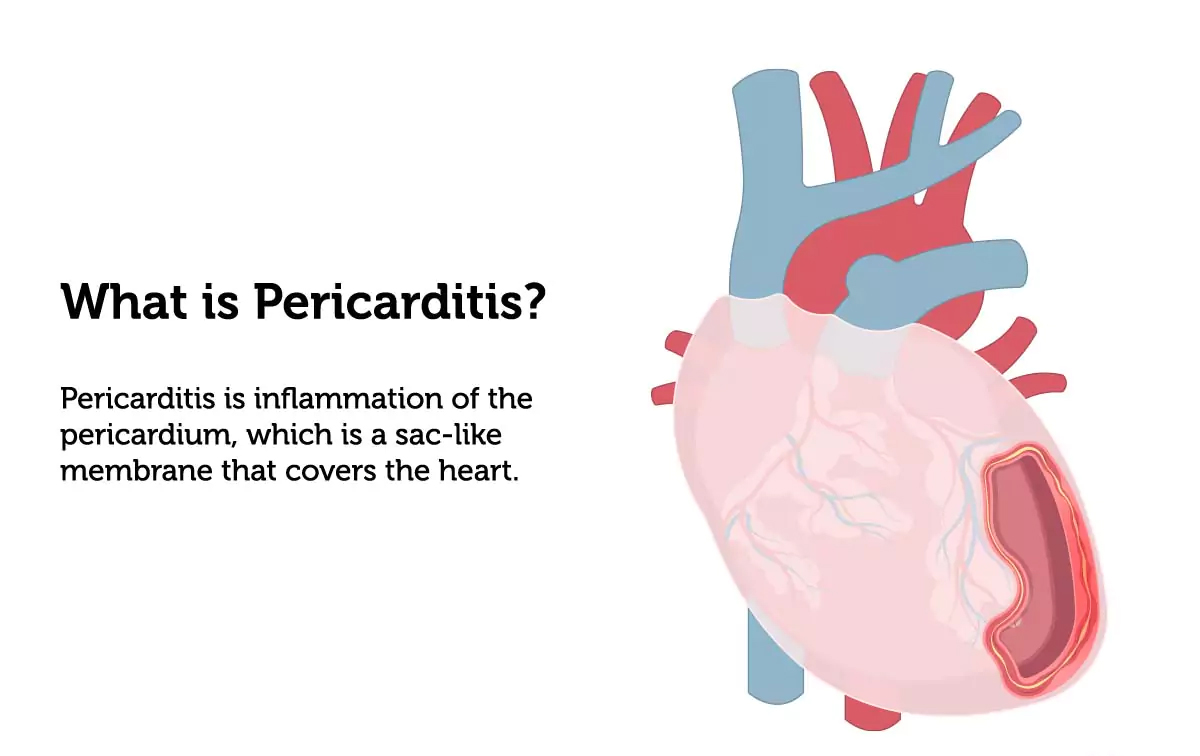
What is pericarditis?
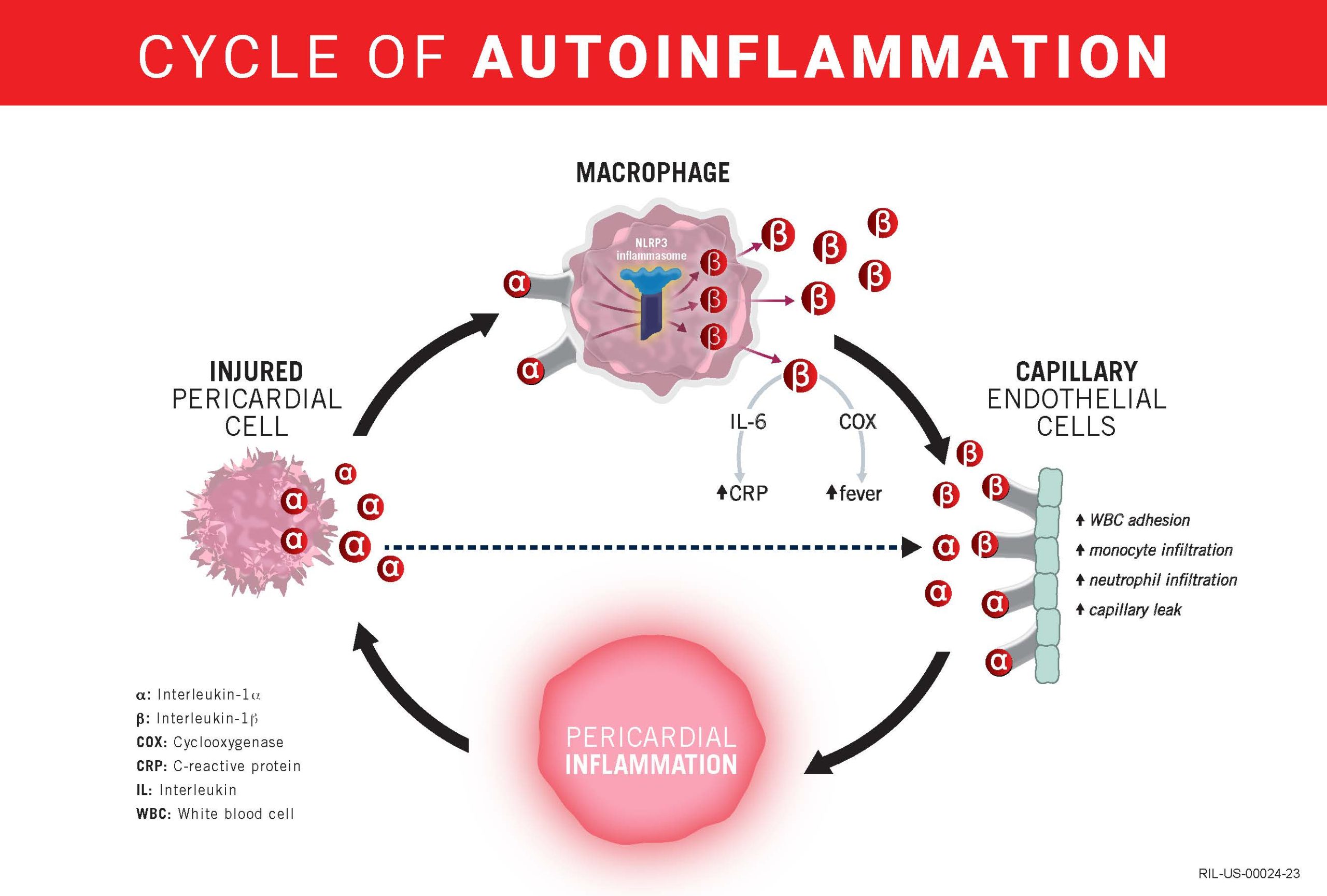
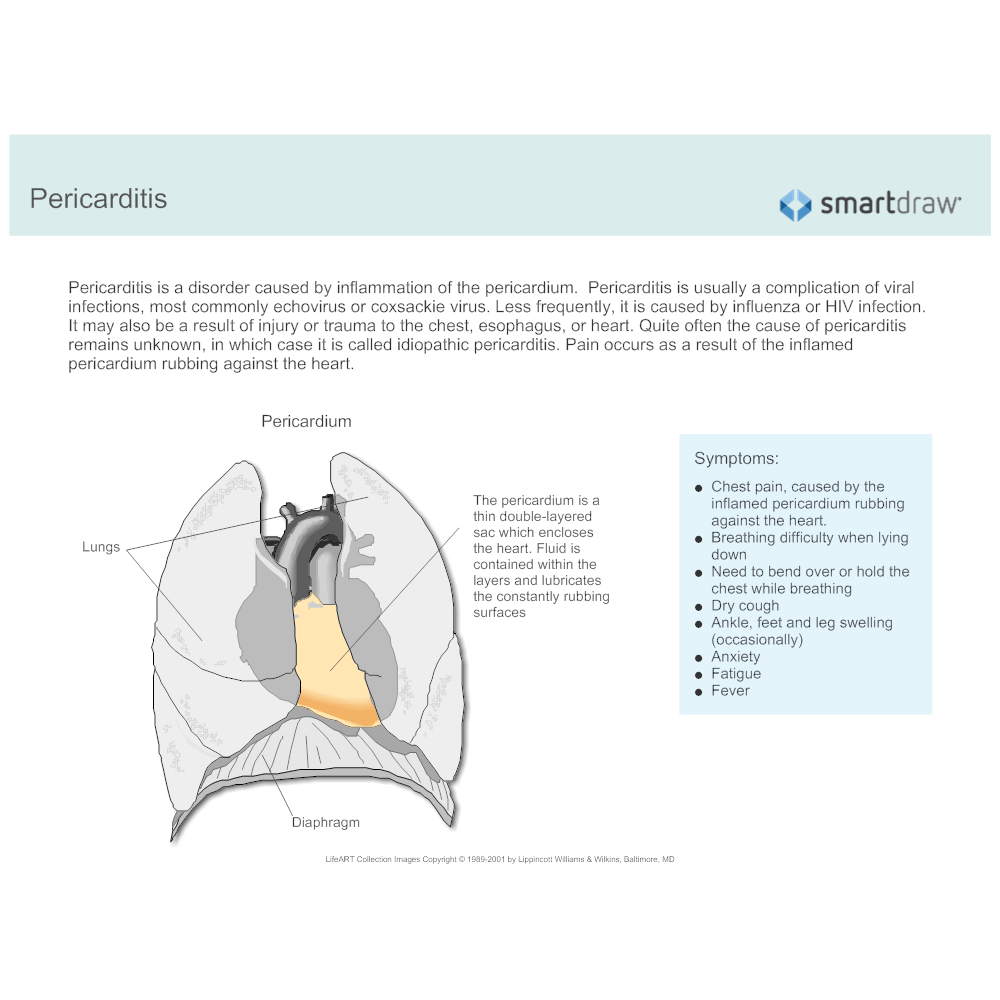
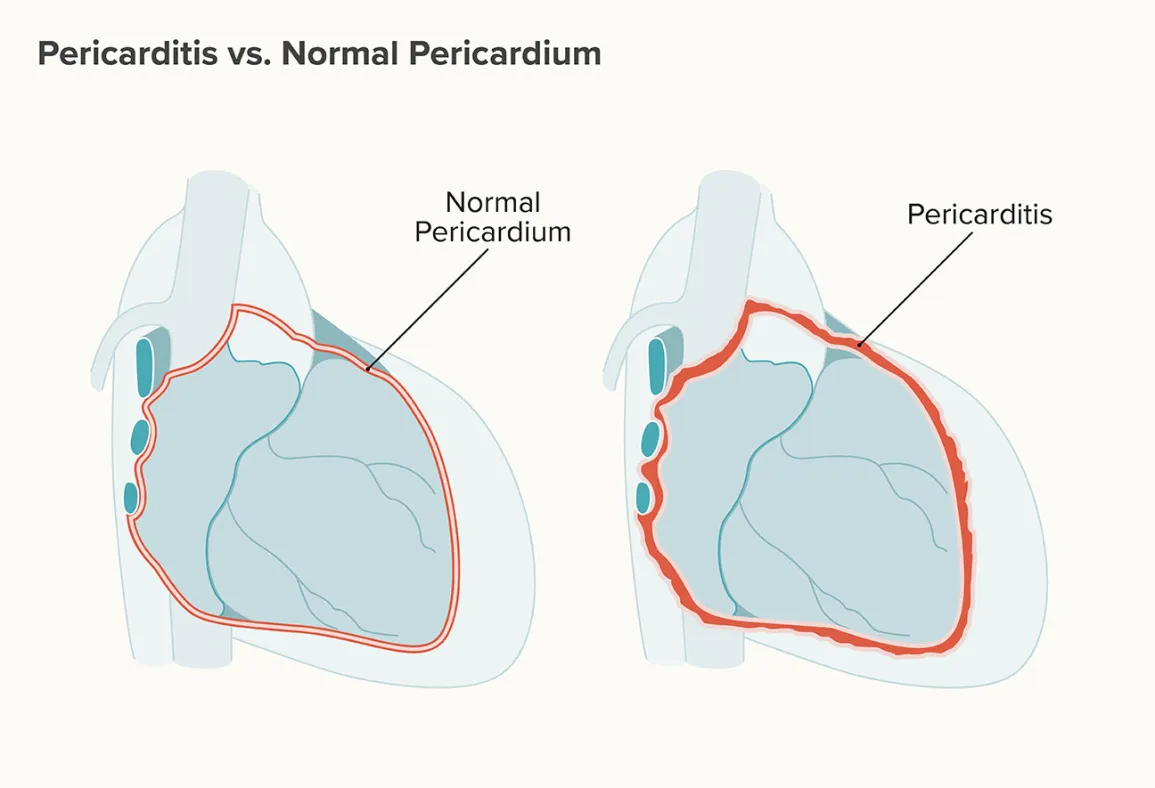
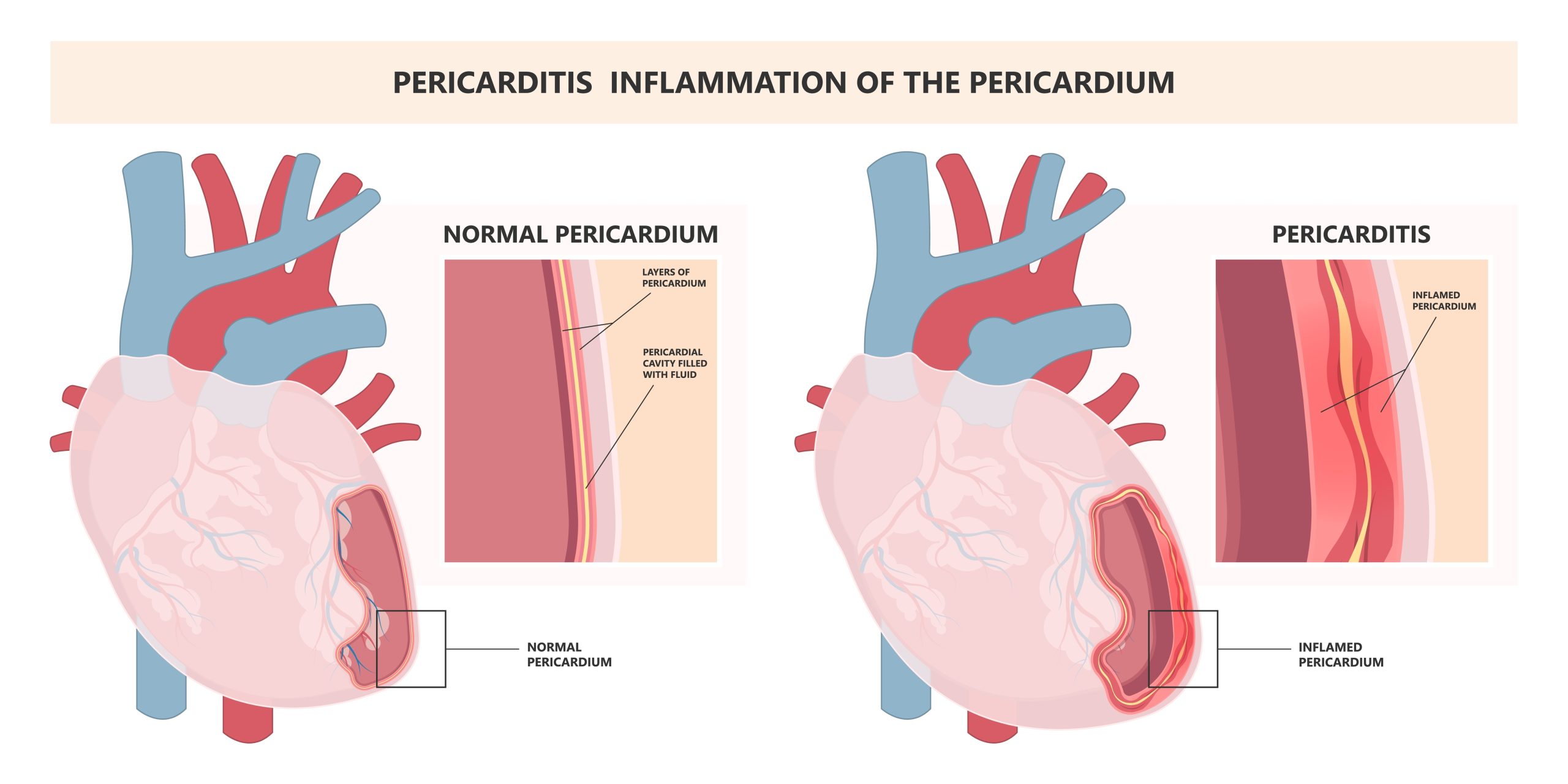
