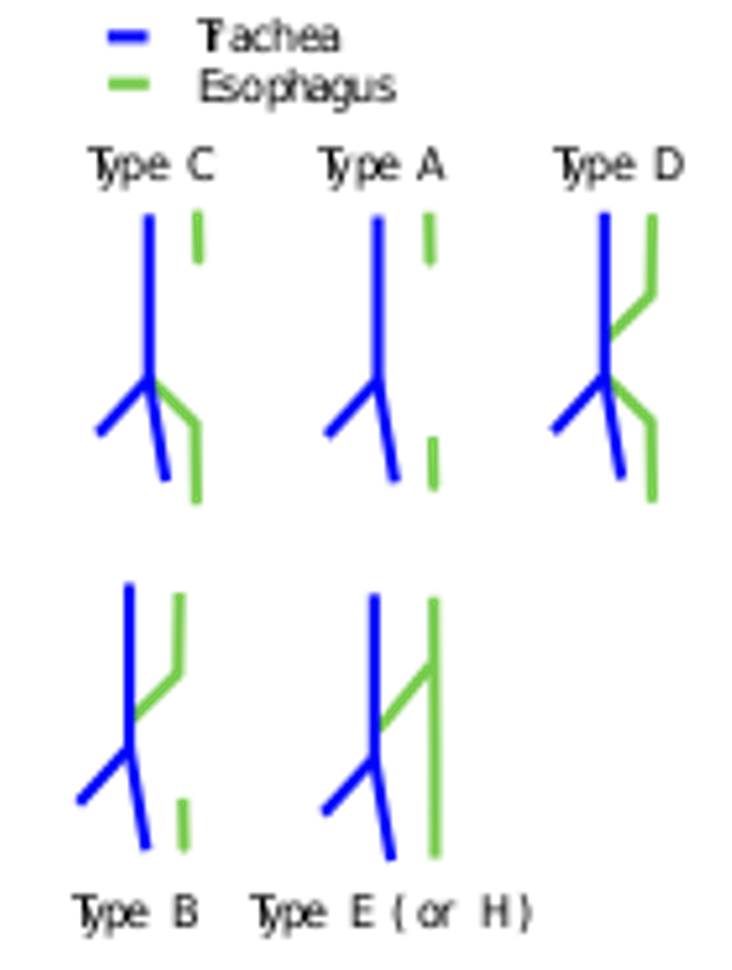
Tracheo-oesophageal fistula
This is a congenital defect which results in a connection between oesophagus and trachea
– During early development, the oesophagus and trachea begin as a single tube
– Normally, this tube divides into the 2 tubes in the first trimester of pregnancy
– If this separation does not occur properly this leads a residual connection allowing food to enter the oesophagus.
– Most common defect is proximal oesophageal atresia and distal oesophagus arising from trachea
Symptoms:
Antenatal:
– Polyhydramnios (excess amniotic fluid in utero as baby cannot swallow fluid)
– Absent stomach bubble on antenatal US (due to OA)
Postnatal:
– If Oesophageal Atresia –> Drooling and Coughing and choking during feeding
– If fistula –> coughing, respiratory distress, cyanosis when eating
This condition is associated with a type of disorder that affects many body systems, called the VACTERL association
VACTERL Association
Diagnosis:
A nasogastric tube is used to see if it can reach the stomach. If not, this indicates oesophageal atresia
Management:
Surgical correction
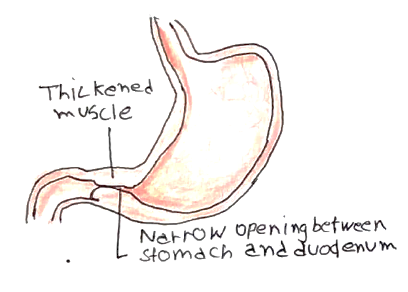
Pyloric stenosis
This is congenital hypertrophy of pyloric sphincter, which presents in the first month of life
– It is more common in males, usually affects the first born and a significant proportion have a positive family history
Symptoms:
– Projectile non-bilious vomiting, about half an hour after feeding
– Constipation and dehydration
– Olive-live mass in the abdomen
– Hyperchloremic, hypokalemic alkalosis due to the vomiting
Diagnosis:
Ultrasound
Management:
Ramstedt pyloromyotomy (surgical removal of smooth circular muscle)
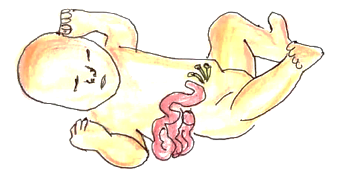
Gastroschisis
This is a congenital malformation of the anterior abdominal wall just lateral to the umbilical cord
– This leads to exposure of bowel/stomach out of the abdominal wall without covering sac
– Can lead to severe dehydration and protein loss
Diagnosis:
Seen antenatally (20-week anomaly scan) and postnatally
Management:
– You can deliver the baby vaginally
– Cover abdomen in clear occlusive wrap (minimise fluid/heat loss)
– This required urgent surgical correction immediately after birth
Exomphalos
