Overview
Hydrocele refers to a collection of serous fluid between the parietal and visceral layers of the tunica vaginalis.
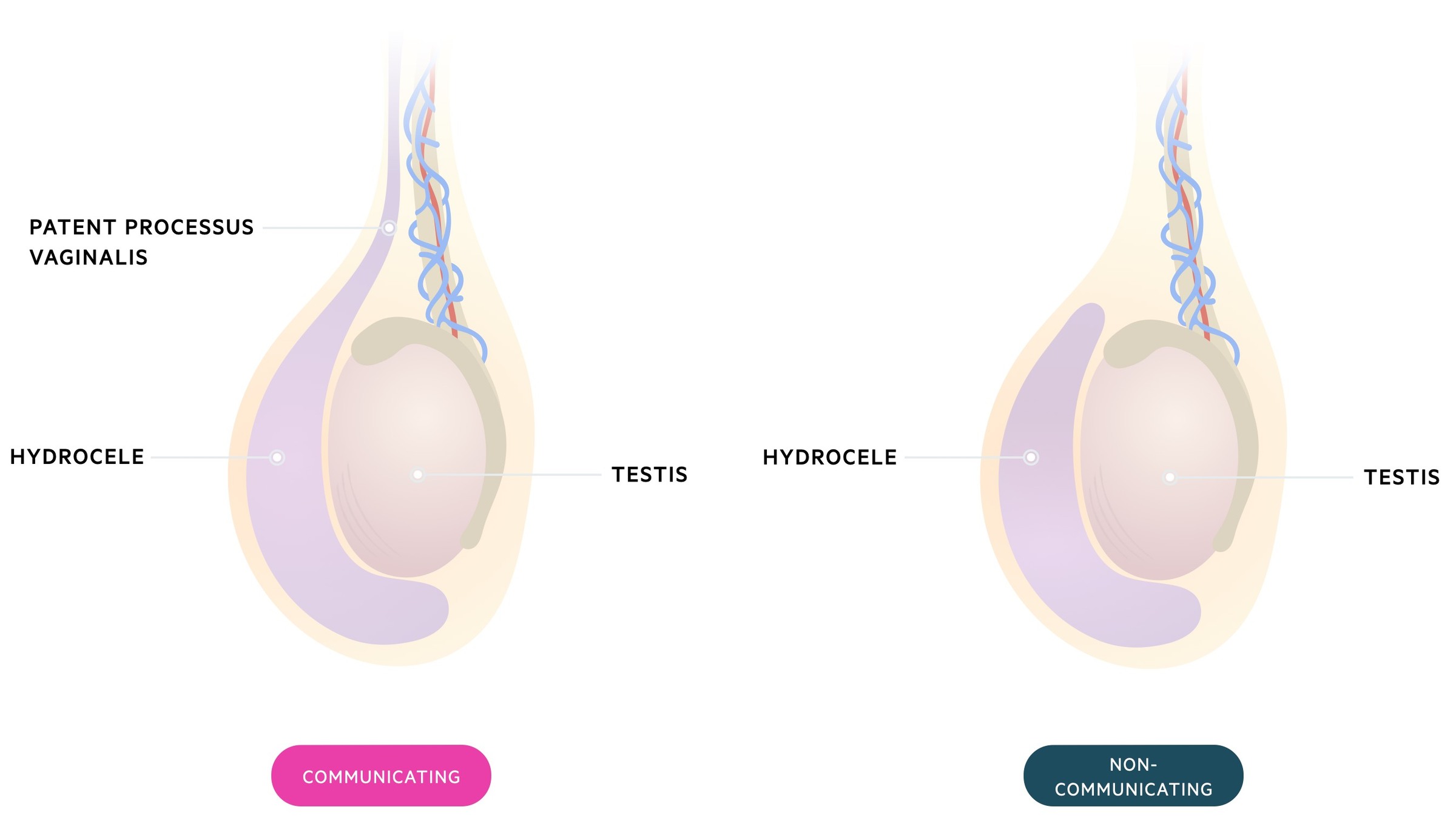
Patients present with (typically) a non-tender scrotal swelling. Hydroceles may be associated with (communicating hydrocele) or without (non-communicating hydrocele) a patent processus vaginalis.
Treatment depends on the underlying aetiology, age and symptomatic burden of the hydrocele.
NOTE: In rare cases a similar condition may be seen in women where fluid accumulates in the canal of Nuck.