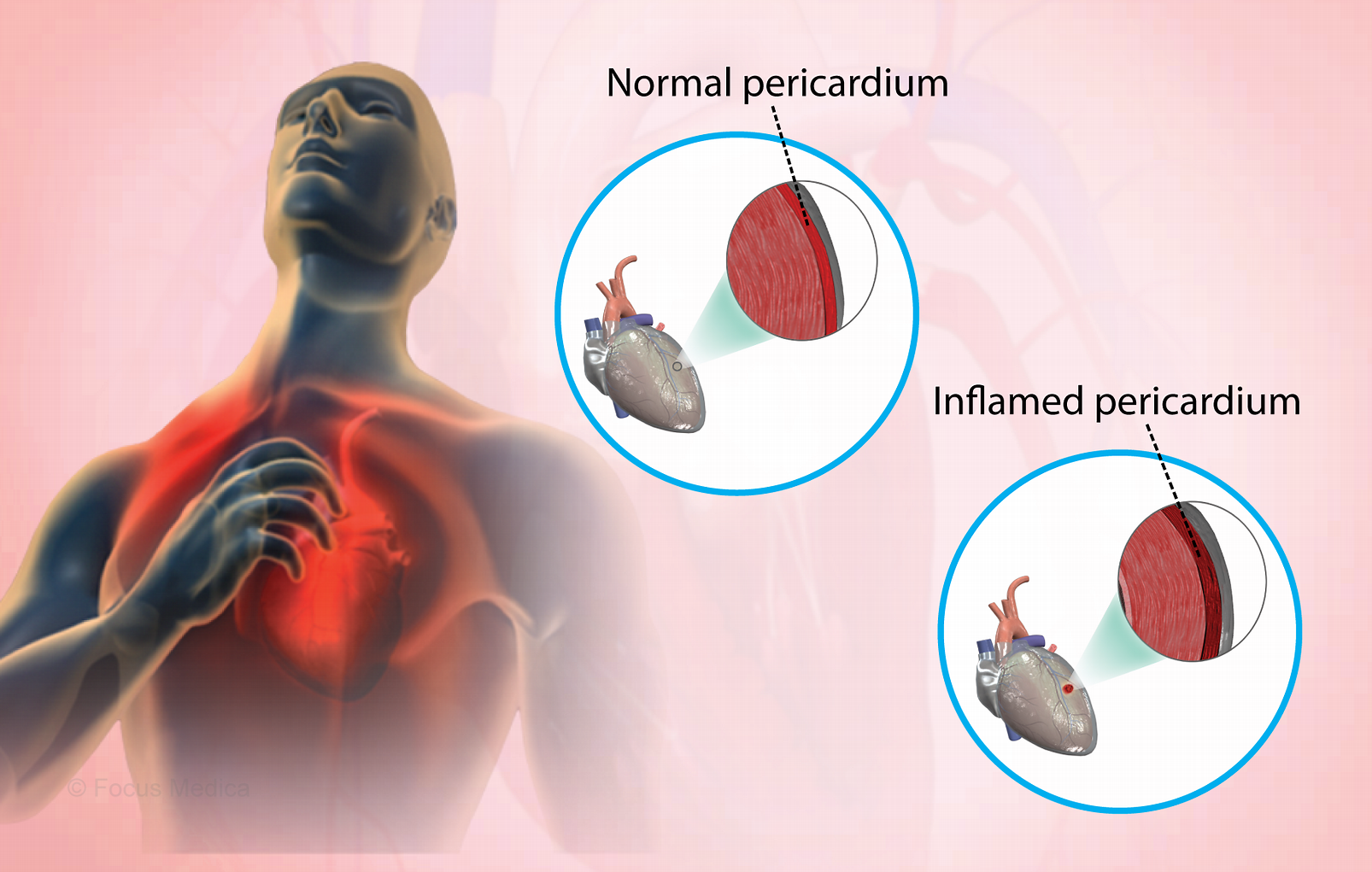
Pericarditis is inflammation of the pericardium, the thin sac-like membrane around the heart. It becomes swollen and irritated. Pericarditis often causes chest pain and sometimes other symptoms.