This is a condition like gastroschisis. However, the abdominal contents covered by the amniotic sac
– The amniotic sac membrane is protective and protects against severe dehydration and protein loss
– It is associated with disorders which lead to the overgrowth of organs, such as Beckwith-Wiedemann syndrome
Diagnosis:
Seen antenatally (20-week anomaly scan) and postnatally
Management:
– Delivery the baby by Caesarean section
– This requires surgical repair in stages
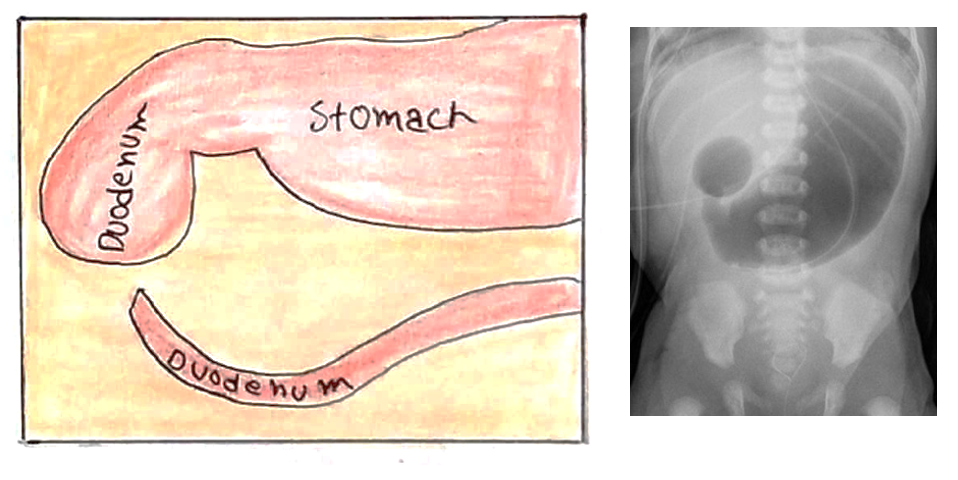
Duodenal atresia
This is a condition in which the duodenum has a dead end cut off after the stomach and is unconnected to the rest of bowel
– This obstructs the passage of food and secretions and so resembles small bowel obstruction.
– It is associated with Down’s syndrome
Symptoms:
– Polyhydramnios in utero
– Bilious vomiting and abdominal distension a few hours after birth
Diagnosis:
– Abdominal X-ray shows ‘double bubble sign’ (due to distended stomach and proximal duodenum)
Management:
– NG tube and IV fluids (“Drip and suck”)
– Urgent surgical correction to join the proximal duodenum to the distal duodenum
Meckel’s Diverticulum
This is an outpouching of the ileum which occurs due to failure of the vitelline duct to involute.
– It follows the rule of 2s –> seen in 2% of people, usually 2 inches long and within 2 feet of ileocecal valve and it is twice as prevalent in males than females and seen in very young children around the age of 2
– It contains remnants of gastric and pancreatic tissue and can secrete stomach acid
Symptoms:
Most cases are asymptomatic but can cause a variety of presentations
– Bleeding -> acute, painless rectal bleeding
– Small bowel obstruction (acts as a lead point for intussusception)
– Meckel’s diverticulitis –> clinically identical to appendicitis

Diagnosis:
This depends on the presentation
– If bleeding –> technetium-99 scan (demonstrates increased uptake by ectopic gastric mucosa)
– If small bowel obstruction or Meckel diverticulitis –> CT abdomen is investigation of choice
Management:
– Laparotomy and removal
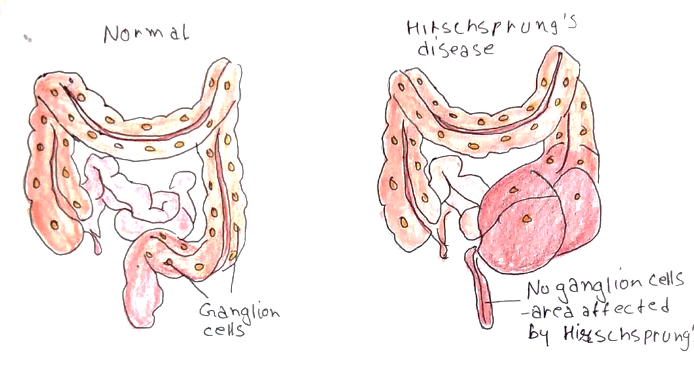
Hirschsprung disease
This is a condition in which there is a error in the development of the nervous plexuses which supply the distal segment of the large bowel.
