Introduction
Obstetric haemorrhage, which includes both antepartum and postpartum haemorrhage, is the leading cause of maternal death worldwide.
Within the UK, maternal death from obstetric haemorrhage is uncommon, but still causes approximately 7 deaths per year.
Postpartum haemorrhage refers to vaginal bleeding up to 12 weeks following delivery. Prompt recognition and management is key to good outcomes. It should be remembered that earlier antepartum haemorrhage can reduce a patient’s physiological reserve and ability to compensate for bleeding in the postpartum period.
Classification
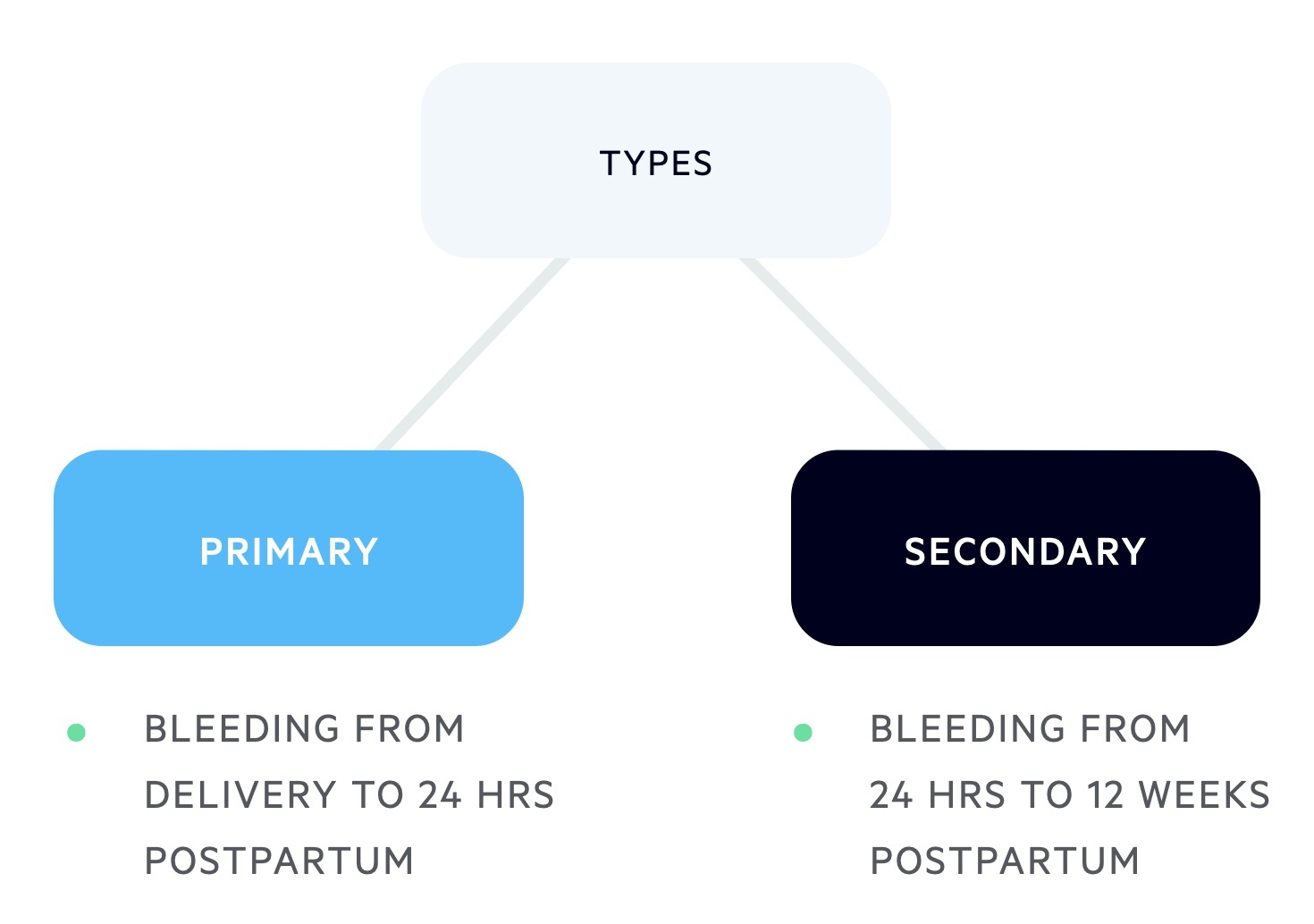
Postpartum haemorrhage (PPH) can be classified as either primary or secondary.
- Primary PPH: is defined as vaginal bleeding that occurs from delivery of baby to 24 hrs postpartum.
- Secondary PPH: is defined as vaginal bleeding from 24 hrs postpartum to 12 weeks postpartum.
Severity
PPH can be graded as minor, moderate and severe.
The severity of PPH is dependent on the extent of blood loss and can be divided into minor, moderate or severe. The extent of blood loss in PPH is often underestimated.
