The embryo enters the uterus 4 days after fertilisation and transitions from a morula to a blastocyst.
– It then undergoes hatching where the outer zona pellucida is removed allowing it to attach to the endometrium.
– It undergoes invasive interstitial implantation, where the cells of the blastocyst invade into the uterine lining.
– This invasion, and the merging of the syncitiotrophoblasts and endometrial cells allows the placenta to form.
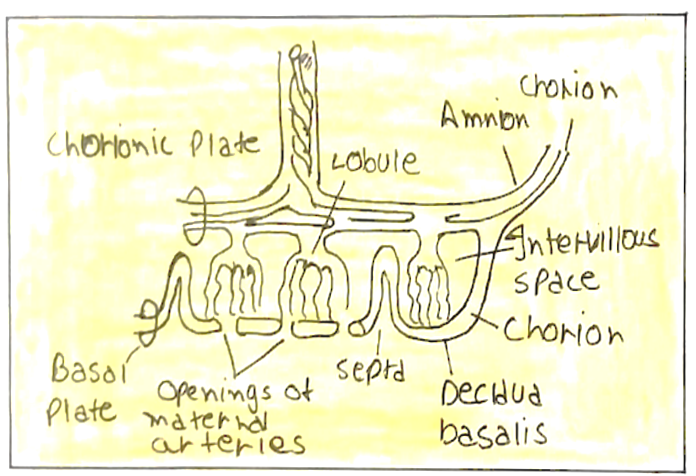
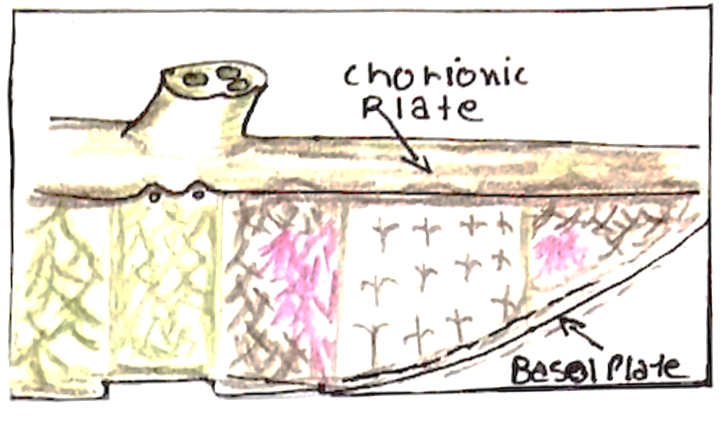
The placenta is a discoid organ which is composed of two plates:
i.) Chorionic plate –> faces the foetus and has the umbilical cord attached
ii.) Basal plate –> opposed to the decidua basalis and maternal blood enters through it
The placenta is formed in a number of steps, which are key to its role in achieving efficient nutrient exchange
i) Trophoblast differentiation:
The trophoblast (outer layer of blastocyst) differentiates into the:
– Syncitiotrophoblast (STB) –> outer multinucleated layer
– Cytotrophoblast (CTB) –> inner deeper layer
– The Syncitiotrophoblast is non-proliferative and is generated
by continual fusion of the Cytotrophoblast cells
ii) Erosion of decidua:
The Syncitiotrophoblast erodes into the decidua (endometrium)
– This breaks the endometrial glands and superficial capillaries
