The commonest aetiologies of dementia are: Alzheimer’s disease, Vascular and Lewy body dementia.
– These conditions are difficult to diagnose and there are many assessment tools e.g. GPCOG, abbreviated mental test score (AMTS) and the mini-mental state examination (MMSE)
Investigation pathway:
– 1st do a cognitive assessment e.g. MOCA
– Exclude reversible causes – do FBC, U&E, LFTs, calcium, glucose, TFT, Vit B12 and folate (2)
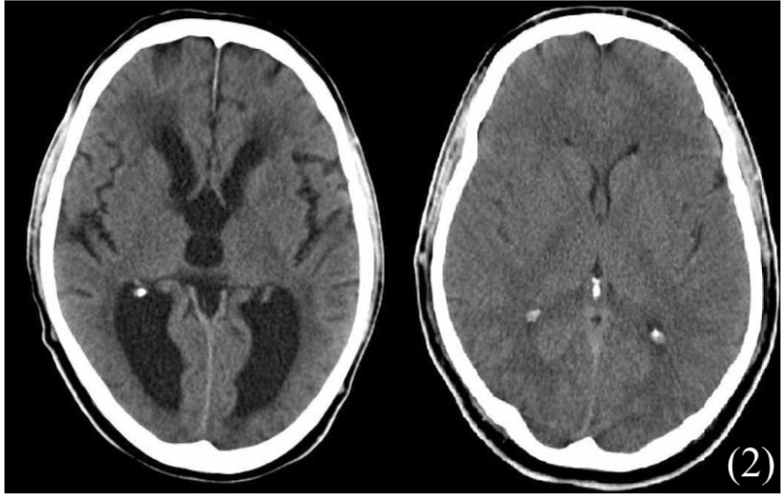
– Imaging – CT head (structural causes) and MRI (vasculature changes)
Alzheimer’s disease
The number one cause of dementia in the UK is Alzheimer’s disease. The disease is characterised by a progression degeneration of the cortex and typically occurs sporadically and in the elderly.
– Early onset AD can be seen in families (autosomal dominant mutation in presenilin) + Down’s syndrome
– Pathogenesis of the disease is controversial however it is known that the degradation product of amyloid precursor protein, B-amyloid peptide accumulates, giving rise to amyloid plaques.
– In addition, tau proteins are know to coalesce to form neurofibrillary tangles destroying ACh neurones
Symptoms:
– Memory loss (loss of memory is slow and progressive- beginning with short-term memory and later affecting long term episodic memory)
– Learned motor and language skills lost over time
– Changes in behaviour (aggression) and personality
Diagnosis:
This is based on clinical suspicion once other diseases have been ruled out
Management:
– AChE inhibitors (donepezil, rivastigmine, galantamine)
– NMDA antagonists (Memantine) used in late-stage disease
– Antipsychotics used to control severe, non-cognitive symptoms
Vascular Dementia
This is one of the most common types of dementia which occurs due to degeneration of the brain secondary to cardiovascular risk factors
– It leads to multifocal infarction in parts of the brain over a period of time leading to cognitive decline
Symptoms:
Memory loss over time
Patients may have a stepwise deterioration (e.g. after TIA/cardiovascular event)
Diagnosis:
CT/MRI scan
Management:
Control cardiovascular risk factors e.g. diabetes management, hypertension
Do not use drugs that are used in Alzheimer’s disease (e.g. AChE inhibitors)
A type of dementia which is related to Lewy Body deposition in the substantia nigra, limbic and neocortical areas. This leads to features of both Alzheimer’s disease and Parkonsons
Symptoms:
Triad of decreasing memory + Visual hallucinations + Parkinsonism ie bradycardia or rigidity
– REM sleep behaviour disorder.
Diagnosis:
Usually clinical. Reduced dopamine uptake shown SPECT (DaT scan)
Management:
AChE inhibitors (donepezil) + Memantine– Do not use antipsychotics, as these can cause irreversible Parkinsonism due to Da blockade
This is a type of frontotemporal dementia which classically affect the frontal and temporal lobe.
– It accounts for 20% of the cases of young onset dementia and is the third most common type of dementia.
– Pick bodies (round aggregates of tau protein) collect in the lobes and cause destruction of neurones.
Symptoms:
– Gives early personality change + impaired social conduct + disinhibition + increased appetite
– Age of onset before 65 + progresses slowly though there is preserved memory/visuospatial skill
This is increased CSF volume in the brain, due to imbalance between production and absorption.
– Divided into obstructive (non-communicating) and non-obstructive (communicating)
Common symptoms:
– These present with symptoms of raised intracranial pressure
– Headache (worse in morning, when lying down and Valsalva)
– Nausea/vomiting
– Papilledema
a) Obstructive
– Mechanical blockage to the drainage of CSF
– This causes dilation of the ventricles above the structural block
– Cannot use lumbar puncture as this will cause a brain herniation
Causes:
Tumours + Haemorrhage + developmental abnormalities
b) Non-Obstructive
Due to imbalance between production and absorption
Causes:
Increased production (choroid plexus tumour) or failure to reabsorb (meningitis)
c) Normal Pressure Hydrocephalus:
A special type which gives large ventricle but normal ICP
Symptoms:
– (Wet, wobbly and wacky)
– Triad of urinary incontinence, gait instability + dementia
Investigations:
1st CT head
– Lumbar puncture is used for diagnosis and therapy
Treatment:
– In acute setting, external ventricular drain (EVD)
– True long-term treatment is ventriculoperitoneal shunting, diverts CSF from ventricles to peritoneum