– It is caused by poor migration of the crest cells to this area resulting in an aganglionic segment of large bowel
– Without these nervous cells, this means that there is no innervation of the smooth muscle meaning that effective peristalsis cannot occur
– This abnormal segment is therefore left narrow and contracted and food becomes obstructed here
– The normal segment of bowel proximal to the aganglionic segment will be dilated as food collects here
Symptoms:
– Delayed passage of meconium (>48 hours after birth)
– Signs of bowel obstruction –> abdominal distension, bilious vomiting
– Poor growth
– Chronic constipation in childhood
Diagnosis:
– Rectal examination –> shows narrowed segment and gush of liquid stool/flatus on withdrawal of the examining finger
– Suction rectal biopsy –> this shows Absence of ganglion cells and Presence of large acetylcholinesterase-positive nerve trunks
Management:
– In the acute setting, bowel irrigation
– Surgery (anorectal pull through aganglionic segment removed and then you anastomose normal bowel to the anus)
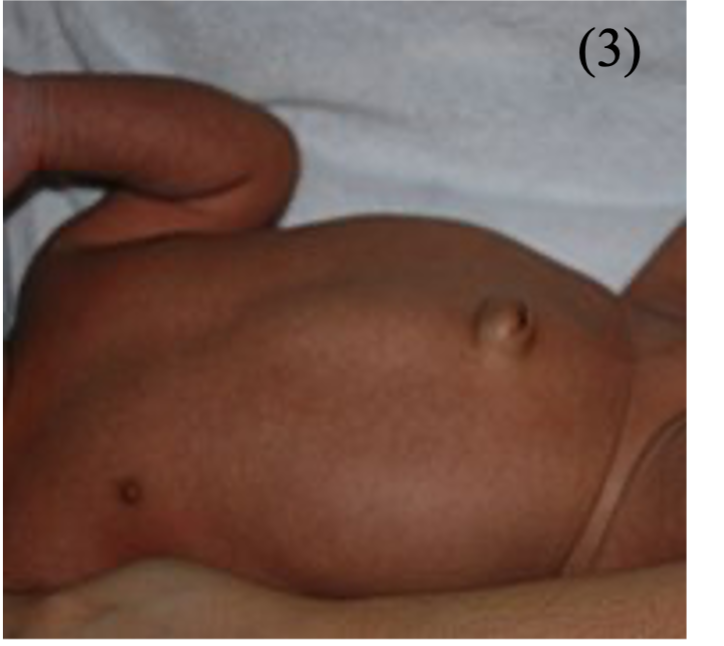
Umbilical Hernia
This is a herniation of the bowel content through the umbilicus. It is a common finding in neonates and usually asymptomatic
– It is associated with Down’s syndrome
Symptoms:
Usually asymptomatic
Diagnosis:
Clinical diagnosis
Management:
No treatment is required as they usually self-resolve in the first few years
Malrotation
This describes a failure of the normal sequence of rotation of the bowel:
– The caecum remains high in the midline and fixed to the posterior abdominal wall
– This can lead to duodenal obstruction in 2 ways: Small bowel volvulus (which can lead to SMA compromise) or extrinsic compression from Ladd’s bands (peritoneal bands that cross the duodenum anteriorly)
– It usually presents in the first week of life
Symptoms:
– Obstructive symptoms –> bilious vomiting, distension
– Can give bowel ischaemia –> abdominal pain and tenderness
Diagnosis:
Upper GP contrast study
Management:
Surgical correction (Ladd’s procedure)

