Acute Otitis Media
This is an infection of the middle ear which is usually seen in children, due to Eustachian tube dysfunction
– It usually occurs with a history of an URTI (S. Pnemoniae) giving fever and cough
Symptoms:
Earache, fever, irritability and diarrhoea, but can lead to tympanic membrane perforation
Management:
1st line is 5-7-day course of amoxicillin (but strict antibiotic guidelines, only give if:)
a) Systemically unwell or high risk of complications
b) Younger than 2 years with bilateral otitis media
c) Otorrhoea (discharge after ear drum perforation)
d) If none of the above but if symptoms do not improve after 3 days (use back-up prescription)
If a child is having recurrent otitis media, they may have a tympanostomy tube (grommet) inserted to reduce the risk of glue ear.
Otitis Media with effusion (Glue Ear)
This is inflammation of the middle with fluid accumulation in the middle ear and mastoid air cells due to a negative pressure balance due to dysfunction of the Eustachian tube
– This is often a complication of acute otitis media caused by a viral or bacterial infection
– Apart from the infection, the problem is that the fluid can lead to a conductive hearing loss as it reduces sound wave vibrations in the middle ear
– In children, this can lead to problems like speech and language delay
Symptoms:
– Can be asymptomatic except reduced hearing
– Secondary problems like speech and language delay and balance problems in children
Diagnosis:
– On examination, see a retracted ear drum with a possible fluid level
– Audiometry –> may show conductive hearing loss
Management:
– Antibiotics. If severe, consider tympanostomy tubes and possible adjuvant adenoidectomy
Adenoidal hyperplasia
This is enlargement of the adenoid (pharyngeal) tonsils which can lead to partial obstruction of the nasal airway.
– Adenoidal tonsils increase in size until about 8 years of age and then gradually regress
– In young children between 2-8 years, , the adenoids grow faster than the airway narrowing the lumen
– This reduces airflow in the airway predisposing to certain infections
Symptoms:
May be asymptomatic
– Obstruction of airflow –> children become mouth breathers, changes to the voice
– Infection risk –> recurrent episodes of otitis media, sore throat and cough
Diagnosis:
Nasal endoscopy is used to visualise the adenoids
Management:
Adenoidectomy if obstructive sleep apnoea or recurrent otitis media with effusion
Choanal atresia
Choanal atresia is a congenital disorder where the back of the nasal passage (choana) is blocked
– It is due to problems in the bony and soft tissue leads to obstruction of the nasal passage
– It usually presents at birth and is associated with having other defects like learning disabilities and colobomas
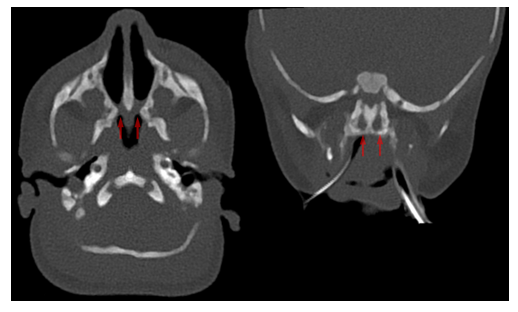
Symptoms:
– If unilateral –> usually asymptomatic
– If bilateral –> presents early with breathing difficulties e.g., cyanosis (as neonates are nose breathers)
– This includes cyanosis and when eating is later resolves when crying
Diagnosis:
– Clinical Examination
– CT scan is used to provide definitive diagnosis
Management:
– Surgery (fenestration procedures) to open the airway and keep it patent
Allergic Rhinitis
This is inflammation of the mucous membranes which is caused by an allergic reaction.
– It can be atopic (IgE antibodies to inhaled allergens) or non-atopic.
– It is classified into intermittent vs persistent, mild vs severe and seasonal vs perennial (all the time)
– It is associated with atopic conditions, eczema, asthma, sinusitis, and adenoidal hypertrophy
Symptoms:
– Coryza –> runny nose, sneezing, tickly throat
– Conjunctivitis with runny and itchy eyes
– Blocked nose with feeling of obstruction (this may disturb sleep and concentration)
– Can lead to chronic cough due to post-nasal drip
Management:
– 1st line is 2nd generation non-sedating antihistamines e.g., loratadine
– Corticosteroid nasal spray for nasal symptoms
– Sodium cromoglicate eye drops for eye symptoms
– If persistent, leukotriene receptor antagonist
– Nasal decongestants –> used for <10days due to rebound effect
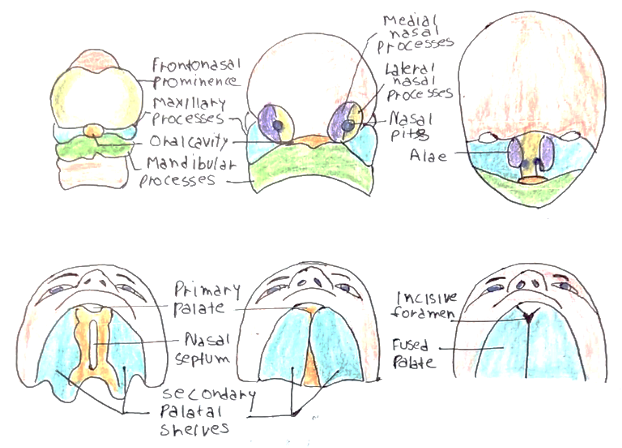
Cleft lip and palate
This is the most common congenital facial abnormality
– Cleft lip occurs due to a failure of the fronto-nasal and maxillary processes to fuse in development
– Cleft palate occurs due to a failure of the palatine processes and the nasal septum to fuse
– It is associated with maternal anti-epileptic use
Symptoms:
– Visual deformity
– Feeding difficulties
– Speech problems
– Delayed development of the teeth
– Increased risk of otitis media (for cleft palate)

Diagnosis:
– Ultrasound antenatally –> 20-week anomaly scan
– Postnatally on NIPE (new-born infant physical examination)
Management:
This must be corrected surgically at specific ages
– Cleft lip –> Surgery in the first 2-3 months (preferred is 10 weeks)
– Cleft palate –> Surgically between 6-12 months
Hearing loss
There are many conditions which lead to hearing problems in children
– These include genetic, infective and acquired conditions
Causes:
– Conductive hearing loss –> Otitis media with effusion (glue ear), Down’s syndrome
– Sensorineural hearing loss –> Congenital infections (rubella), meningitis, Usher Syndrome
Diagnosis:
There are many different tests that children have at each stage of development to check hearing
– Newborn –> Otoacoustic emissions test (part of the Newborn Hearing Screening Programme)
– If this is abnormal –> do auditory brainstem response test
– 6-9 months –> Distraction test (performed by the health visitor)
– >3 years –> Pure tone audiometry done as child enters school
Management:
– Treat the underlying condition if reversible
– If irreversible, child will require hearing aids, cochlear implants or start learning sign language to communicate

