Overview
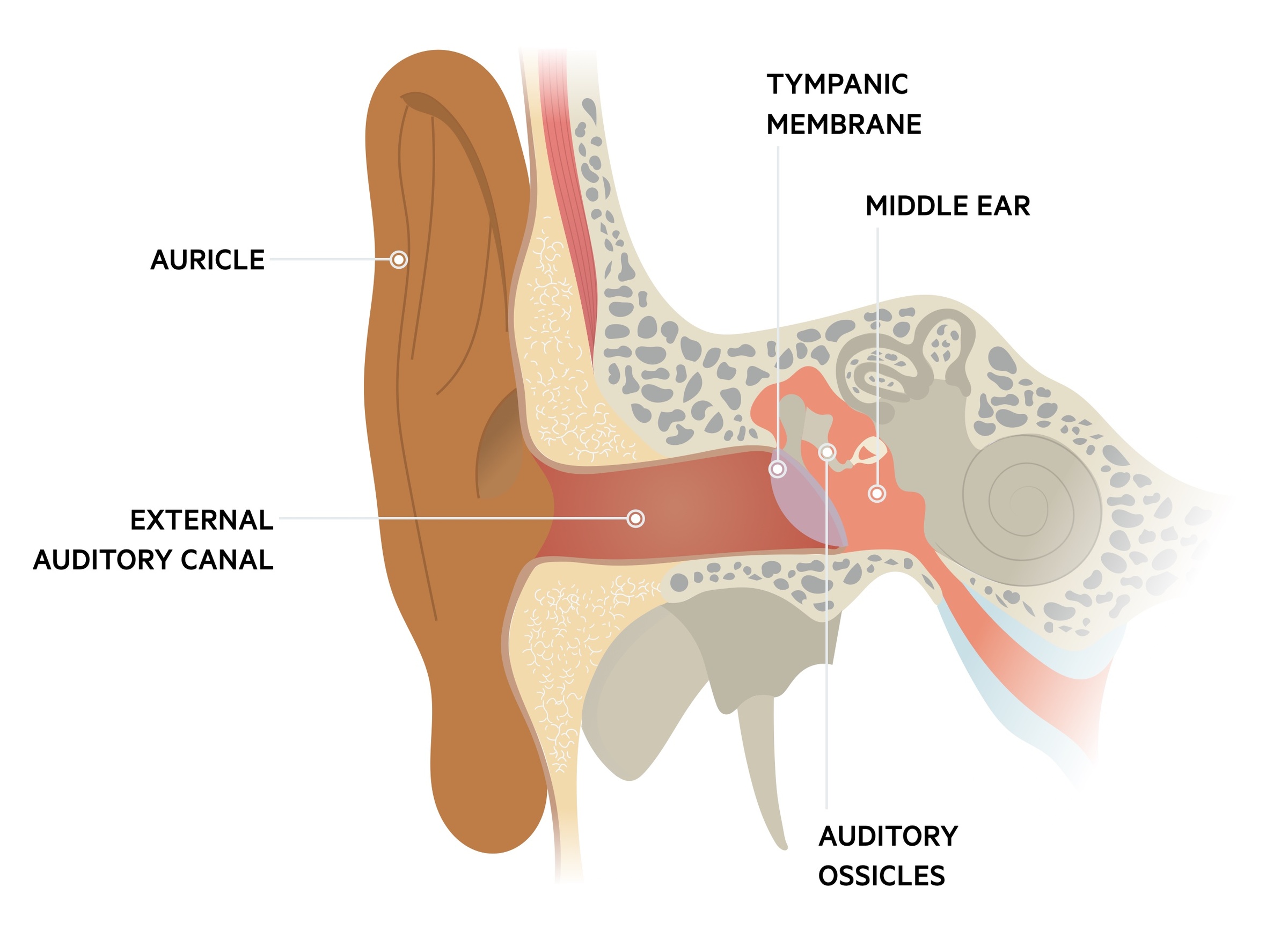
Malignant otitis externa is a serious condition where infection spreads from the external auditory canal to the skull base.
It most commonly affects the elderly, diabetic or immunocompromised. Pseudomonas aeruginosa is by far the most common causative pathogen.
Treatment is primarily with intravenous antibiotics and supportive care.
Risk factors
The majority of cases of malignant otitis externa are associated with diabetes or glucose intolerance.