It is a serious condition; you should always seek medical attention if you have any type of chest pain.
The main types of pericarditis are:
- acute pericarditis — symptoms begin suddenly, but don’t last long
- chronic pericarditis — symptoms develop gradually and persist, or may persist after an acute attack
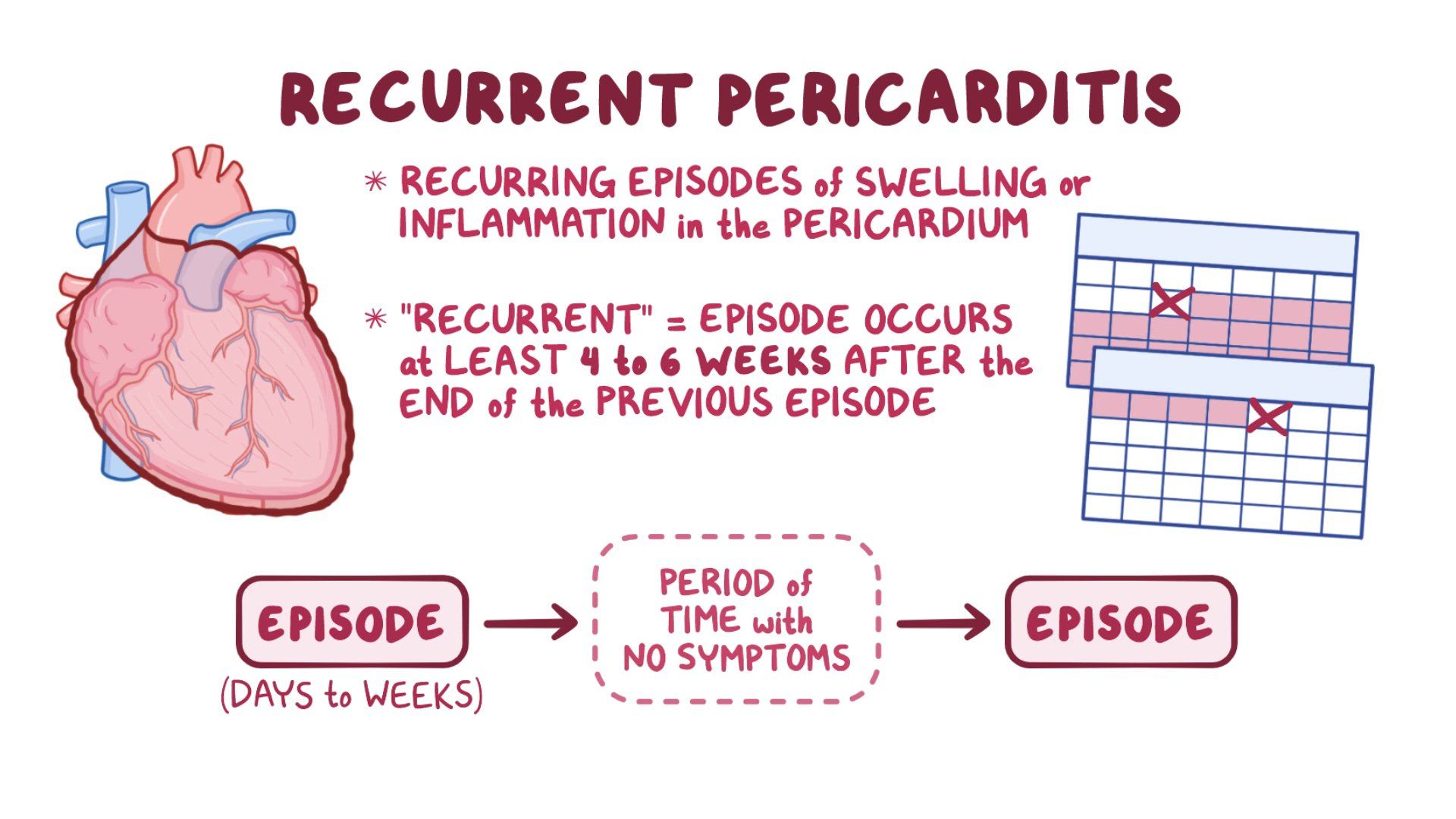
- recurring pericarditis — repeated attacks of acute pericarditis
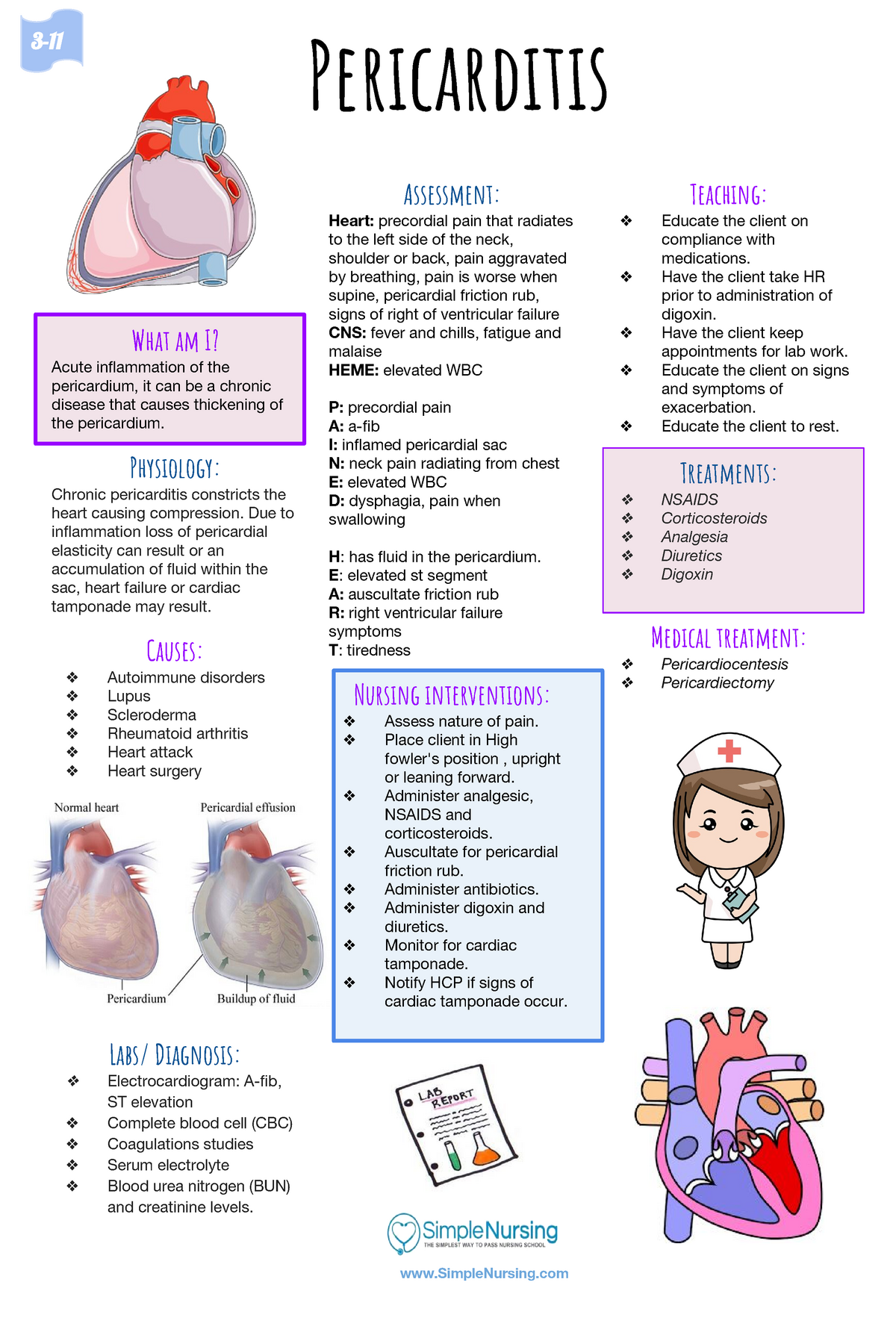
What are the symptoms of pericarditis?
