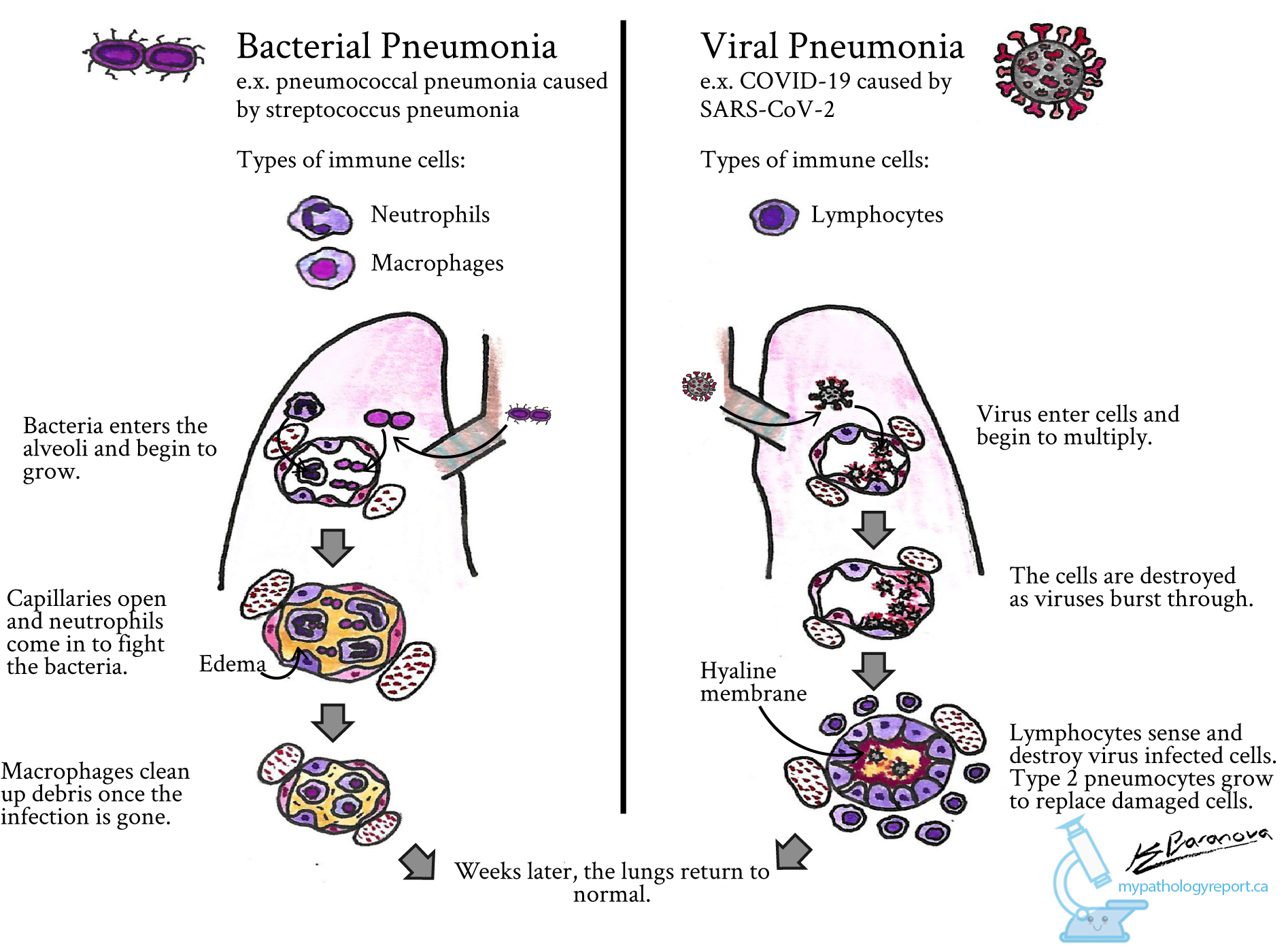
Bacterial pneumonia
Bacterial pneumonia may be caused by the pneumococcal bacteria, called streptococcus pneumoniae. This is one of the worst types of pneumonia.
Other types of bacteria that can cause pneumonia are haemophilus influenzae and moraxella catarrhalis.
Viral pneumonia
Viral pneumonia is caused by different viruses. The most common are:
- influenza (flu) virus
- respiratory syncytial virus
- SARS-CoV-2 — the virus that causes COVID-19
In severe cases of COVID-19, breathing difficulties can develop into pneumonia. This is a serious illness that can be life-threatening.
