Overview
Acute epididymo-orchitis is a common cause of testicular pain and swelling.
It is caused by acute inflammation of the epididymis (epididymitis) that may affect the testicle (orchitis). Most commonly the aetiology is infectious through the spread of pathogens from the urethra or bladder. It may be related to urinary tract infections or sexually transmitted infections.
Testicular torsion must be considered in anybody presenting with acute testicular pain, particularly in children, adolescents and younger men. If there is any diagnostic uncertainty, refer to urology / paediatric surgery.
Aetiology
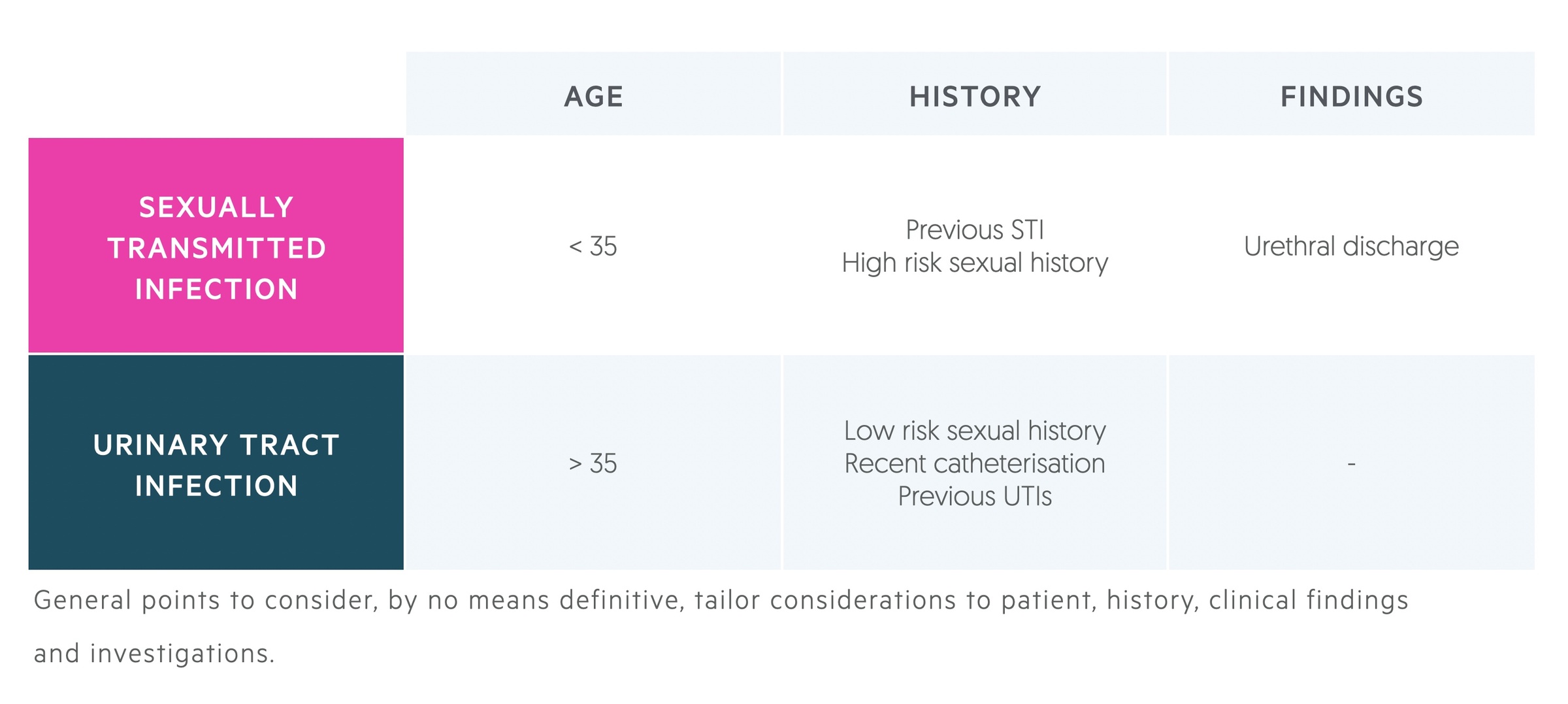
Epididymo-orchitis is most commonly caused by sexually transmitted infections or urinary pathogens.