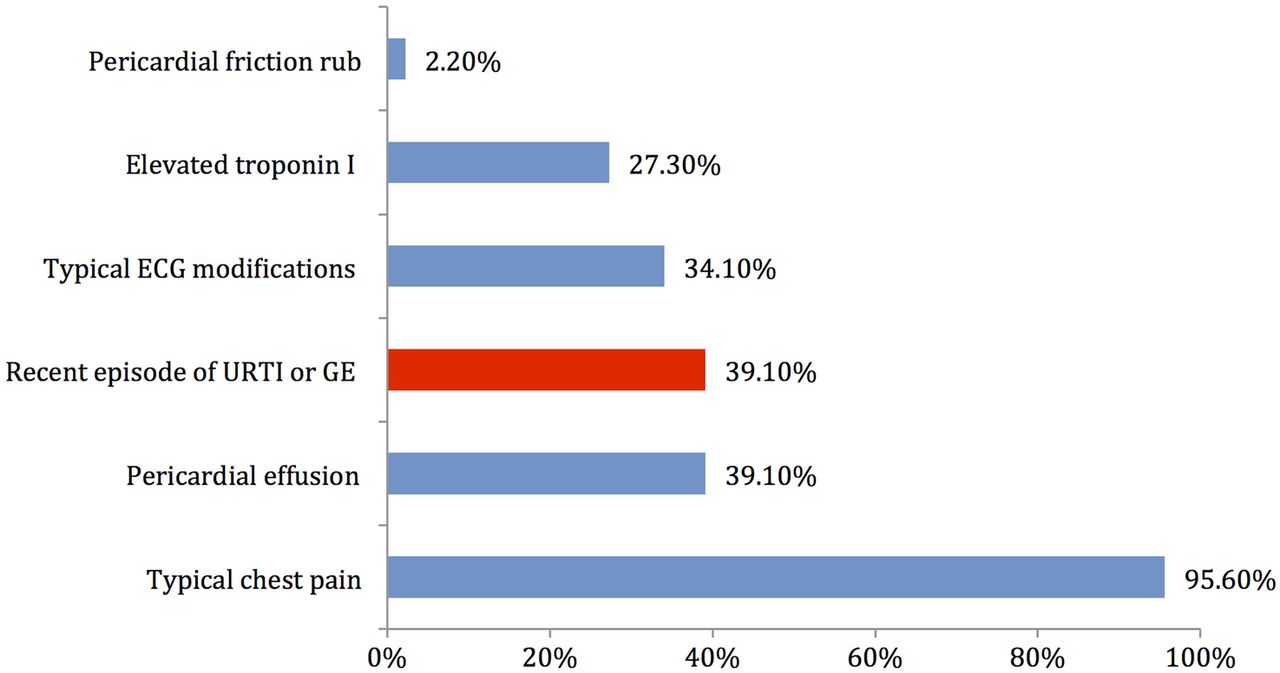
The most common symptom of pericarditis is sharp, piercing chest pain in the centre or left side of the chest.
Depending on the cause of pericarditis, symptoms may also include:
- low fever
- heart palpitations
- shortness of breath
- weakness or fatigue
- nausea
- dry cough
- swelling of the legs or abdomen
The symptoms of pericarditis can be similar to those of a heart