Types
There are two major types of hydrocele: communicating and non-communicating.
Communicating
These occur due to the failure of normal closure of the processus vaginalis. This allows the passage of peritoneal fluid into the tunica vaginalis. Communicating hydroceles are therefore considered congenital though they may present in older children, adolescents and even adults.
It should be noted that a patent processus vaginalis is relatively common. It is estimated to be present in 80-94% of newborns and 20% of adults.
Non-communicating
There is no abnormal connection with the peritoneal cavity as seen in communicating hydroceles. Instead, fluid is produced by the mesothelial lining of the tunica vaginalis.
They occur when there is an imbalance between fluid production and absorption. Many are idiopathic but identifiable triggers include trauma, infection (e.g. epididymo-orchitis) and testicular torsion.
Others
Hydrocele of the spermatic cord: segmental closure of the processus vaginalis results in an isolated segment of fluid.
Abdomino-scrotal hydrocele: rarely a hydrocele enlarges, propagates up the inguinal canal and develops an abdominal component.
Clinical features
Patients present with scrotal swelling.
The swelling is typically described as:
- Smooth
- Non-reducible
- Demonstrating transillumination with a pen-torch
- Non-tender
It may be possible to differentiate between communicating and non-communicating hydroceles based on its features. Communicating hydroceles tend to change size and are related to ambulation (increasing when standing for prolonged periods).
In adults communicating hydroceles may present for the first time due to increases in intra-abdominal pressure, fluid overload or continuous peritoneal ambulatory dialysis.
Investigations
A testicular USS is the investigation of choice.
Testicular USS has excellent sensitivity. NICE CKS advise urgent USS if:
- It is not evident whether the scrotal swelling is testicular, or extra-testicular
- Body of testis can’t be distinguished
- Men aged 20-40 (where a hydrocele may be the first presentation of a testicular cancer)
- A haematocele does not follow trauma, or is chronic
- There is a history of trauma and scrotal pain, or persistent testicular symptoms
- There is diagnostic uncertainty
It should always be remembered that a hydrocele may occur secondary to epididymo-orchitis, testicular torsion or testicular cancer. Inguinal hernias can pass into the scrotal sac and present as an extra-testicular swelling. If these diagnoses are suspected the patient should be investigated, managed and referred based on the individual presentation.
NOTE: On the NICE CKS pages for investigation and management the age for urgent USS differs (20-34 vs 20-40) – the key message is to have a high index of suspicion for cancer and get an urgent USS.
Management
Management of hydroceles depend on the age, underlying cause, association with hernia and symptoms present.
Infants
The vast majority of simple hydroceles in infants resolve during the first year of life. Patients should have ongoing observation to ensure resolution occurs and to identify the development of an inguinal hernia. Depending on the resource reviewed different cut-offs are described from where surgical intervention should be considered:
- NICE CKS / BMJ Best Practice: advise cut-off of two years of age
- European Association of Urology: advise cut-off of one year of age
Concomitant inguinal hernia or underlying testicular pathology are also indications for referral to paediatric surgeons and early surgery. When surgery is indicated, a common procedure for an uncomplicated communicating hydrocele is an open repair with high ligation of patent processus vaginalis.
Late-onset hydroceles
In patients with suspected idiopathic non-communicating hydroceles, a period of observation may be taken. Spontaneous resolution may be seen in up to 75% of cases. Scrotal support can help adults with symptoms of discomfort. Surgery is considered where cases are persistent or symptomatic.
Communicating hydroceles that develop above the age of two are somewhat less likely to resolve and may increase the risk of an incarcerated inguinal hernia. Elective surgical management should be considered. Hydroceles secondary to infection or trauma will tend to resolve with time or treatment of the underlying cause. Hydroceles may occur as a complication of varicocelectomy (surgery to treat a varicocele). In this setting conservative management should be trialled as the vast majority will resolve with time.
Aspiration of a hydrocele is simple and may give initial relief, however, recurrence is very common. When surgery is required in older patients there are a number of options which include:
- Lord’s procedure: this involves plication of the sac. Tends to be used for small-medium sized hydroceles with a thin sac. It has a reduced risk of haematoma when compared to the Jaboulay procedure.
- Jaboulay procedure: the sac is opened drained, partially excised, everted and sutured behind the testicle. Tends to be used for larger hydroceles with a thick sac. Greater risk of haematoma.