It’s thought that about half of pneumonia cases are caused by a virus.
Pneumonia from other infections
Another cause of pneumonia is mycoplasma pneumoniae. Pneumonia caused by mycoplasma organisms is usually milder, but the recovery can be longer.
Other organisms, such as fungi, can also cause pneumonia. This is more common in people whose immune systems are not working properly. This includes people with HIV infection or people being treated for cancer.
How is pneumonia diagnosed?
Doctors diagnose pneumonia mainly by talking with you and examining you.
Tests for pneumonia include:
- blood tests
- a chest x-ray
How is pneumonia treated?
Treatment will depend on your age and the type of pneumonia you have.
If bacteria have caused your infection, the main treatment is antibiotics. Antibiotics are medicines that kill bacteria. In milder cases, antibiotics can be taken as tablets, by mouth. In more severe cases, they’ll be given to you via a drip, at least at first.
Antibiotics are usually given at the first sign of pneumonia.
If your symptoms don’t improve after 5 days of taking antibiotics, contact your doctor. Sometimes you may need to change the dose or type of antibiotic, or you may need more than one medicine.
Viral pneumonia treatment
Viral pneumonia cannot be treated with antibiotics. In most cases, viral pneumonia will clear up by itself.
Will I need to go to hospital?
Most people who have pneumonia will be able to recover at home.
Some people will need to be treated in hospital. This is more common for people who are:
- babies
- young children
- people over 70 years
In hospital you may get fluids through a drip in your arm, as well as antibiotics. The doctors will also monitor you to see if there is enough oxygen in your blood.
Taking care of myself
There are some things you can do to help your recovery:
- get plenty of rest
- drink plenty of fluids — to avoid dehydration
- take paracetamol— to relieve pain and reduce fever
If you’re a smoker you should try to quit smoking.
Keep well away from things that will irritate your lungs, such as wood fires and cigarette smoke.
Some people may also need physiotherapy to help clear their lungs.
Can pneumonia be prevented?
Prevention is the best protection from pneumonia. Vaccinations can help prevent some types of pneumonia.
One vaccination that reduces your risk of pneumonia is the pneumococcal vaccine. The pneumococcal vaccine is free in Australia for some people through the National Immunisation Program (see below).
It’s a good idea to speak to your doctor about whether vaccination is recommended for you or for your children.
Pneumococcal vaccine
Vaccination is your best protection against pneumonia. This table explains more about the pneumococcal vaccine.
| What age is it recommended? | It is recommended:
|
| How many doses are required? | The recommended number of doses depends on:
|
| How is it administered? | Injection |
| Is it free? | The vaccine is free for:
Ask your doctor if you are eligible for additional free vaccines based on your situation. You can find out more about vaccination on the Department of Health website and the National Immunisation Program Schedule. |
| Common side effects | The vaccine is very safe. Side effects depend on your age and the type of vaccine that you are given. In children, side effects may include pain, redness and swelling where the needle went in. Other reported side effects are: feeling irritable, feeling drowsy, fever, and a reduced appetite. |
Other vaccinations
You can also consider getting vaccinated against influenza. Pneumonia is one of the possible complications of influenza.
A new influenza vaccine is available every year. It is free to people who are at increased risk, including:
- children between the ages of 6 months and 5 years
- Aboriginal and/or Torres Strait Islander people of all ages
- people with certain medical conditions
- pregnant women
- people aged 65 and over
For more information about the influenza vaccine, visit the Department of Health website.
Vaccination can also prevent other illnesses that can lead to pneumonia. These are available for all children in Australia as part of their routine childhood vaccinations. The National Immunisation Program Schedule includes:
- haemophilus influenzae type b (Hib)
- measles
- pertussis (whooping cough)
- varicella (chickenpox)
Other ways to prevent pneumonia
Not smoking will help protect you against pneumonia.
If you or someone near you has an infection, you can reduce the risk of passing that infection on by:
- limiting your exposure to others while you are unwell
- washing your hands frequently with soap and water
- keeping your hands away from your eyes, nose and mouth
- avoiding sharing food, drink and utensils
Cough etiquette
When coughing and sneezing use a tissue to cover your nose and mouth. Then throw the tissue away.
If you don’t have a tissue, cough or sneeze into your inner elbow.