– Spaces appear within the STB and coalesce to form lacunae
– Glandular secretions and maternal blood fill the lacunae.
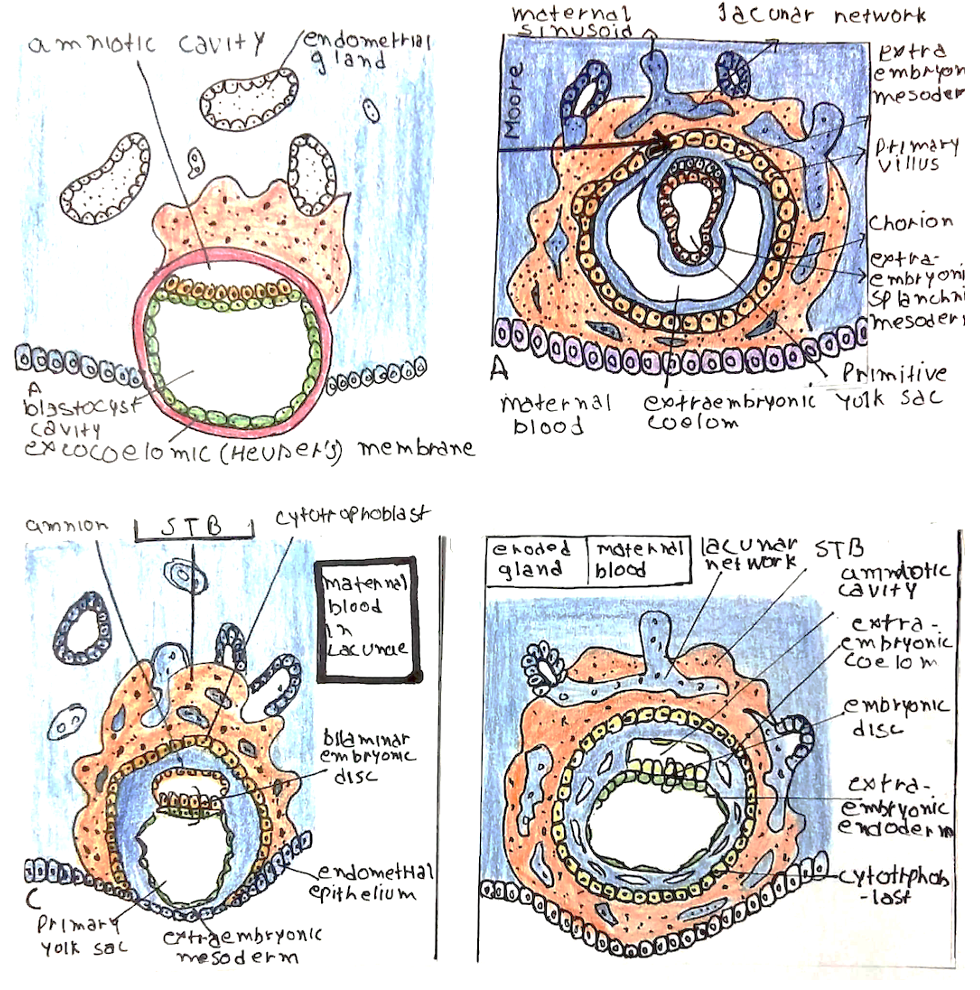
iii) Early villus formation:
Cytotrophoblast cells and extra-embryonic mesoderm from the embryo penetrate into the trabeculae of the Syncitiotrophoblast between the lacunae
– This forms the earliest placental villi
– A vascular network develops in the mesoderm
– This connects back to the foetus via the connecting stalk
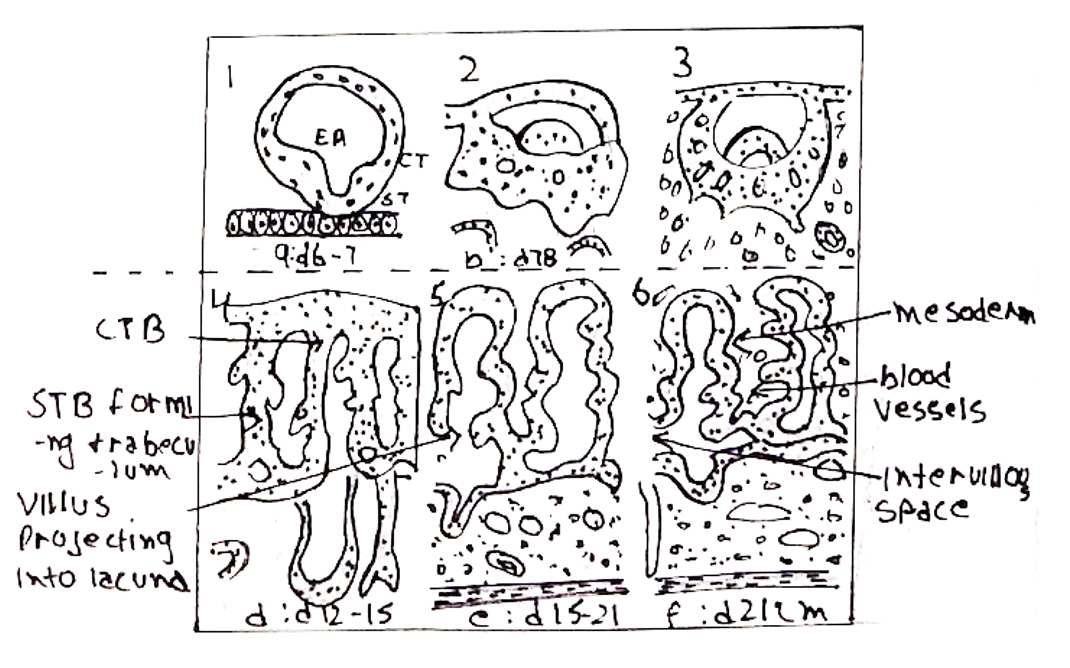
iv) Formation of villous tree:
Side branches extend from the early villi into the lacunae
– They gradually branch to become more complex
– Repeated branching forms the placental villous tree
– The lacunae are then referred to as the intervillous space
v) Regression of villi:
In early pregnancy, placental villi form over the entire chorionic sac
– Later however, the villi regress over the superficial pole to leave the discoid placenta. (i.e., they only remain in one pole, forming the placenta)
– The remainder of the sac forms the placental membranes (these rupture to a provide a route of exit at birth)

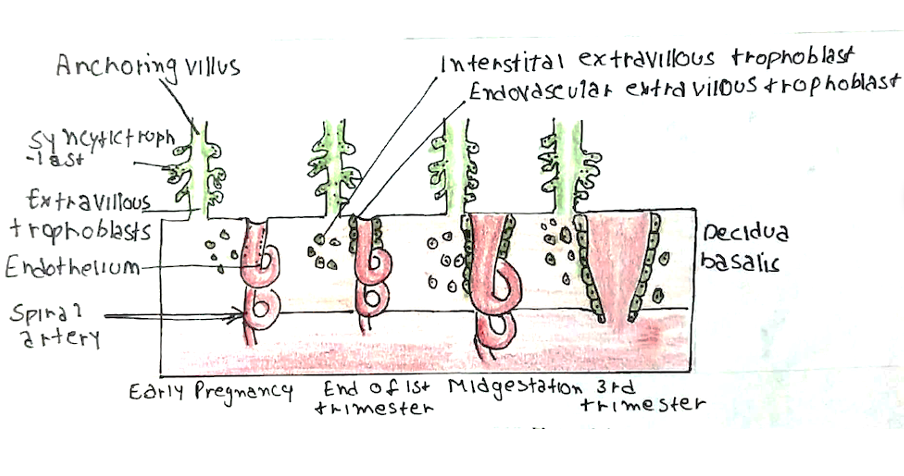
vi) Remodelling of circulation:
The general anatomical organisation of the placenta is achieved by 3-4 weeks
– However, it is not fully functional until maternal circulation has been remodelled which occurs by 10-12 weeks.
