Psychosis is the misrepresentation of thoughts and perceptions that originate from a patient’s own mind which are experienced as reality. It is a symptom, not a diagnosis in itself and affects about 3% of the population.
Causes: With most psychiatric conditions, the aetiology of psychosis is seen with a biopsychosocial model:
Biological:
Genetics –> Twin studies have shown schizophrenia has 50% concordance rate in MZ twins
Dopamine–> Antipsychotics block D2 receptors whereas L-Dopa induces psychosis
Neurodevelopmental –> Higher in people with low birth weight, developmental delay etc.
Psychological:
Prodrome –> Often preceded by patients exhibiting anxiety, depression and ideas of reference
– These people can be offered CBT to reduce risk of progression to full psychosis
Social:
Stress –> Linked to social deprivation, urbanisation and stressful live events
Schizophrenia
This is the most famous psychotic condition which was originally called “Dementia Praecox” by Kraepelin.
– It is more frequent in men typically arising before the age of 40 and is linked with the risk factors above
In a nutshell, the main problems of schizophrenia for patients (symptoms and side effects) can be conceptualised by looking at the dopamine pathways in the brain. There are 4 main dopaminergic pathways in the brain:
Mesolimbic (VTA to NAc) –> This is involved in the reward pathway and attributing salience to a stimulus
– Excessive dopamine activity here is thought to give positive symptoms: delusions, hallucinations etc.
Mesocortical (Pre-frontal cortex) –> Dopamine here is important for executive functioning, emotion, speech
– Underactive dopamine here is thought to give negative symptoms: alogia, anhedonia, blunted affect
Nigrostriatal (SNr to Basal Ganglia) –> Dopamine here increases voluntary motor movements
– Therefore, explains why anti-psychotics (D2-blockers) lead to extrapyramidal symptoms
Tuberoinfundibular (to anterior pituitary) –> Dopamine here is responsible for reducing prolactin output
– Explains why anti-psychotics (D2-blockers) elevate prolactin release giving hyperprolactinaemia
Symptoms: These can mostly be divided into positive and negative symptoms
a) Positive – This is defined as symptom that is present through its presence
- Hallucinations – This is a perception which the patient experiences as coming from the outside world
– However, it occurs in the absence of an external stimulus
– The most common are 3rd person auditory hallucinations or voices giving running commentary
Charles-Bonnet Hallucination
- Delusions – A false belief out of keeping with the patient’s sociocultural background
– This is held with unshakeable conviction even in the face of contradictory evidence
– Most common is persecutory –> the belief that people are conspiring against you
– Delusions of reference –> the belief that people on TV/radio are talking to/about you
Specific Delusions
- Thought Disorder – an impaired capacity to sustain coherent discourse, in written or spoken language
- Catatonia – These are abnormal movements experienced by some patients:
– Waxy flexibility (you can move a patient into a position and they will remain frozen there)
– Catatonic stupor (this is where a patient suddenly stops and stays there)
- Passivity Phenomena – This is the belief that your thoughts/actions are no longer your own
– Includes thought insertion (something putting a thought into your head), thought broadcasting (everyone can read your thoughts) and thought withdrawal.
b) Negative – This is defined as symptom that is present through its absence. Remember by 5A’s:
– Affect blunted = restricted emotion with poor emotional display
– Alogia = paucity of speech
– Asociality = social isolation
– Anhedonia = Lack of pleasure
– Avolition = Lack of motivation
Diagnosis: The DSM-5 needs >2 of the following experienced for 1 months. At least 1 should include 1-3:
- Delusions
- Hallucinations
- Disorganised speech
- Disorganised or catatonic behaviour
- Negative symptoms
Subtypes: These are recognised by the ICD-10.
Paranoid – This is the most common type of schizophrenia
– Prominent hallucinations and delusions but mostly normal intellectual functioning and emotion
– Person feels very suspicious and persecuted
Catatonic – uncommon type which is characterised by prominent psychomotor disturbances
– Patient display rigidity, posturing, and abnormalities of voluntary movement
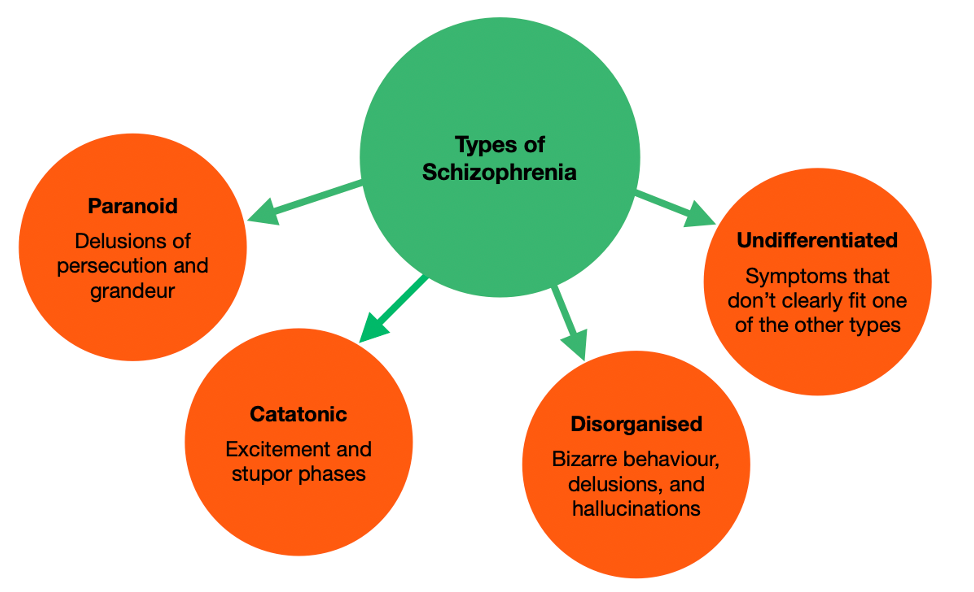
Hebephrenic/Disorganised – This has early onset, with unpredictable behaviour and speech
– Affect and mood is inappropriate with giggling, mannerisms and pranks
– Patients can also have fleeting hallucinations and delusions
Residual – A long-term subtype where most symptoms have gone but the negative symptoms remain
Undifferentiated – cannot be classified into any of the other subtypes
Management – The primary management will be oral antipsychotics in a staged approach
i) Antipsychotics –> 1st line is oral atypical anti-psychotics (quetiapine, olanzapine, risperidone)
–> 2nd line is oral typical anti-psychotics (haloperidol, chlorpromazine etc.)
–> 3rd line is clozapine, only used for psychosis refractory to other treatments
When prescribing antipsychotics, must regularly monitor weight, lipids and glucose and ECGs:
– Always start at the minimum dose with monotherapy and then titrate up the medication
– Minimum length of treatment is 6 months
– For single episode (medicate for 6-24 months)
– 2nd is 5 years medications
– 3rd is life-long medication
ii) Psychotherapy –> CBT is offered to all patients, helps to challenge delusions and develop coping strategies
iii) Social support –> Need social support for appropriate housing, financial advice
Delusional Disorder
This is a rare mental illness in which a patient experiences delusion, but with no accompanying hallucinations, thought disorder, mood disorder or flattening of affect.
Diagnosis:
Patient must show delusions in absence of any other psychotic symptoms or reversible cause (drugs)
Management:
Psychotherapy (CBT) is main line + Antipsychotics