attack, pneumonia, pulmonary embolism, pneumothorax, pleurisy or costochondritis. So it is always important to seek medical attention if you have any of the symptoms listed above.
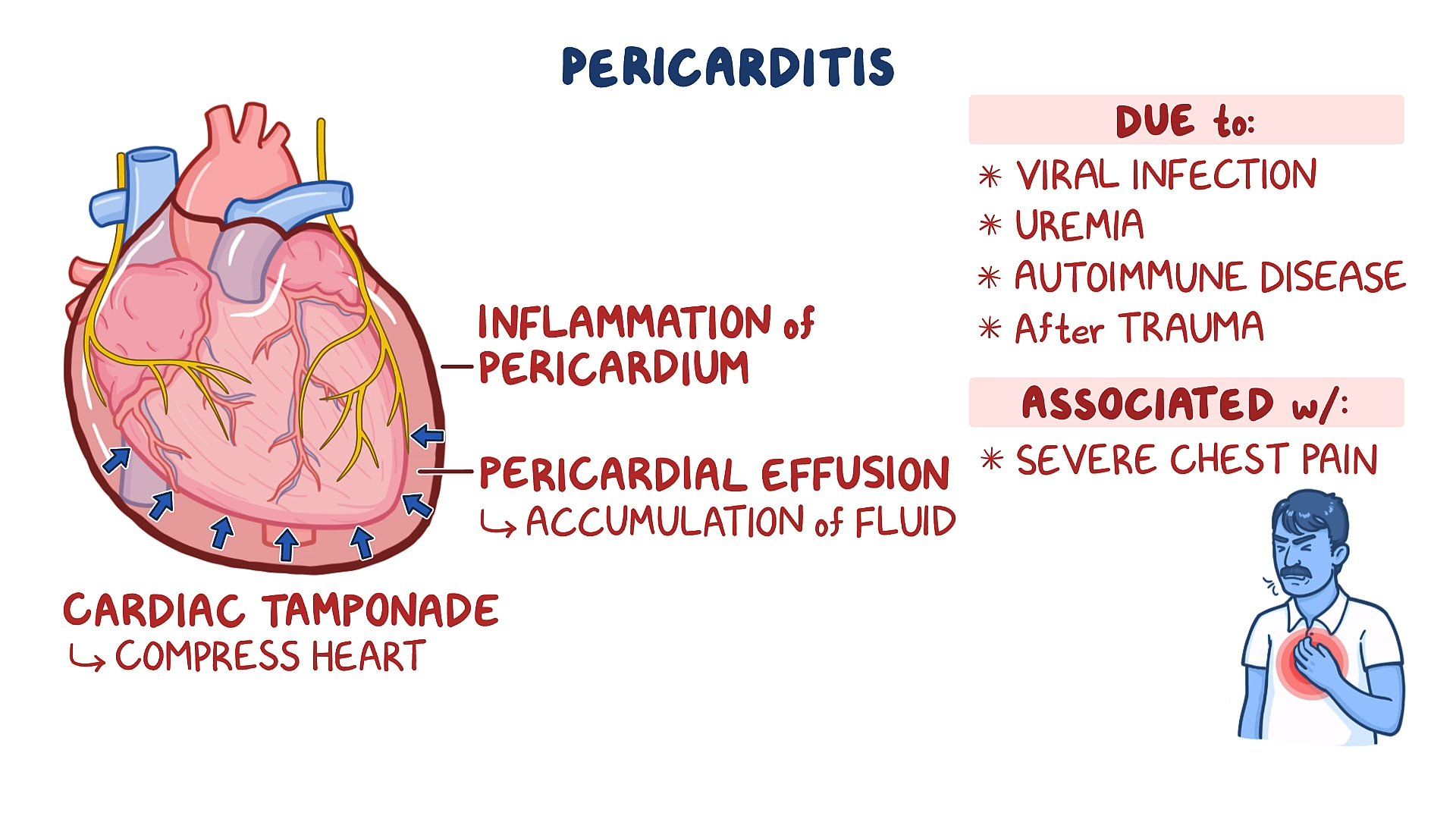
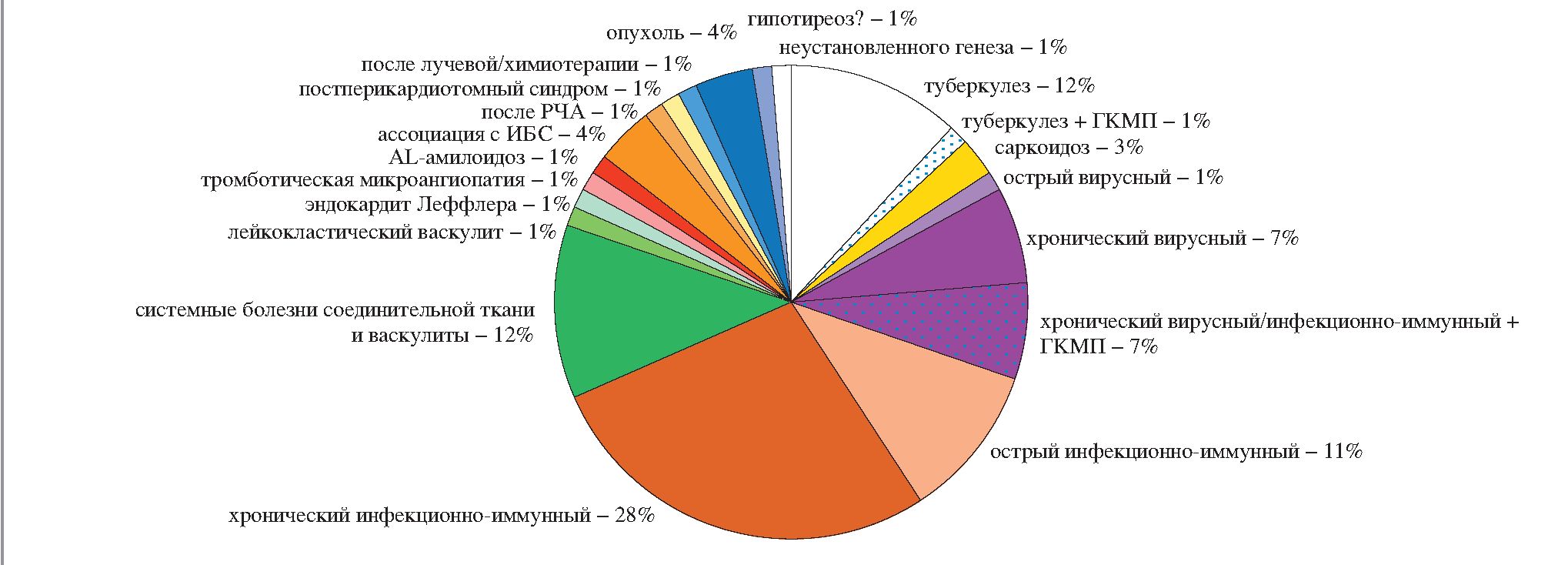
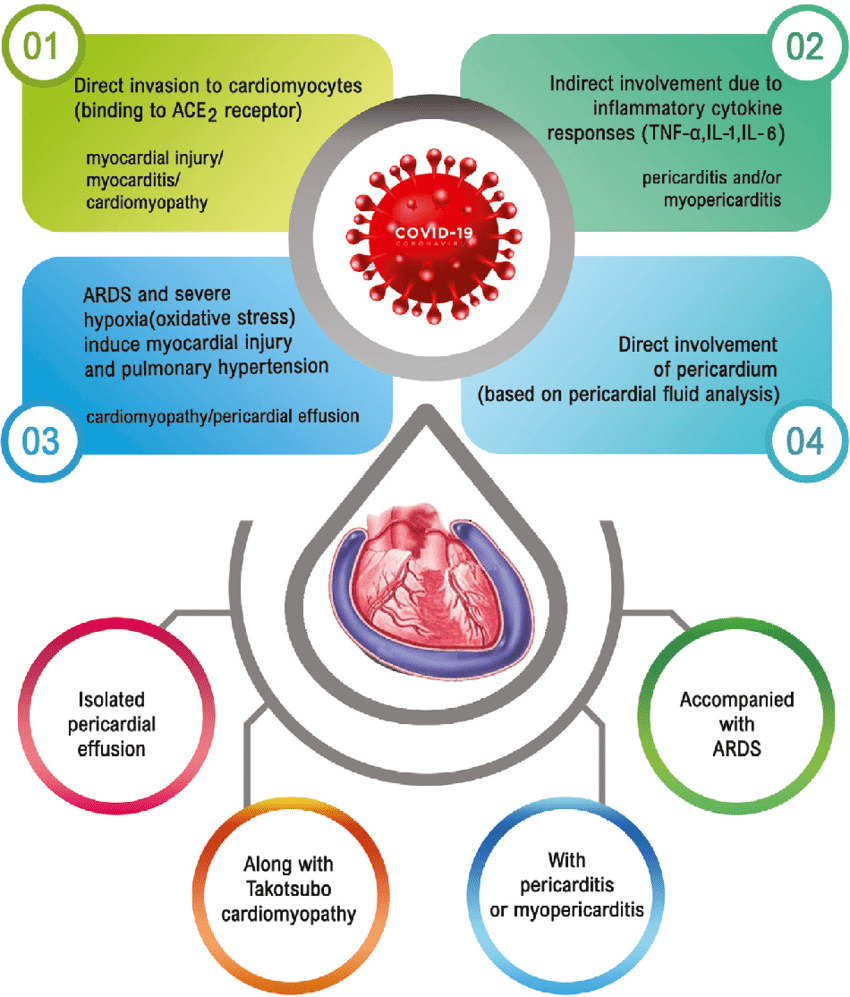
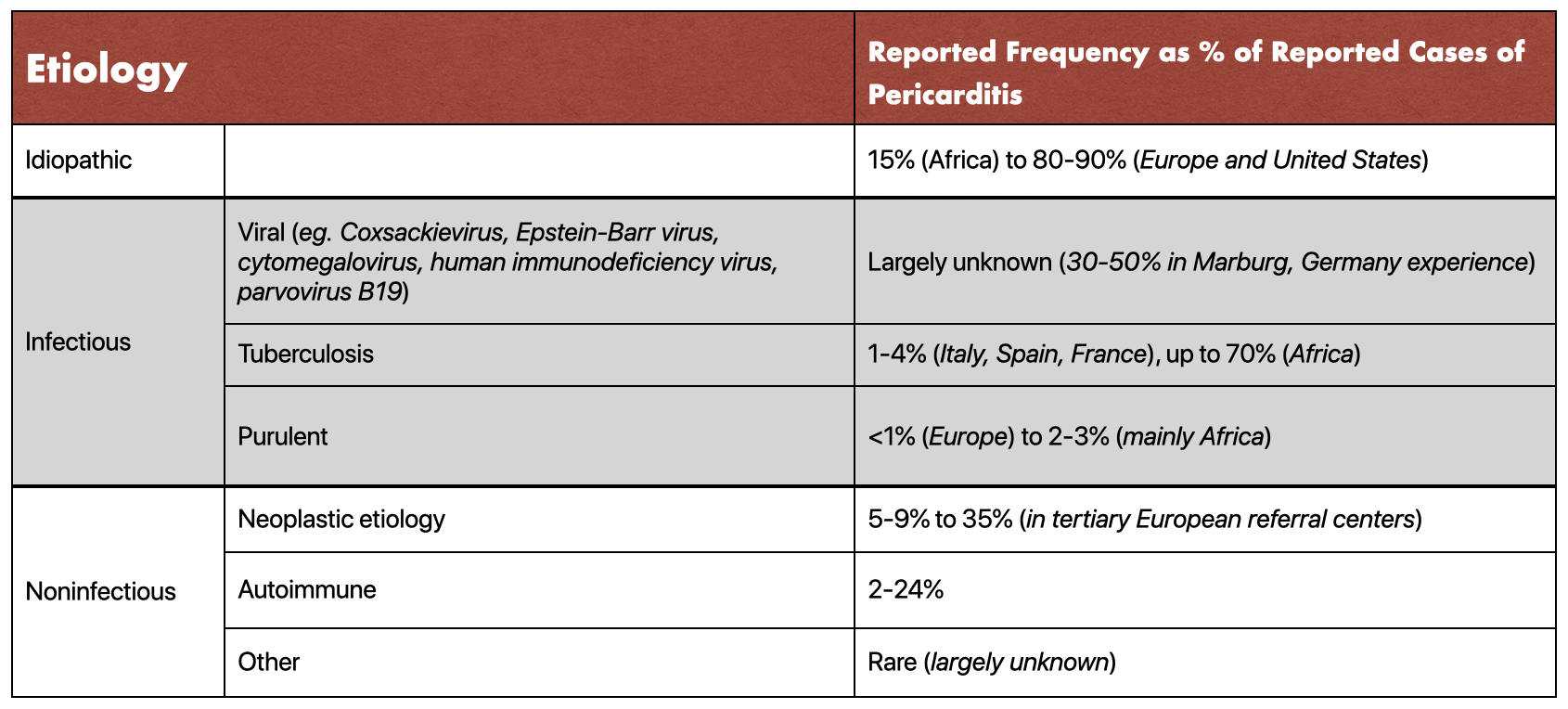
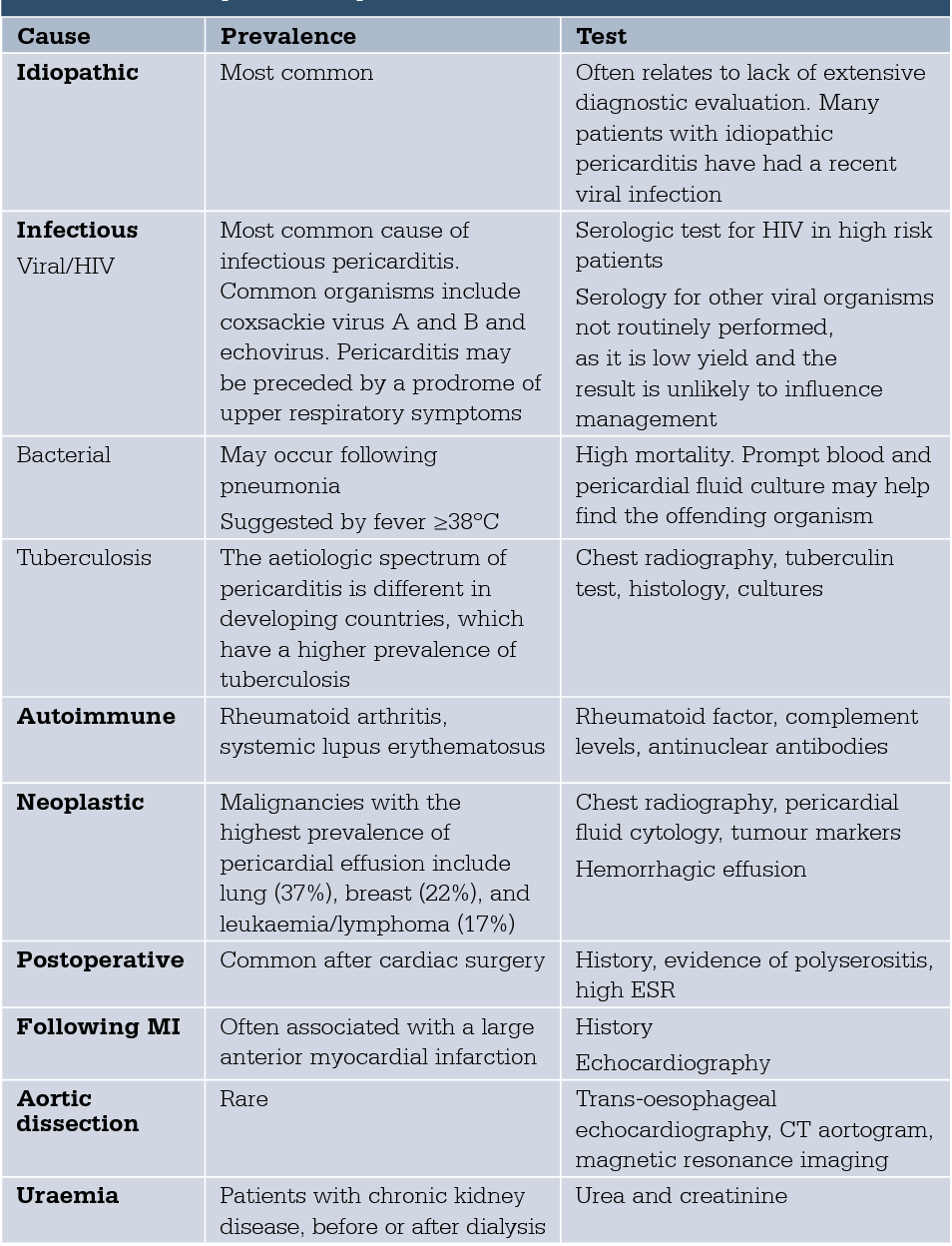
What causes pericarditis?
