These shunts due to not cause cyanosis at birth, as the pressure in the left circulation is more than the right
– The increased pressure in the pulmonary circulation leads to remodeling and pulmonary hypertension
– This causes right ventricular hypertrophy and will eventually cause a reversal to a right-to-left shunt
– This is called Eisenmenger’s syndrome which occurs about 10-15 years
– This is a progressive condition which will lead to heart failure usually at the age of 40 if left untreated
Atrial septal defect (ASD)
This is a defect which leads a residual hole between the two atria.
– A failure to close the flaps leaves a patent foramen ovale. In the neonatal heart, pressure is higher in the LA than RA, so blood is shunted from left-to right atrium
Development of the Atrial Septum

The atrial septal defect exists in two main types:
i) Ostium primum – This is a defect at the bottom of the atrial septum
– Occurs when septum primum does not grow all the way down
ii) Ostium secundum – This is a defect in the centre of the atrial septum which is more common
– Occurs when the septum secundum does not grow enough during development

Symptoms:
– Most are asymptomatic and go undetected for many years
– Increases the risk of chest infections
– Gives fixed splitting of S2 ( due to a delay in the closing of the pulmonary valve)
– Can cause an ejection systolic murmur loudest at upper left sternal edge (due to increased flow across the P valve)
Complications:
– Paradoxical emboli –> Embolism from the venous system passes through foramen ovale to the left side of the heart entering the systemic circulation and causing a stroke
Diagnosis:
– Echocardiogram
– ECG –> this can show right bundle branch block with axis deviation
– CXR –> may show cardiomegaly and enlarged pulmonary arteries
Management:
– Small ASDs may close on their own so many only require monitoring
– ASDs large enough to cause symptoms or right ventricular dysfunction will require surgery or cardiac catherization
Ventricular septal defect (VSD)
This is a hole which connects the ventricles which is the most common congenital heart defect.
– VSD can also be acquired and is a complication of myocardial infarction
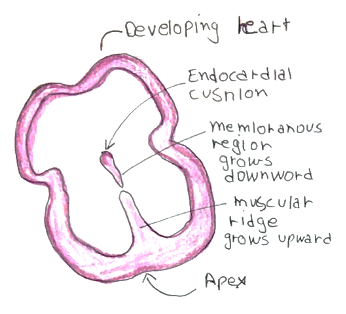
– During development, a muscular ridge of tissue grows upwards from the apex
– This fuses with a thinner membranous region coming down from the endocardial cushion
– If they don’t fuse properly, a gap remains leaving a defective ventricular septum
– In the neonatal heart, pressure is higher in the Left ventricle than the right ventricle
– Therefore, VSDs result in shunting of blood from the left to the right
Symptoms:
If small VSD:
– Most of these are symptomatic
– Pansystolic murmur at lower left sternal edge (loud murmur implies smaller defect) with a quiet P2
If large VSD:
– Gives symptoms of heart failure (breathless, poor growth)
– Predisposes to recurrent chest infections
– Gives either no murmur or soft pansystolic murmur with a loud P2
– The louder the murmur is, the narrower the hole and less severe the disease
– If left untreated will progress to Eisenmenger’s syndrome
Diagnosis:
Echocardiogram
Management:
Medical management of heart failure followed by surgery to close hole if large
Patent ductus arteriosus (PDA)
This is a condition which is defined as a failure of the duct to close by a few days after birth 1
– During embryological development, the ductus arteriosus allows blood to flow from pulmonary artery to aorta bypassing lungs.
– In term infants, in normally closes shortly after birth due to increased pulmonary flow (this enhances clearance of maternal prostaglandins which maintain duct patency)
– But a failure of the ductus arteriosus to close results in left-to-right shunt between the aorta and the pulmonary artery, as the pressure is higher in the aorta than pulmonary artery
– It is associated with prematurity and maternal rubella infection

Symptoms:
– Asymptomatic at birth with no cyanosis
– However, if left untreated can lead to Eisenmenger syndrome and heart failure later in life
– Continuous ‘machine-like’ murmur described as “rolling-thunder” with a left sub-clavicular thrill
– Wide pulse pressure
– Heaving apex beat
– Poor growth
Diagnosis:
Echocardiography
Management:
– Indomethacin –> inhibits prostaglandin E synthesis causing closure of the ductus arteriosus
– If very large or persistent, requires surgical repair

