A premature infant is defined as a baby that is born alive before 37 weeks, which can be split into categories.
– Antenatally, mothers are given magnesium sulphate (neuroprotective) and steroids to stimulate lung maturation
– Extremely preterm = <28 weeks (these need transfer to tertiary centre)
– Very preterm = 28 – 32 weeks
– Moderate – Late preterm = 32-37 weeks
Premature babies are expected to have delayed developmental milestones. Therefore, to track their development, we need to correct the baby’s age according to how premature they were to see whether they are delayed from their expected development.
– This is done by taking the baby’s actual age in weeks (number of weeks since the date of birth) and then subtract the number of weeks your baby was preterm.
– Therefore, a baby who is 12 weeks old but 6 weeks premature will have a corrected age of 6 weeks
– The corrected age holds till about 2 years when premature babies should catch up.
Necrotising Enterocolitis (NEC)
This is an acute inflammatory injury of the distal small bowel and proximal section of the large intestine.
– It starts with feeding intolerance but can quickly lead to bowel perforation and peritonitis
– There is no known cause, but it is thought to be due to a mixture of immature intestine function, bacterial imbalance and a hyperimmune response
Risk factors:
Cow’s milk formula feeds (rather than breast milk), prematurity
Symptoms:
– Early –> Feed intolerance, Vomiting (may be bile-stained), distension
– Late –> Distended, shiny abdomen, bloody stool and respiratory distress
– Can lead to bowel perforation and shock
Tests:
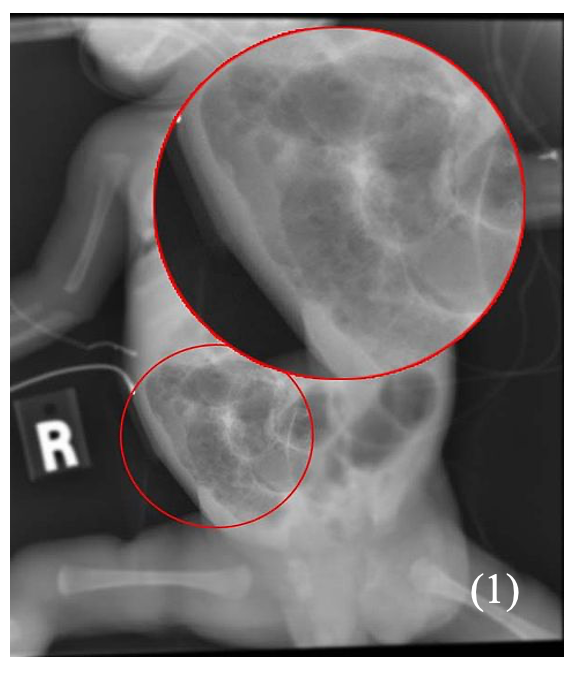
Abdominal x-ray –> air in dilated bowel, pneumatosis (air in bowel wall), rigler sign (if bowel perforation)
Management:
– Total gut rest and TPN (total parenteral nutrition)
– Antibiotics for infection risk
– If bowel perforation, laparotomy
– Once it settles down, feeds are gradually reintroduced.
Respiratory Distress Syndrome/Surfactant deficient lung disease
This is a common problem in premature infants which is due to inadequate gas exchange in the lung.
– Premature infants are deficient in surfactant due to immaturity of type II alveolar cells
– Surfactant deficiency results in decreased lung compliance (stiff lungs) and higher alveolar surface tension resulting in diffuse alveolar collapse
– This leads to poor gas and oxygen change with an increased work of breathing
Symptoms:
– Tachypnoea (> 60 breathes/min)
– Sternal and subcostal recession
– Nasal flaring
– Expiratory grunting
– Cyanosis (if severe)
Tests:
– ABG shows a respiratory acidosis
– Chest X-ray shows a diffuse granular or ‘ground glass appearance’ with air bronchograms
Management:
– Antenatally –> Glucocorticoids are given to stimulate foetal surfactant production
– Postnatally –> Oxygen + respiratory support (1st line is CPAP or HFNC, 2nd line is invasive ventilation)
–> You can also give exogenous surfactant to help increase lung compliance
Bronchopulmonary Dysplasia (BPD)
This is part of the spectrum of chronic lung diseases in premature infants.