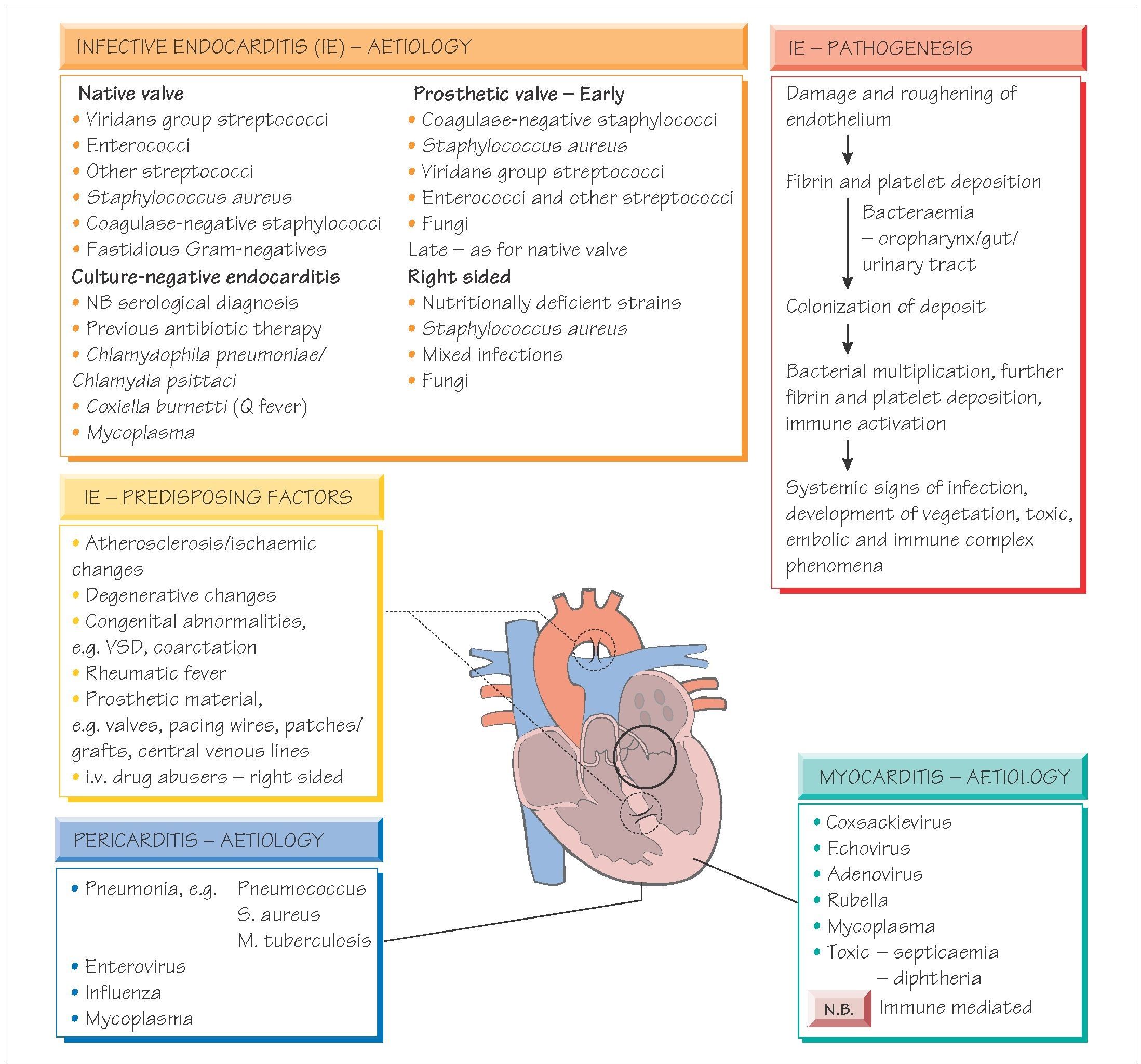
Pericarditis can be caused by a viral, bacterial or fungal infection.
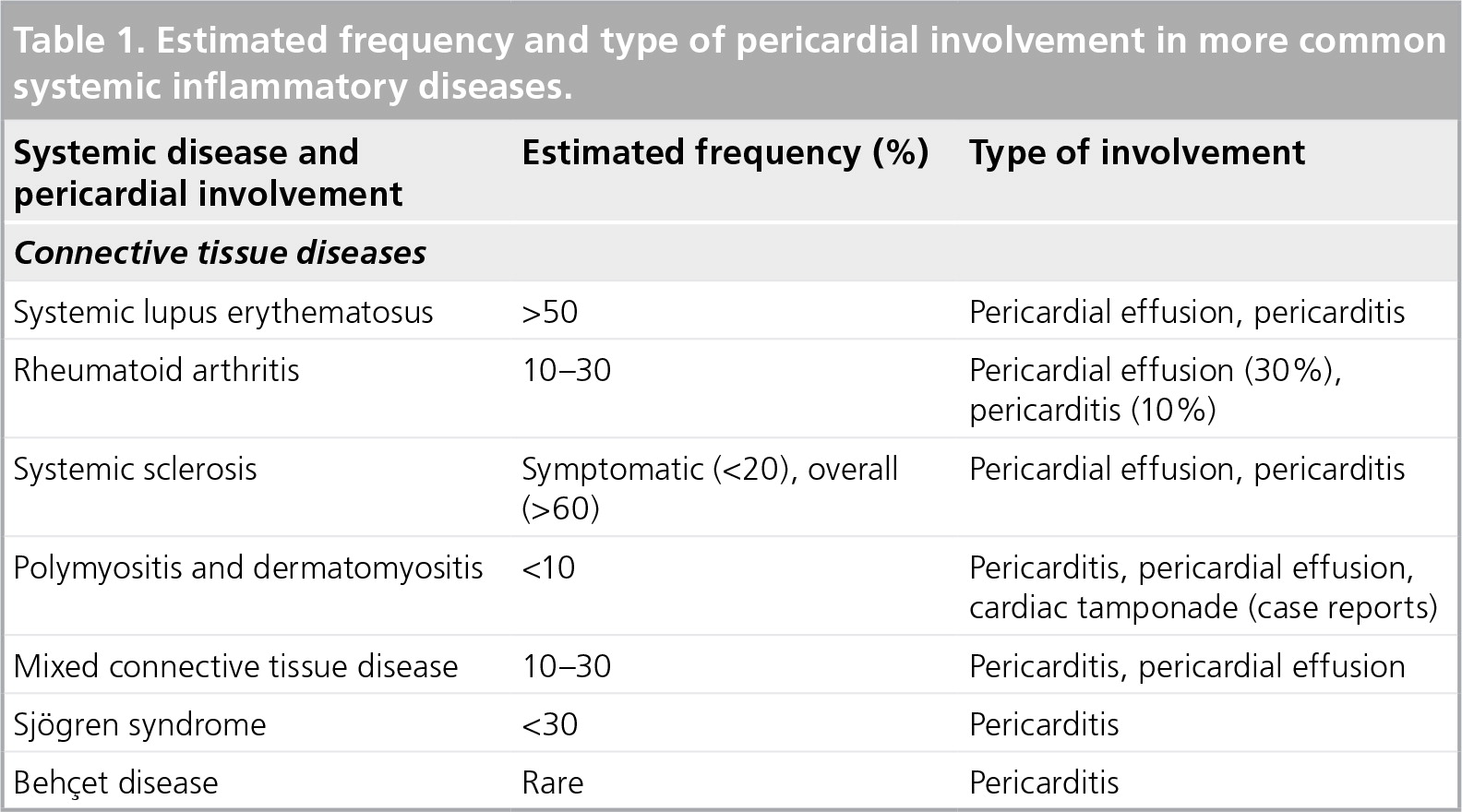
Pericarditis can also develop after a heart attack. Other less common causes include autoimmune disorders, such as lupus or rheumatoid arthritis, or a heart or chest injury.
Often, the cause of pericarditis cannot be found.
Pericarditis has been reported as a rare side effect of the mRNA COVID-19 vaccines Comirnaty (Pfizer) and Spikevax (Moderna). Symptoms typically appear within 1 to 5 days of vaccination. People who experience any of the following symptoms after having an mRNA COVID-19 vaccine should seek prompt medical attention:
- chest pain
- pressure or discomfort in the chest
- irregular, skipped heartbeats or ‘fluttering’
- fainting
- shortness of breath
- pain when breathing
How is pericarditis diagnosed?
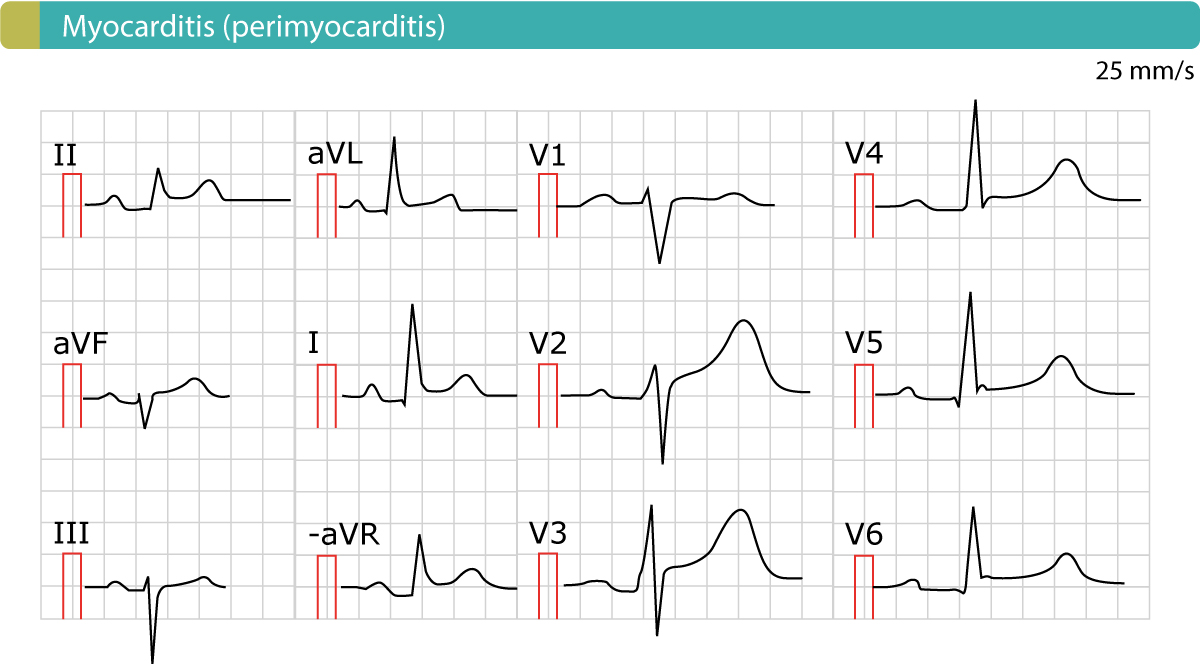
Your doctor may perform a physical examination and listen to your heart using a stethoscope. They may also run blood and other tests such as an electrocardiogram (ECG), and suggest that you have a chest x-ray to check the size and shape of your heart, or other imaging such as an echocardiogram (ultrasound), CT scan or MRI scan.
