During pregnancy there is also development of the breast tissue to prepare for breastfeeding.
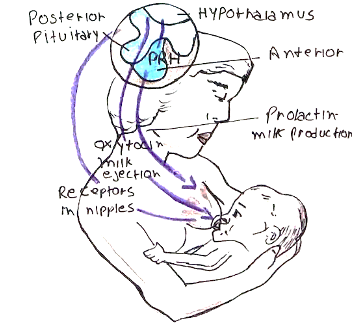
– After delivery of the placenta, the low progesterone and high prolactin stimulate milk secretion
– Prolactin –> stimulates lactogenesis and disrupts the pulsatile GnRH secretion (natural contraception)
– Oxytocin –> stimulates milk ejection from the breast as well as uterine contractions
Milk contains all the nutrients the infant needs (except vitamin D and K) up till 6 months of age.
– It is divided into the colostrum (first milk produced) and mature milk:
Colostrum:
– First milk produced that is rich in proteins and immunoglobulins.
Mature milk:
– Contains proteins, lactose, fats, minerals, trace elements and vitamins
– Proteins and cells that provide passive immunity
– Secretory IgA, lactoferrin and lysozymes.
– Lymphocytes and macrophages.
– Bacteria that contribute to neonates’ GI flora.
There are many benefits of breast feeding for mother and infant:
Maternal:
– Faster uterine involution, bonding, contraception,
– Protection from breast/ovarian/endometrial cancer.
Infant:
– Lower incidence of diarrhoea, necrotising enterocolitis (NEC),
– Lower incidence of otitis media and respiratory tract infections
It is possible for some drugs to pass in the breast milk to the baby, remembered by the acronym SPAM-CAA:
Sulfonylureas
Psychiatric drugs: lithium, benzodiazepines
Antibiotics: ciprofloxacin, tetracycline, chloramphenicol, sulphonamides
Methotrexate
Carbimazole
Aspirin
Amiodarone
Breastfeeding Complications
Many mothers might struggle with breastfeeding due to poor technique. There can also be additional complications caused by certain types of infections (S. Aureus, Candida) and blockage of the ducts:
Engorgement
– This occurs when a mother produces more milk than her infant uses.
– This can lead to the breast tissue becoming swollen, firm and red making it difficult for infant to attach
– It causes mild to extreme pain which is typically worse just before feeding
– It usually occurs in the first few days after birth affecting both breasts
– If untreated, can lead to blocked milk ducts, mastitis and impact the milk supply
Management:
Encourage expression of milk to relieve the pressure.
Raynaud’s disease of the nipple
– This condition involves spasm of the arteries which supply the nipple
– This leads to intermittent pain which is present during and immediately after feeding.
– Blanching of the nipple may be followed by cyanosis and/or erythema
– The nipple pain resolves when nipples return to normal colour
Management:
– Minimise exposure to the cold, using heat packs after breastfeeding, stop smoking
– If symptoms persist, you can consider nifedipine
Mastitis
This is a condition that refers to inflammation of the breast
– It is associated with breastfeeding: milk stasis can cause an inflammatory response
– Women can then develop a secondary infection, most commonly with staphylococcus aureus
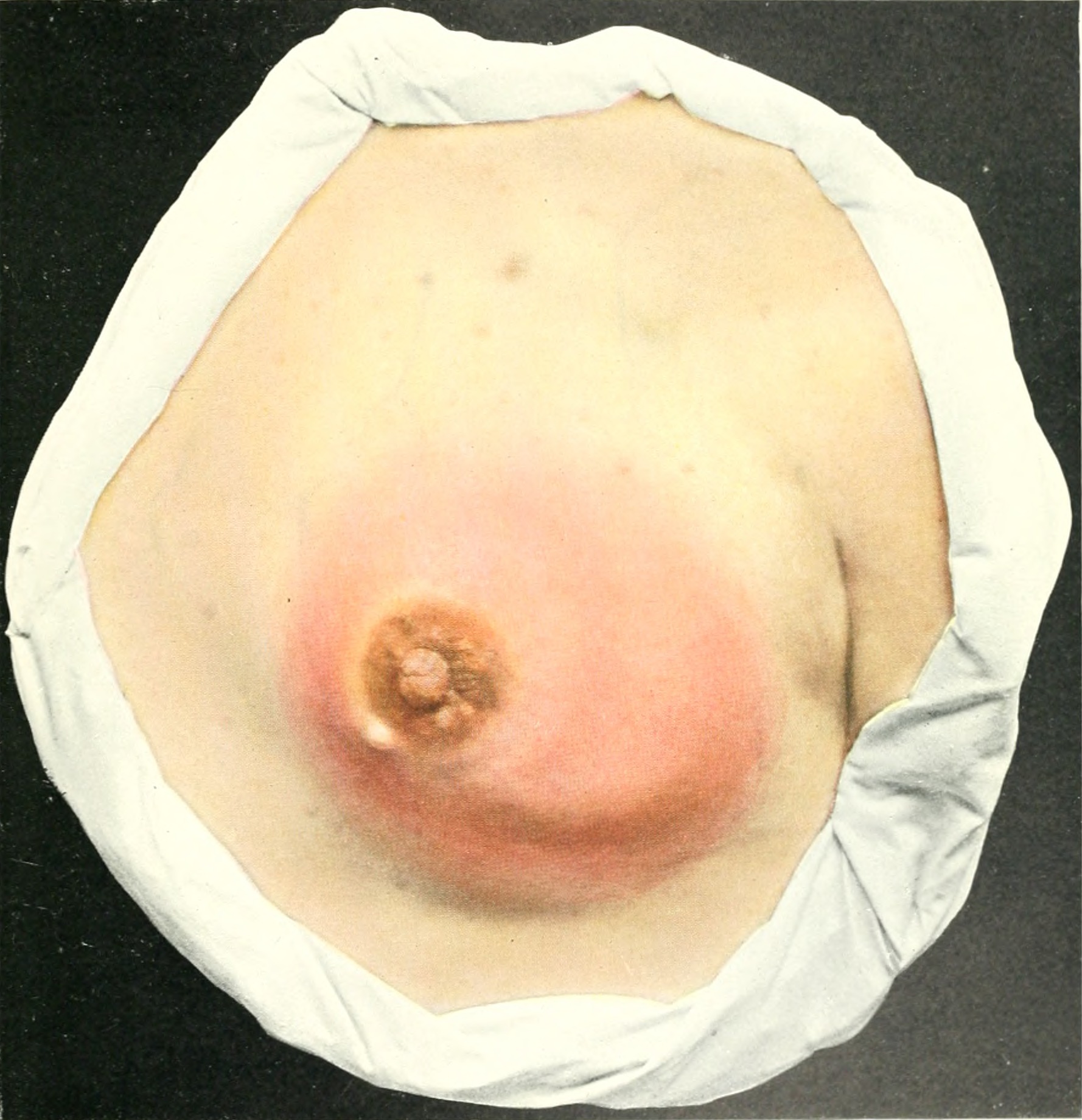
Symptoms:
Erythematous, tender, swollen area of breast
– Systemic upset with fevers, chills and fatigue
Management:
– 1st line is to advise continue breastfeeding, ensuring the breast is fully emptied
– If symptoms do not improve after 24 hours of milk removal –> Flucloxacillin 10-14 days