– CTB cells, known as extravillous trophoblasts (EVTs), invade the maternal spiral arteries which supply the endometrium
– The EVTs replace the endothelium of the arteries, resulting in vessel dilation and loss of vasoreactivity
– This results in blood flow to the intervillous spaces that is low pressure and low velocity
– Failure to convert the spiral arteries is associated with complications like growth restriction and pre-eclampsia
vii) Placental maturation:
By the 4th month, the placenta has two components:
– The decidua basalis (the maternal portion)
– The chorion frondosum (the foetal portion)
During the 4th and 5th months:
– The decidua form decidual septa
– These divide the placenta into compartments called cotyledons
– Cotyledons receive their blood supply through 80-100 spiral arteries
viii) Full-term placenta:
By the end of pregnancy, the placenta has a thickness of about 3cm,
diameter 15-25cm and weighs 500-600g.
– The foetal side is covered by chorionic plate
– The maternal side is covered by a thin layer of decidua basalis.
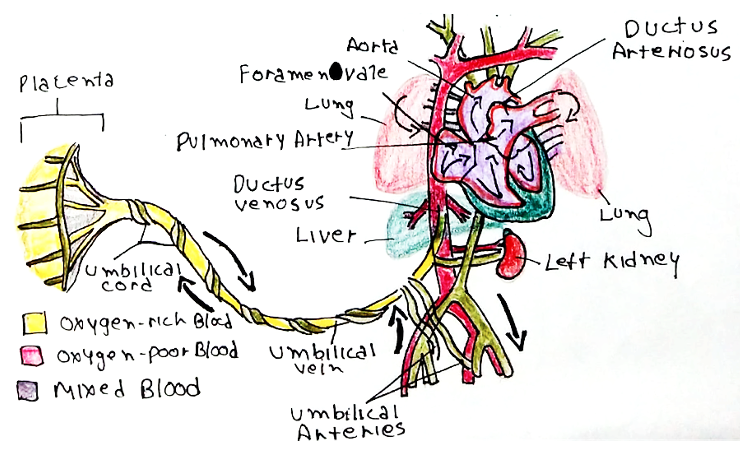
Umbilical cord
The umbilical cord is formed from the connecting stalk, which connects the blastocyst to the placenta.
– It is made of 3 blood vessels that carry foetal blood:
i) 2 umbilical arteries:
– These are branches from the internal iliac arteries
– Carry deoxygenated blood from the fetus to the placenta
ii) 1 umbilical vein:
– This joins the inferior vena cava via the ductus venosus
– Carries oxygenated blood from the placenta to the fetus
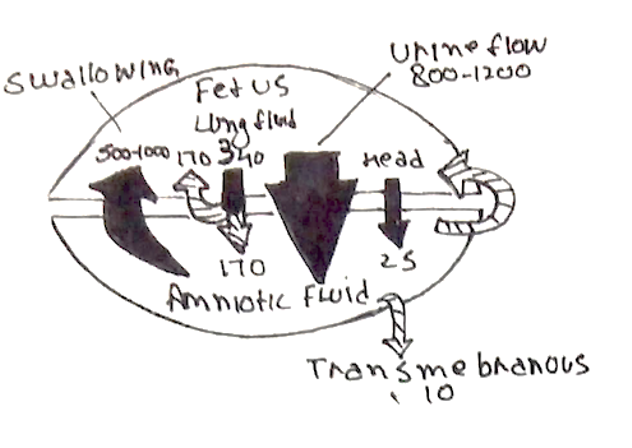
Amniotic fluid
This describes the protective fluid within the amniotic sac that cushions the fetus and serves as a transport medium for nutrients and metabolites.
– It is formed by maternal plasma diffusing through placenta and foetal urine
– It is around 850–1500 mL by the end of pregnancy
– The amniotic fluid is completely exchanged every 3 hours
– It is drained by the fetus (swallows fluid) + reabsorbed by umbilical cord into maternal circulation
– It contains proteins, glucose, urea, hair, dead skin, sebum and foetal urine