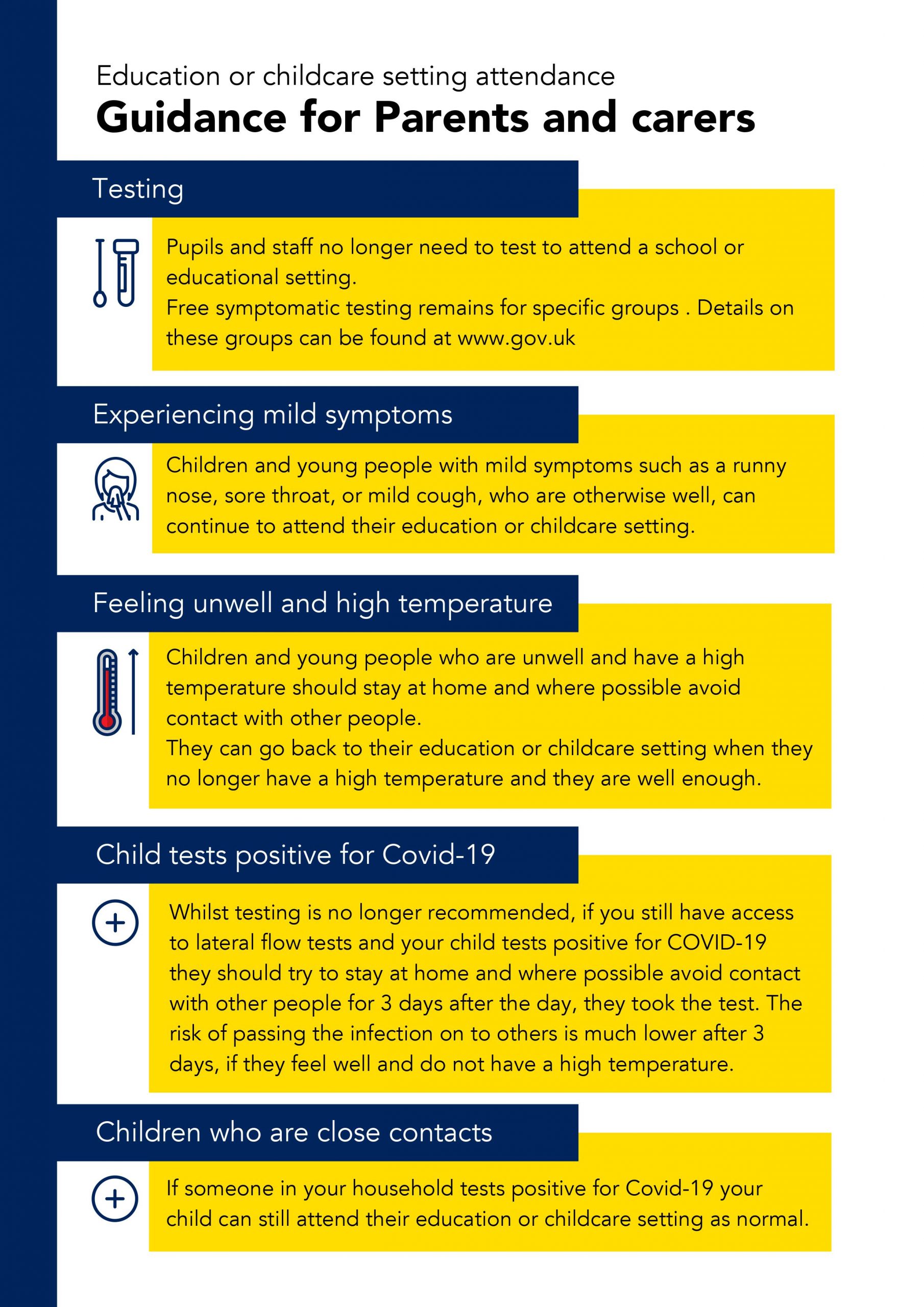
Who is a ‘close contact’?
State and territory governments decide on the definition of a close contact and there are differences between them. Please check the definition made by the government of the state or territory that you are in.
You are generally a close contact of someone who has COVID-19 if:
- you are living with someone who has COVID-19; or
- you have spent a lot of time indoors with someone who has COVID-19; or
- under exceptional circumstances determined by states or territories
What should a close contact do?
If you are a close contact of someone who has COVID-19, you should follow the close contact recommendations of the state or territory that you are in.
The recommendations may include wearing a mask, getting tested and working or studying from home. You may also be recommended to avoid high-risk places or having contact with people at risk of severe illness.
- ACT
- New South Wales
- Northern Territory
- Queensland
- South Australia
- Tasmania
- Victoria
- Western Australia
Do close contacts still need to isolate?
If you are a close contact of someone who is a confirmed case of COVID-19, you do not have to isolate. However, you should follow the recommendations of the state or territory you are in.
How should I care for a close contact, including myself?
Isolation is no longer mandatory in Australia, but you can follow these tips to help ease symptoms and stop the spread of COVID-19.
- The person with COVID-19 should isolate at home and not go out other than to get medical care. They shouldn’t go to work, school or public areas, or use public transport or taxis.
- Call ahead before visiting doctors or health clinics to tell them that the person has COVID-19.
- The person with COVID-19 should wear a face mask when in the same room as people who don’t have COVID-19. They should wear a face mask if they must go out in public, such as to seek healthcare.
- When you are in the person’s room, wear a single-use surgical mask and disposable gloves. This is especially important if you have contact with their body fluids or secretions, or blood. Throw out masks and gloves after use.