- Minor: 500-1000mls
- Moderate: 1000-2000mls
- Severe: > 2000mls.
Risk factors
Risk factors for the development of PPH can be divided into both antepartum and intrapartum factors.
Antepartum
Major antepartum factors include multiple pregnancy, antepartum haemorrhage and previous history of PPH. Below is a list of the main risk factors for PPH:
- Abruption
- Placenta praevia
- Multiple pregnancy
- Pre-eclampsia, gestational hypertension
- Previous PPH
- Ethnicity (i.e. Asian)
- Obesity (i.e. BMI > 30)
- Anaemia
- Uterine anomalies, fibroids
Intrapartum
The main intrapartum factors for PPH include retained placenta, C-section and induction of labour. A list of intrapartum risk factors is shown below:
- C-Section (Emergency > Elective)
- Induction of Labour (IOL)
- Retained placenta
- Episiotomy
- Instrumental
- Prolonged labour
- > 4kg baby
- Pyrexia in labour
Aetiology
The aetiology of PPH can be remembered as the ‘four T’s’.
The four T’s include Tone, Trauma, Tissue and Thrombin and refer in particular to primary PPH:
- Tone (most common): reduction in uterine tone, typically the result of prolonged labour, macrosomia, twins, uterine anomalies or polyhydraminos. ‘Active’ management of the third stage reduces the risk.
- Trauma: usually due to episiotomy, extensive perineal tears or uterine rupture.
- Tissue: refers to retained placenta and placenta accreta.
- Thrombin: refers to either pre-existing or newly developed coagulopathies. Coagulopathies may also result from significant APH or PPH!
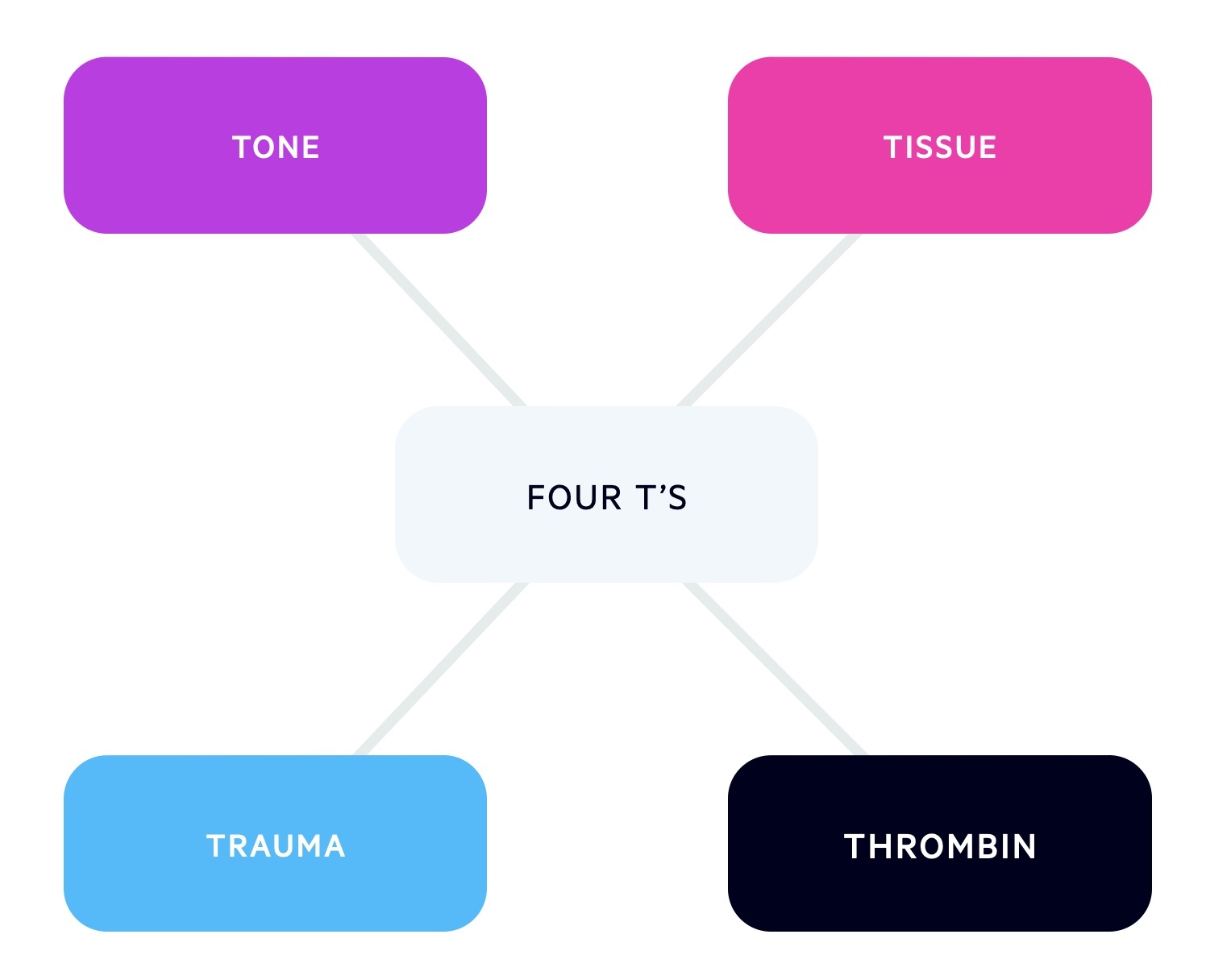
Secondary PPH most commonly occurs secondary to retained products of conception and endometritis.