– It describes a state in which the premature infants, usually those treated with O2, require long-term oxygen therapy
– The lung disease is thought to be from delayed lung maturation, oxygen toxicity which results in the alveoli not being mature enough to function normally
Symptoms:
– History of being treated with oxygen/mechanical ventilation
– Abnormal respiratory function with findings characteristic of BPD
– They require supplemental long term oxygen therapy
Complications:
– Increased risk of recurrent cough and wheeze and hyperinflation of the lungs
– Recurrent pulmonary infections (especially viral)
– Pulmonary hypertension which can lead to cor pulmonale
Tests:
Chest X-ray shows hyperinflation, atelectasis and cystic changes
Management:
– Supplemental oxygen and nutrition (to support growth and development)
– Antibiotics and vaccinations (for recurrent infections) and steroids to promote foetal lung development
Apnoea of Prematurity
This is a condition in which premature infants stop breathing for spells which last >20s
– This can be accompanied by hypoxia or bradycardia. They are common in preterm infants until about 32-24wks
– Apnoea’s occur frequently in premature infants due to immaturity of the central respiratory drive, impaired coordination of respiratory muscles and triggering of the chemoreceptor response.
– It is often due to an underlying cause e.g. infection, meconium aspiration, respiratory distress syndrome
Symptoms:
Absent airflow for >/=20s associated with Bradycardia (<100bpm) or cyanosis/drop is SpO2
Tests:
Infant pneumogram or infant apnoea/sleep study
Management:
It is first necessary to rule out underlying causes.
– Avoid triggering the chemoreceptor response (with careful positioning, do not flex baby)
– Give caffeine –> This is given to reduce the number of apnoeic cells
– If frequent –> may require respiratory support
Periventricular leukomalacia (PVL)
This is a white-matter brain injury that usually affects neonates, especially premature infants
– It is characterised by necrosis of the white matter near the lateral ventricles, due to a mixture of ischaemia, inflammation and free-radical release.
– Following hypoxia, coagulation necrosis occurs involving tissue dissolution and cavity (hole) formation
Symptoms:
– Motor control problems with delayed motor milestones
– May develop cerebral palsy
– May develop epilepsy and seizures
– Eye problems –> motor problems in eye control, squint, nystagmus
Tests:
Cranial ultrasound shows multiple, bilateral cysts. MRI can be used to confirm diagnosis
Management:
There are no treatments for PVL, manage complications
Germinal Matrix/Interventricular Haemorrhage
These are two related condition which refer to bleeding in the brain usually in the first 3 days of life
– The germinal matrix is the area of dividing neurones and glial cells in the developing brain, and it is located above the caudate nucleus
– It contains a network of fragile blood vessels and is very sensitive to changes in pressure and hypoxia
– As premature infants lack ability to autoregulate blood flow, they are high risk to rupture these vessels leads to haemorrhage.
– A germinal matrix haemorrhage is a small haemorrhage are confined to the germinal matrix
– An intraventricular haemorrhage is large where the bleed extends into the ventricles and can cause a hydrocephalus
Symptoms:
Depending on the size and location this can lead to several long-term neurological problems:
– Seizures
– Cerebral palsy
– Learning difficulties
Diagnosis:
Cranial Ultrasound
Management:
– The best treatment is prevention by giving dexamethasone to the mother before premature delivery
– If hydrocephalus is present –> CSF drainage may be required
– Monitor and manage long term complications
Retinopathy of prematurity
This is a potentially blinding condition which is due to the abnormal development of retinal blood vessels
junction which can lead to scarring and retinal detachment
– High concentration oxygen or hypotension causes vasoconstriction of the vascular retinal area
– The decreased blood flow causes a down-regulation of growth factors
– After, neovascularisation occurs giving aberrant retinal vessel growth (due to VEGF excess)
Risk factors:
Use of high concentration oxygen in intensive care unit
Symptoms:
– Can be mild and resolve spontaneously
– Can lead to Retinal detachment, fibrosis and blindness
Management:
– Preterm infants (<32 weeks or <1.25kg) are screened by ophthalmologist
– Peripheral retinal ablation by laser photocoagulation can be used to treat