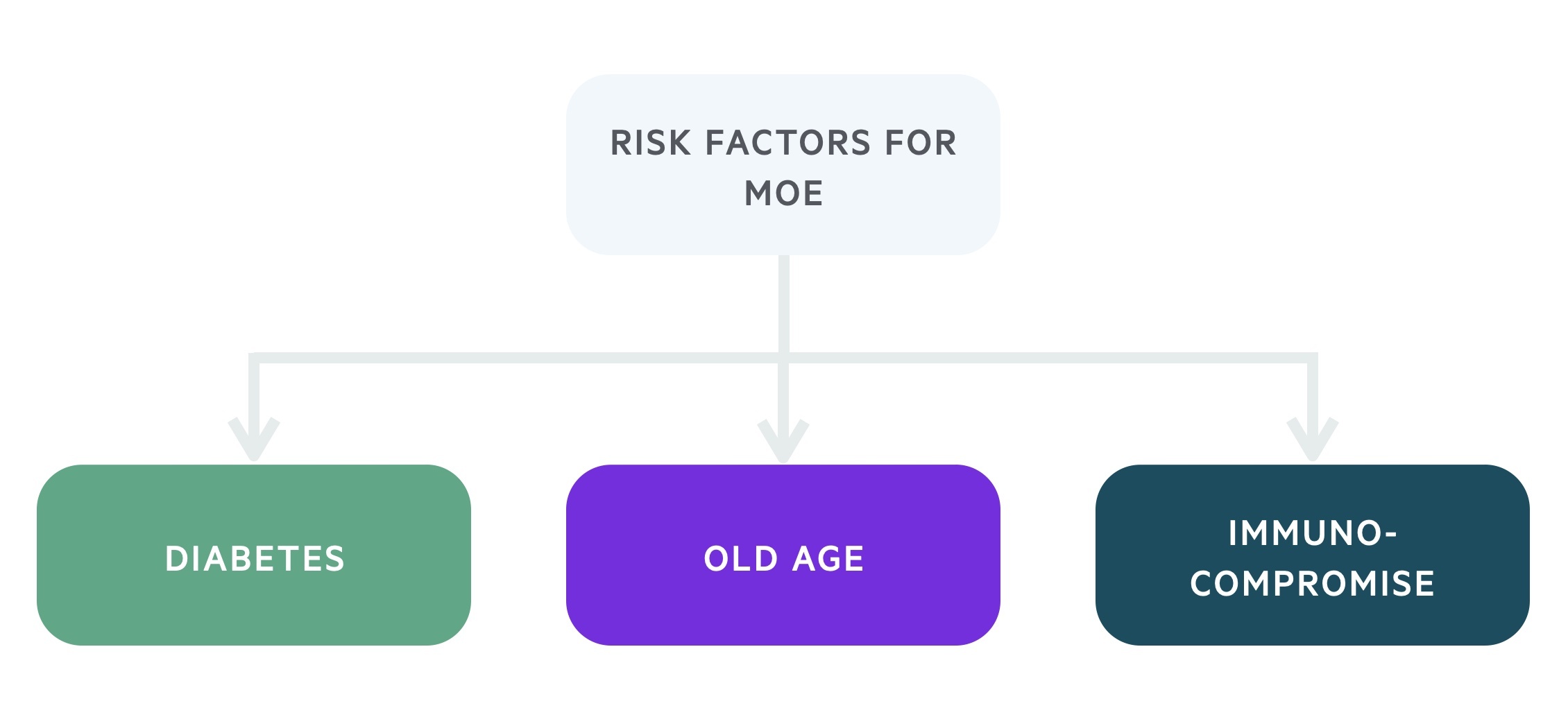
- Diabetes
- Old age
- Immunocompromise (e.g. HIV)
Aetiology
Pseudomonas aeruginosa is the most common cause of malignant otitis externa.
Pseudomonas aeruginosa is a gram-negative rod. It normally causes infections in patients with deficient immune systems or poor glycemic control.
Less commonly other pathogens are implicated. These include Enterobacteriaceae, Staphylococcus aureus, Proteus mirabilis and some fungal species (e.g. Aspergillus, Candida)
Clinical features
Patients often present with severe ear pain and signs of systemic infection.
- Ear pain (otalgia)
- Discharging ear (otorrhea)
- Jaw pain
- Night pain
- Granulation tissue (at the bone-cartilage junction of the inferior portion of the external auditory canal)
Osteomyelitis of the base of the skull and temporomandibular joint develops as infection spreads. This can result in cranial nerve palsies, commonly affecting the facial nerve.
Signs of systemic infection include pyrexia (>38oC), malaise and fatigue.
Investigations & diagnosis
Cultures and imaging (CT, Technetium-99 bone scan) are key to diagnosis.
Bedside
- Blood sugar
- ECG (if indicated)
- Pregnancy test (if indicated)
Bloods
- FBC
- Renal function
- LFTs
- CRP
- ESR
- HbA1c
Microbiology
- Discharge cultures
- Blood cultures
Imaging
CT scan: shows indicative features such thickening and enhancement of soft tissue, opacification of mastoid air cells and can provide evidence of abscess formation.
Technetium-99 (99Tc) bone scan: a nuclear medicine scan that uses 99Tc, a radionuclide tracer, to identify areas of osteoblastic activity and is highly sensitive for bone infection.
Gallium (Ga-67) scan: another nuclear medicine scan that is highly sensitive for infection and osteomyelitis.
Biopsy
May be considered particularly in treatment-resistant cases or where there is suspicion of squamous cell carcinoma.
Management
Antibiotics form the mainstay of management for patients with malignant otitis externa.
Patients with malignant otitis externa should be under the care of ENT and receive a review from a senior member of the team. Input from microbiology is essential to help guide antimicrobial care.
All patients with signs of sepsis should be managed as per the sepsis 6 protocol.
Antimicrobial therapy
Anti-pseudomonal antibiotics are commenced as empiric therapy. Local guidelines and microbiology opinions should be followed, but regimens typically involve a fluoroquinolone (e.g. ciprofloxacin). If resistant pseudomonas is cultured or suspected, Tazocin may be added to regimes. Prolonged courses, at least 6-8 weeks, are normally indicated.
Where fungal causes are identified, appropriate anti-fungal therapies should be commenced.
Surgical intervention
Surgical intervention is now uncommon. It may be used to drain a discrete abscess or take a tissue biopsy.
Hyperbaric oxygen
Though the evidence base is somewhat unconvincing, it may be used alongside antimicrobial therapy.
Complications
Patients with malignant otitis externa may develop a number of complications.
- Cranial nerve palsies: as described above the facial nerve (VII) is most commonly affected resulting in ipsilateral facial droop. As the infection spreads through the skull base cranial nerves IX, X, XI, and XII may be affected.
- Jugular vein thrombosis
- Cavernous sinus thrombosis
- Meningitis
- Brain abscess

