Hypovolemic Shock
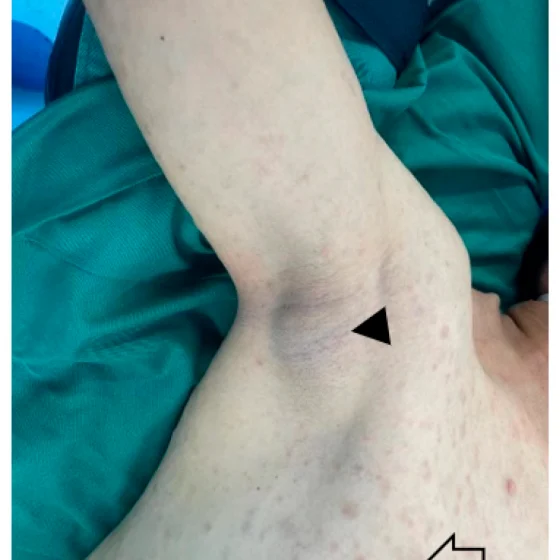
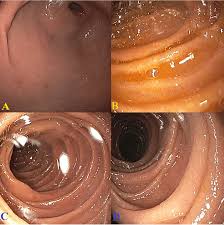
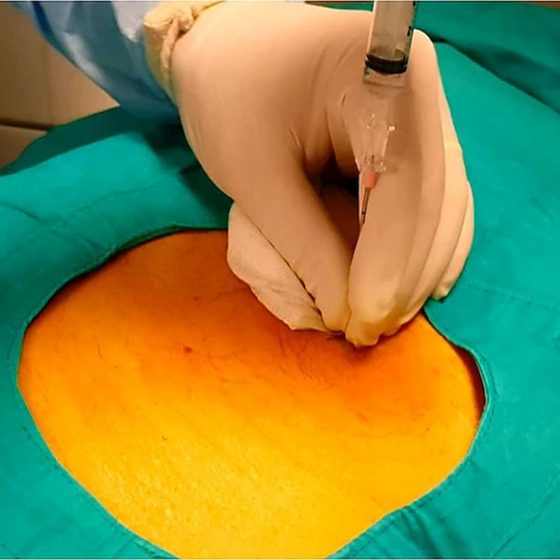
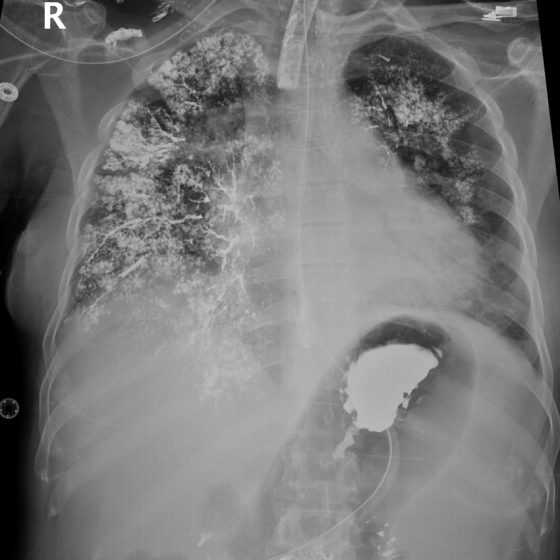
Background Hypovolemic shock refers to a medical or surgical condition in which rapid fluid loss results in multiple organ failure due to inadequate circulating volume and subsequent inadequate perfusion. Endothelium plays a critical role in vascular physiological, pathophysiological, and reparative processes. The functions of the endothelium are highly altered following hypovolemic shock due to ischemia of the endothelial cells and by reperfusion due to resuscitation with fluids. Due to oxygen deprivation, endothelial cell apoptosis is induced following hypovolemic shock. Most often, hypovolemic shock is secondary to rapid blood loss (hemorrhagic shock). Acute external blood loss secondary to penetrating trauma and