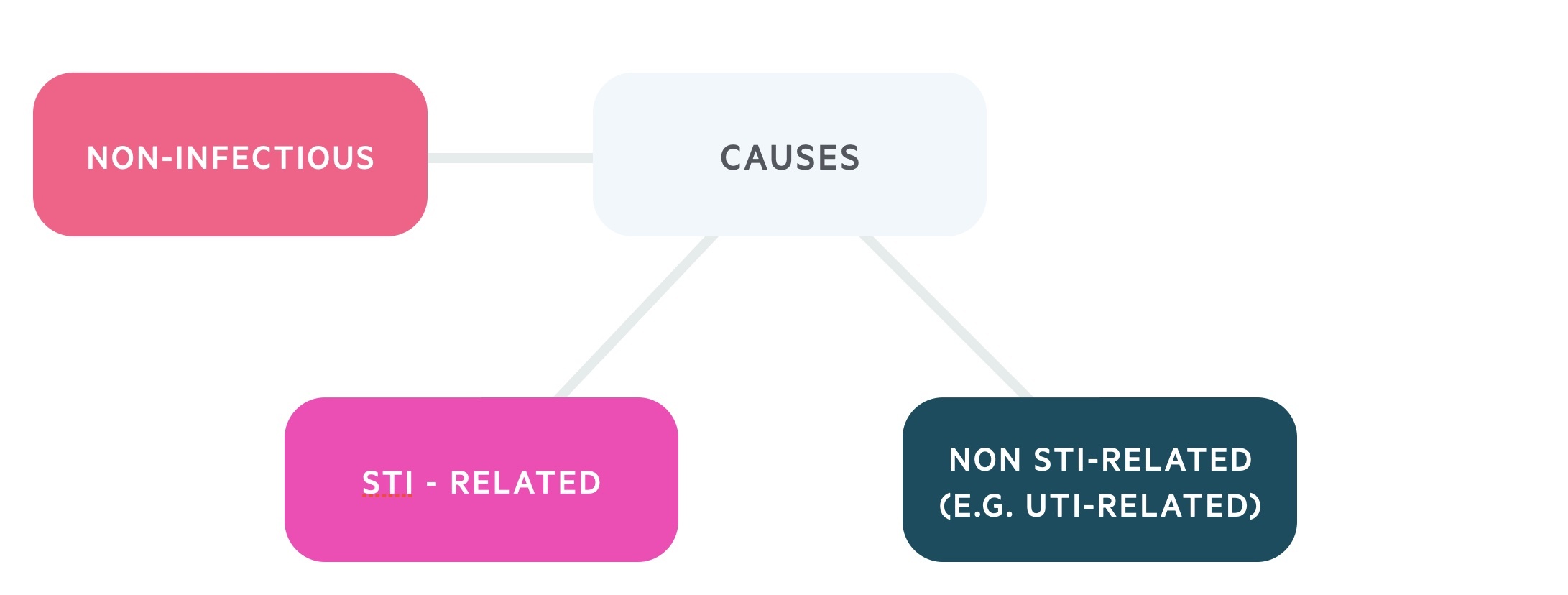
Sexually transmitted organisms tend to be considered in patients younger than 35, who have had previous STIs or are engaging in high-risk sexual activities. Urinary tract infection-related organisms tend to be considered in patients older than 35, particularly in the presence of risk factors like recent catheterisation or recurrent UTIs.
Sexually transmitted infection
- Neisseria gonorrhoeae
- Chlamydia trachomatis
- Mycoplasma genitalium
- Gram-negative enteric organisms (in those engaging in penetrative anal sex)
Non-sexually transmitted infection
- Gram-negative enteric organisms (e.g. Escherichia coli)
- Candida
- Mumps
- TB
- Brucellosis
Non-infectious
- Behcet’s disease
- Amiodarone induced
In pre-pubertal boys, epididymitis is commonly non-infective and self-limiting.
Clinical features
Patients will complain of testicular pain, signs of systemic infection may be present.
Symptoms
- Testicular pain
- Nausea and vomiting
- Fever
- Dysuria
Signs
- Testicular swelling
- Palpable, swollen, tender epididymis
- Testicular erythema
- Tender testicle
- Hydrocele (reactive)
- Urethral discharge
Consider signs and symptoms of potential underlying systemic illnesses that may cause epididymo-orchitis such as mumps and tuberculosis.
You MUST consider testicular torsion and refer urgently to urology if there is any suspicion.
Investigation
Investigations should be aimed at revealing the underlying cause.
Bedside
- Vital signs
- Urine dipstick (send MSU)
- Sexual health screen (or refer to local GUM clinic)
Bloods
- FBC
- UEs
- CRP
- Syphilis
- Bloodborne virus screen
- Mumps serology (if clinically indicated)
- Blood cultures (if pyrexial)
Imaging
USS may confirm the diagnosis, showing inflammation of the epididymis. Reactive hydroceles may be present.
USS is also useful to exclude testicular tumours, another cause of testicular pain.
Management
Antibiotics are used to treat suspected bacterial causes of epididymitis.
For the vast majority of patients, management is with antibiotics and symptomatic relief. Most can be managed on an outpatient basis but patients with signs of systemic or significant infection should be admitted for close monitoring and IV antibiotics.
General advice
- Supportive care: simple analgesia with paracetamol and NSAIDs (if no contraindication) can be recommended. Scrotal support may offer some relief.
- Sex: patients with suspected STI-related epididymo-orchitis should be advised to abstain from sex until the full results of their sexual health screen have returned.
- Safety net: patients should be advised to return if symptoms do not settle within three days (some will fail initial antimicrobial therapy), the pain worsens or they become unwell.
- Referral: an urgent outpatient USS and urology follow-up should be arranged to exclude a testicular tumour.
Antibiotics
- STI related epididymo-orchitis:
- Ceftriaxone, 500mg-1g, IM single dose AND
- Doxycycline, 100mg BD, 10-14 days
- Urinary pathogen-related epididymo-orchitis:
- Ofloxacin, 200mg BD, 14 days OR
- Levofloxacin, 500mg, OD, 10 days
NOTE: All patients being prescribed fluoroquinolones should be counseled on the risk of fluoroquinolone-induced tendon rupture. They should be avoided in patients with a history of tendon rupture related to quinolones or seizures.
Admission
Some patients develop features of systemic upset with acute epididymo-orchitis. This requires hospital admission and IV antibiotics as guided by the microbiology team.
The ‘sepsis six’ should be completed (ensure blood cultures are sent) as well as fluid resuscitation and monitoring as indicated.
Complications
Though rare, serious complications (testicular abscess, testicular infarction) may occur.
- Testicular abscess
- Testicular infarction
- Subfertility