Pericarditis is usually able to be confirmed with a physical examination and electrocardiogram (ECG).
How is pericarditis treated?
Most people with pericarditis need monitoring and treatment to reduce the pain and swelling. If complications develop, surgery may be needed.
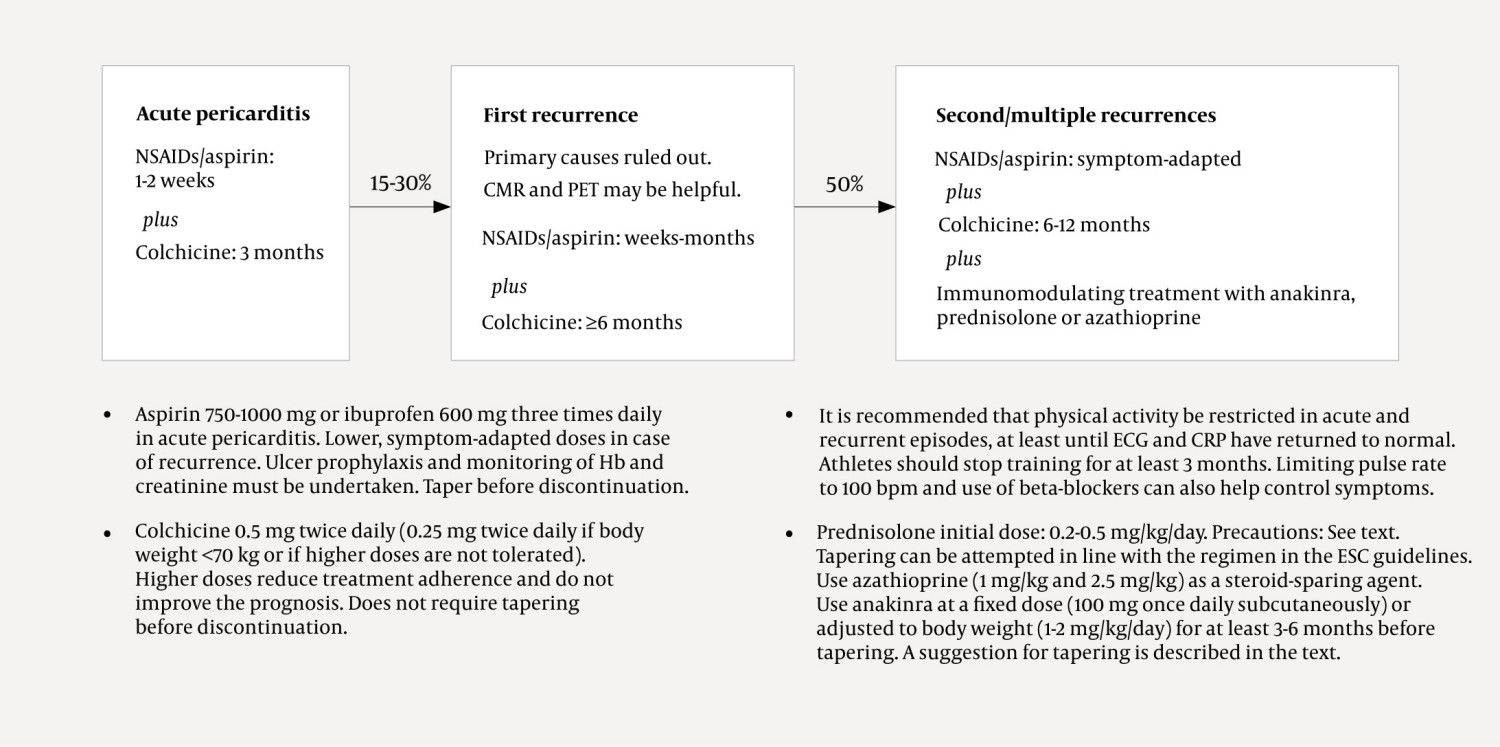
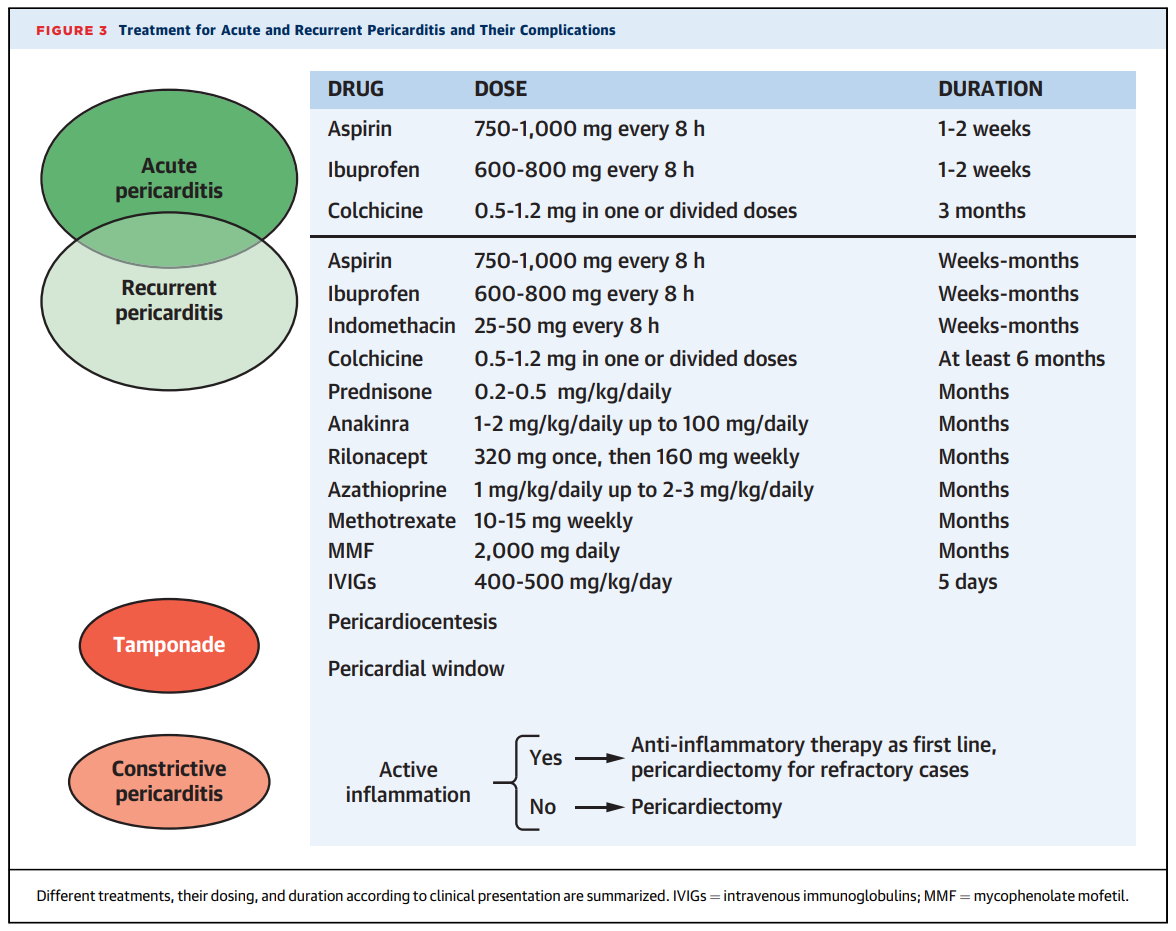
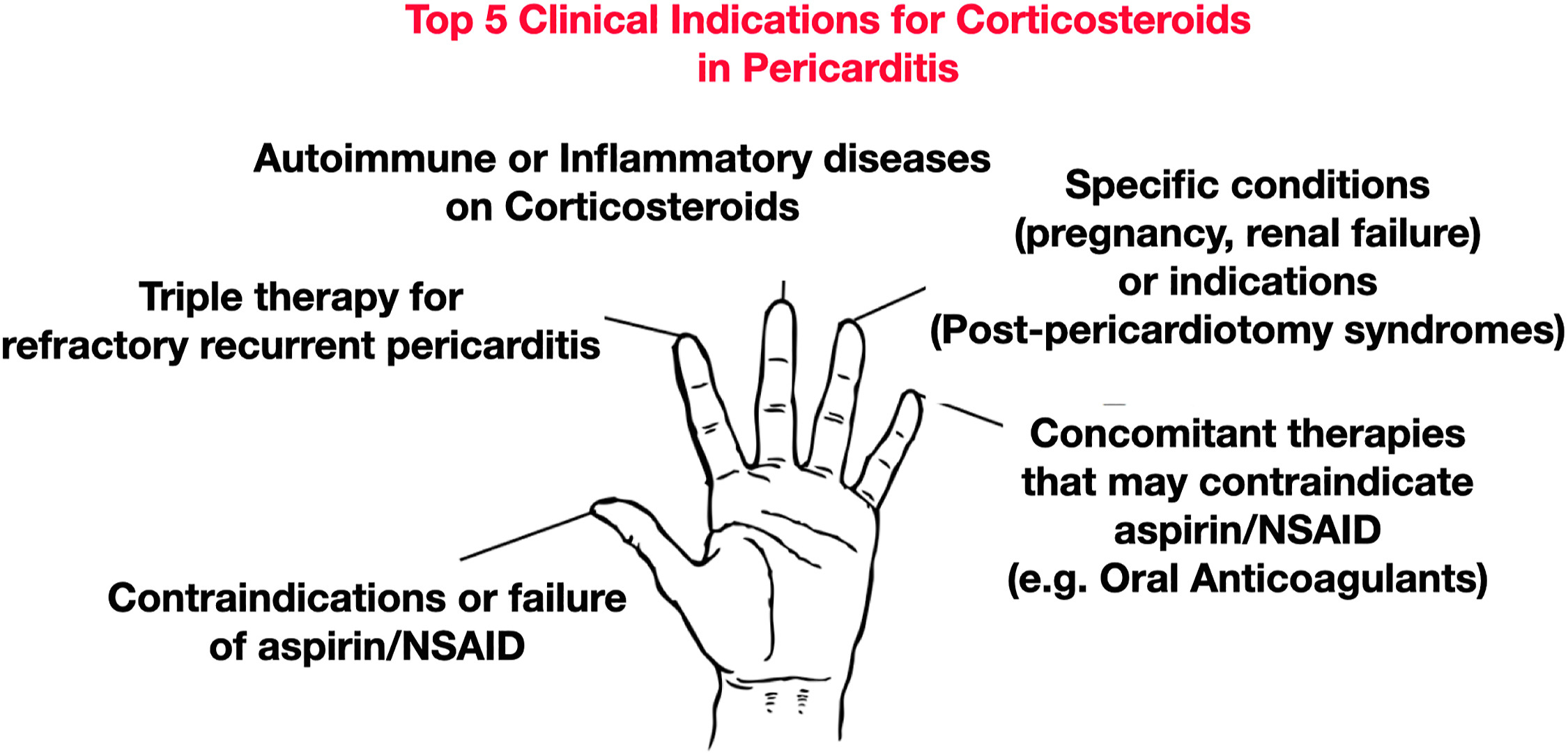
Treatment will depend on type of pericarditis you have, and may include:
- non-steroidal anti-inflammatory drugs (NSAIDs) to reduce swelling
- antibiotics, if there is a bacterial infection
- colchicine, a prescription-only medicine often used for recurring pericarditis
- pain relief medication
If an underlying cause is found, it will be treated where possible. You may also be monitored for potential complications. You will also be advised to avoid strenuous activity until your symptoms get better.