Management
The management of PPH is critical because mother’s can lose a significant amount of blood and develop shock.
General management
- Observations
- Airway/breathing
- High flow oxygen
- Cardiovascular
- Two large-bore Intravenous access
- Bloods: FBC, Coag, U&S, LFTs, Crossmatch x4 units
- Fluid resuscitation
- Disability
- Examine: ?trauma ?atony.
- Exposure
- Amount of blood loss?
- Blood glucose level?
- Febrile?
- Catheter – monitor urine output
Specific management
The specific management of a PPH can be divided into interventions aimed to reduce the risk of developing a PPH or stopping a PPH.
Reduce risk:
- Anticipate those at higher risk:
- Deliver on a doctor-led unit
- Intravenous access
- Bloods: FBC, G&S, Crossmatch in labour
- “Active management of third stage”
- Intramuscular Oxytocin.
- Controlled cord traction (CCT) of placenta to aid delivery.
- Reduces PPH risk by up to 60%.
NOTE: synthetic oxytocin can be used to stimulate contraction of the uterus. Remember a ‘baggy’ atonic uterus is a cause of PPH.
Stopping PPH:
- Uterine massage: placing one hand on lower abdomen and performing repetitive massage and squeezing movements
- Bimanual compression: place one hand on the lower abdomen and one hand in the vagina. Push against the body of the uterus with the hand in the vagina, while the other hand compresses the fundus.
- Tranexamic Acid
- Massive Obstetric Haemorrhage Call
Obstetric haemorrhage protocol
In the event of a major postpartum haemorrhage, the major haemorrhage protocol should be activated throughout switchboard (2222).
Activation of the major haemorrhage protocol means you are alerting blood bank to the need for urgent blood products. A MOH call activates a team of obstetricians, midwives, anaesthetists, theatre, porters, blood bank and haematologists. Immediate access to O– blood can be found on the maternity unit but this is a limited resource.
Once the haemorrhage protocol is activated, a ‘runner’ needs to send an FBC, crossmatch and coagulation screen to blood bank. A blood pack is then sent back to the patient via the ‘runner’ with group-specific blood and fresh frozen plasma. Further products can be acquired following communication with the blood bank.
Obstetric haemorrhage team
- Obstetric team (SHO/Reg/Cons)
- Anaesthetic team (SHO/Reg/Cons)
- Midwifery team (case midwife/Coordinating midwife)
- Haematologist on call
- Haematology lab
- Porter
- Theatres
Fluid & blood products
- Crystalloid: up to 2L Hartmanns.
- Colloid: up to 1.5L until blood arrives.
- Blood: should be given when available, O-neg, group-specific or cross-matched depending on urgency.
- Fresh Frozen Plasma (FFP): 4 units FFP to every 4 units blood (PRC) or if clotting prolonged.
- Platelets: if Plt < 75 and bleeding ongoing.
- Cryoprecipitate: if Fibrinogen <2.
Pharmacotherapy
Uterine atony is the most common cause of PPH and uterotonic drugs are used to prevent it.
Uterotonic drugs
These medications work by increasing the force and frequency of smooth muscle contraction within the uterus.
- Syntocinon
- Oxytocin
- 5-10 iU IM/IV and 40 iU infusion.
- Ergometrine
- Ergot alkaloid
- 0.5mg IM/IV
- Avoid if HTN.
- Carboprost
- Prostaglandin PGF2α
- 0.25mg IM every 15mins, up to x8
- Avoid if asthma.
- Misoprostol
- Prostaglandin PGE1
- 800mcg PR or SL.
Surgical care
In the event that uterotonic medications are ineffective, or bleeding cannot be stopped, surgical intervention needs to be considered.
- Examination under anaesthesia (EUA): look for retained membranes/placenta.
- Repair tear
- Intrauterine balloon
- Brace suture (i.e. B-Lynch suture): compression suture used to mechanically compress an atonic uterus.
- Uterine artery embolization/ligation: liaise with the interventional radiology department.
- Hysterectomy: last resort if all other measures fail.
Secondary PPH
Secondary PPH is often associated with endometritis (endometrial infection) or retained products of conception (RPOC).
In cases of secondary PPH, it is important to assess for infection with high vaginal and endocervical swabs. Concurrently, an ultrasound scan should be completed looking for any RPOC or collections. Mothers may need antibiotics +/- surgical evacuation of retained products of conception (ERPC).