- Keep vulnerable people, such as older people and people with compromised immune systems or chronic health conditions, away from the person. This includes people with chronic heart, lung or kidney conditions, and diabetes.
- The person should cover their mouth when coughing or sneezing and throw used tissues in a lined rubbish bin. They should wash their hands immediately.
- Everyone in the household should wash their hands (often and thoroughly) with soap and water for at least 20 seconds. Use an alcohol-based hand sanitiser if soap and water aren’t available (and if hands are not visibly dirty). Avoid touching the eyes, nose and mouth with unwashed hands.
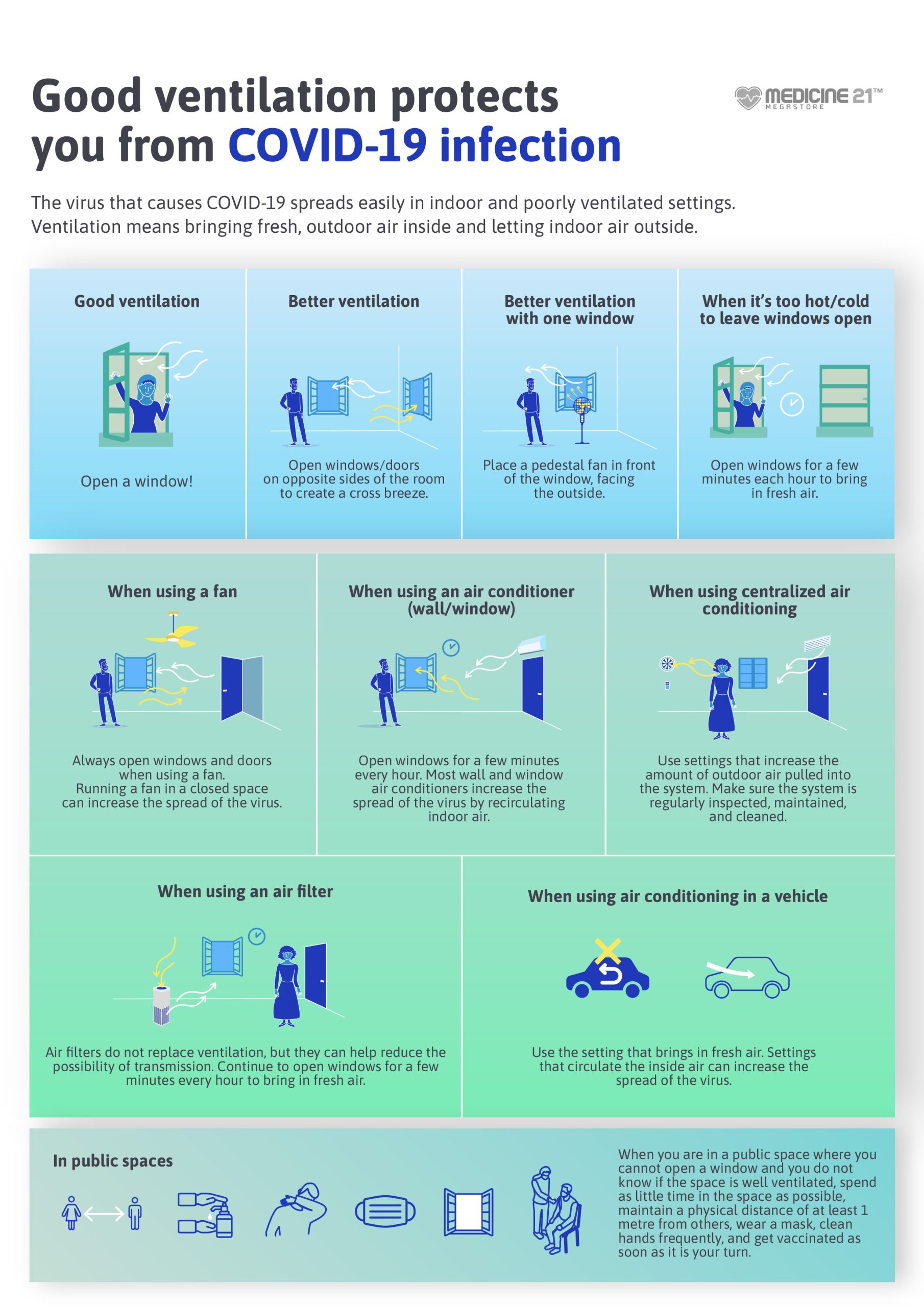
- The person with COVID-19 should also have a separate, well-ventilated room where they can sleep alone. They should use a separate bathroom if one is available. If they can’t isolate in a separate room, they should avoid sharing spaces — such as the kitchen — as much as possible.
- If your symptoms or those of the person you are looking after get worse, seek medical attention straight away.
What you will need
Ensure you have enough face masks, since you’ll need to wear one when moving through shared areas.
You’ll need cleaning products, including detergent and disinfectant, and disposable gloves, to regularly wipe down frequently touched surfaces. Buy a disinfectant that’s labelled ‘hospital-grade’ which kills viruses. You can also use a chlorine-based product such as bleach.
Place tissues, lined bins and soap or alcohol-based hand sanitiser throughout your home.
Preparing your home
Restrict visitors who don’t have an essential need to be in the home.
Shared spaces should have good air flow, such as through an air conditioner or open windows (weather permitting).
Clean all ‘high-touch’ surfaces daily, such as kitchen counters, tabletops, doorknobs, bathroom fixtures, toilets, phones, keyboards and other devices.
To make cleaning as easy as possible, reduce clutter in the home. You can also label kitchen items in the home to help avoid sharing them with the person who has COVID-19.