What are the complications of pericarditis?
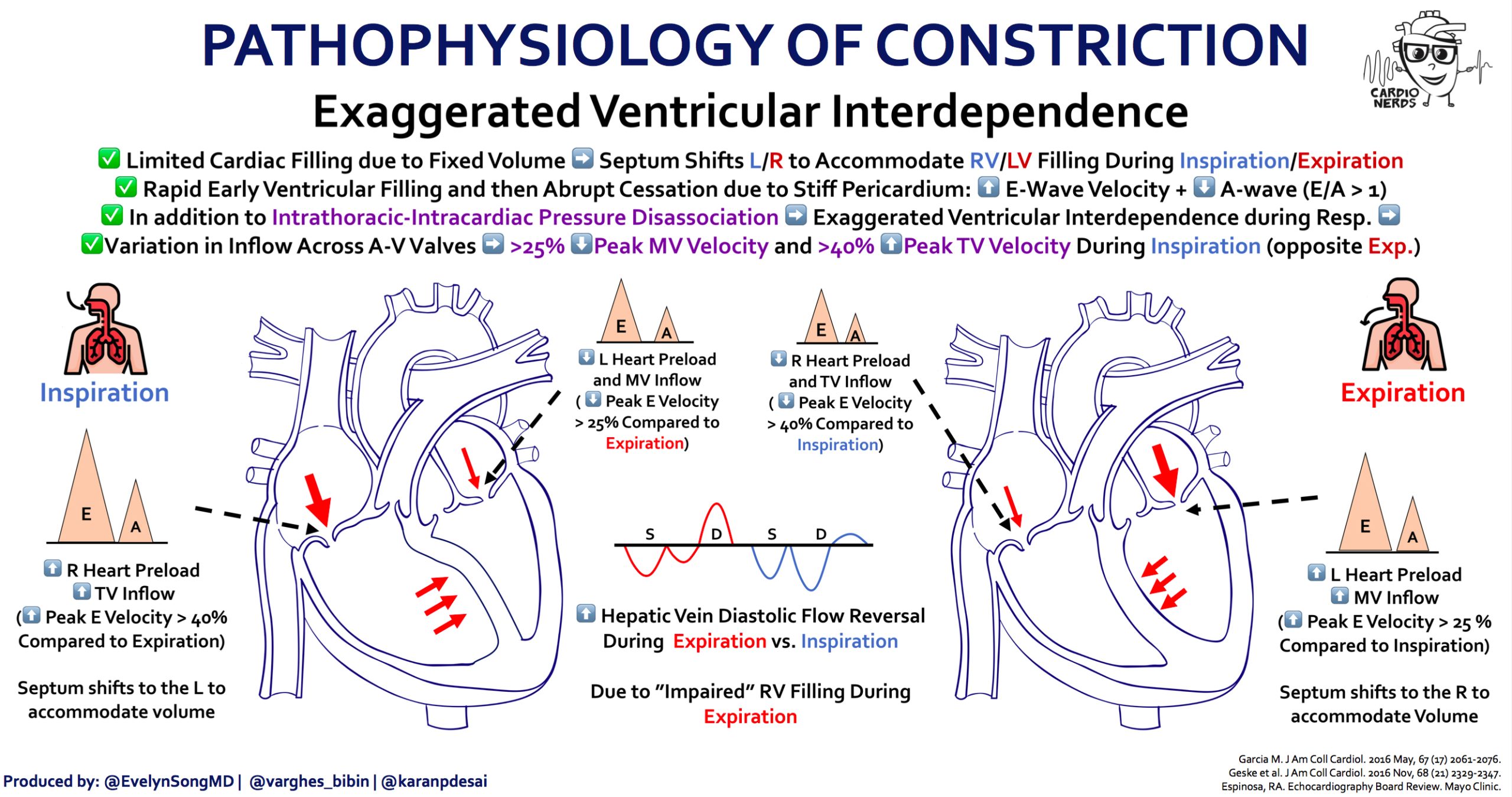
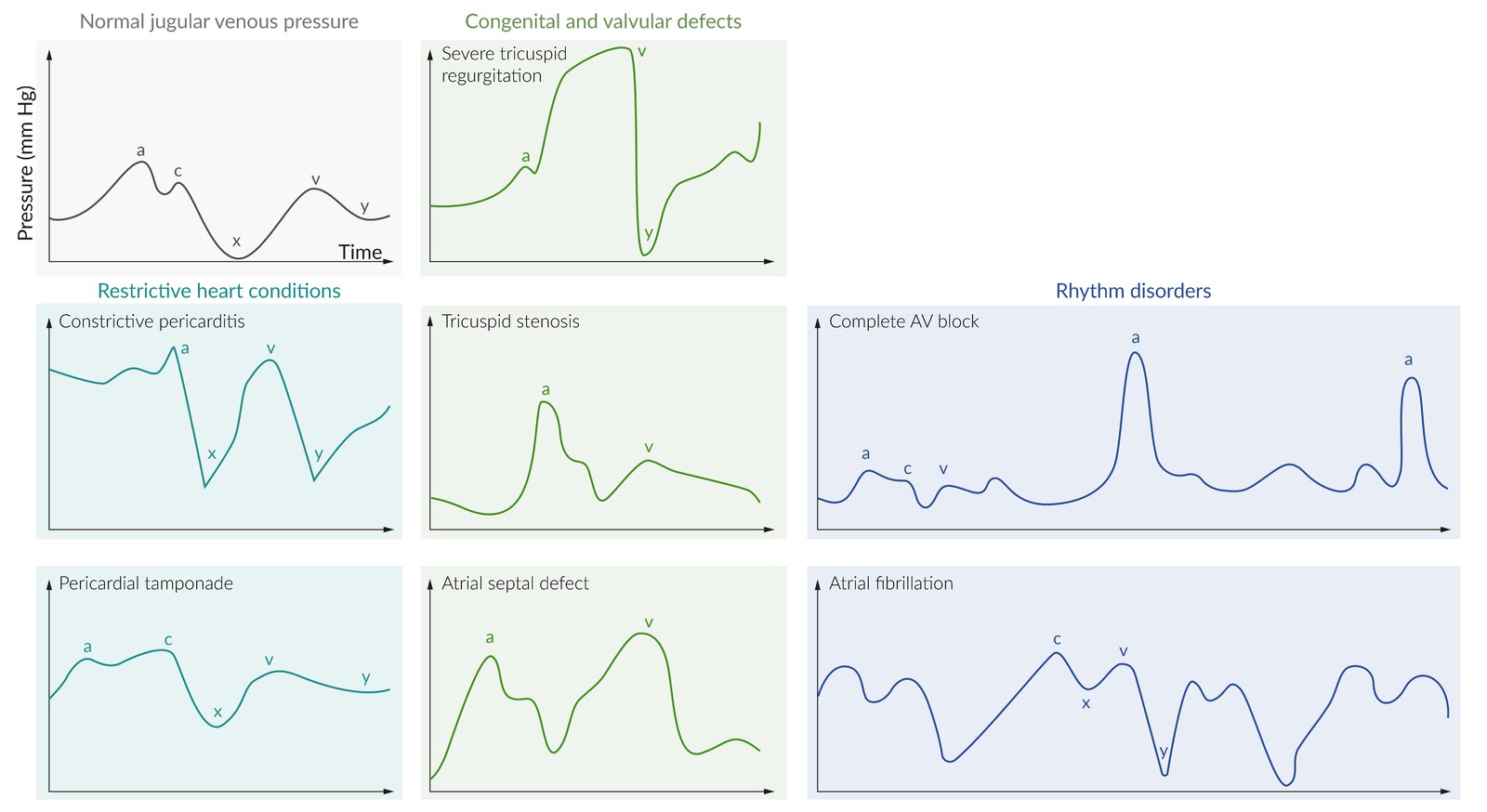
It is possible to develop constrictive pericarditis — permanent thickening and scarring of the pericardium, which stops the heart beating properly, often leading to severe swelling of the legs and abdomen.
Cardiac tamponade is a dangerous condition, where too much fluid collects in the pericardium, which puts pressure on the heart and causes blood pressure to drop dramatically. This is life-threatening and requires emergency treatment.