Placenta Accreta
This is a condition where the placenta attaches directly to the myometrium rather than the endometrium.
– This is a problem as it gives a very high risk of heavy bleeding at time of vaginal delivery.
There are 3 different types of placenta accreta depending on the degree of invasion:
i) Accreta –> Chorionic villi attach to the myometrium but will not invade into this layer
ii) Increta –> Chorionic villi invade into the myometrium, the muscular layer of the uterus
iii) Percreta –> Chorionic villi invade through the myometrium into the perimetrium
Risk factors:
Anything which damages the lining of the uterus (e.g., C-section)
Symptoms:
– Asymptomatic in pregnancy but gives risk of complications
– Post-partum haemorrhage (as placenta does not properly separate in labour)
– Risk of amniotic fluid embolism
– Potential damage to organs (bowel, bladder) from implantation and removal
Diagnosis:
– Ultrasound is the investigation of choice
– MRI can also be used to assess the depth of invasion
Management:
Caesarean section delivery, make precautions for PPH
– After this, it is likely that the woman will need a hysterectomy

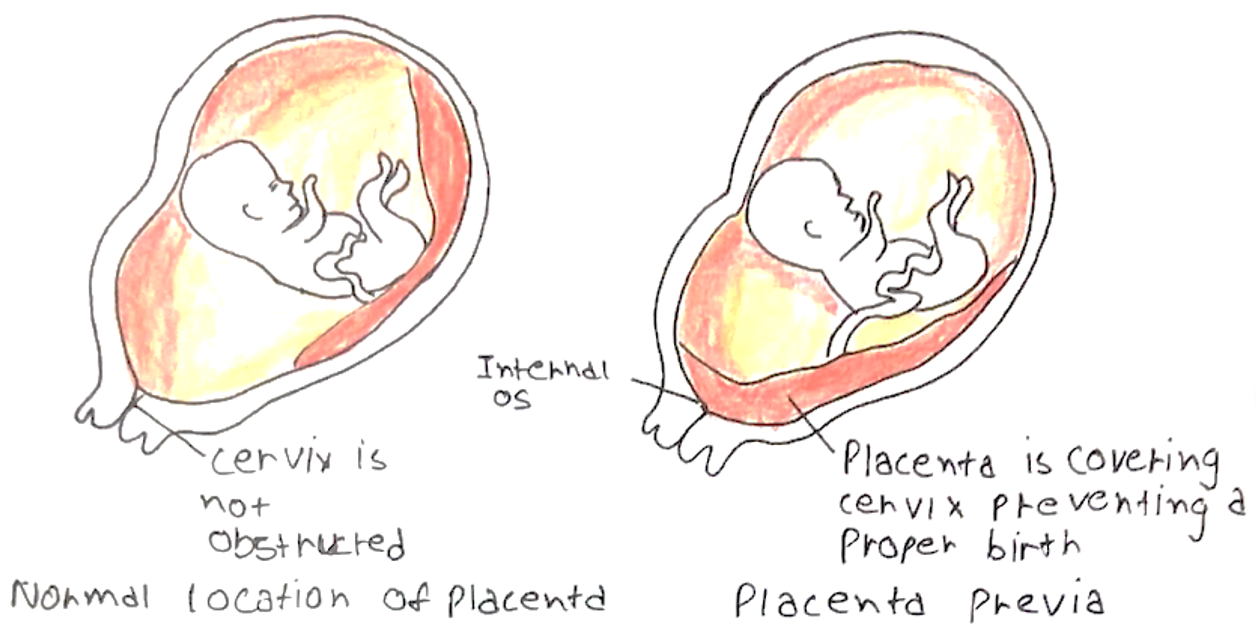
Placenta Praevia
This is a condition where the placenta occupies the lower uterine segment potentially covering the cervical os
– Its proximity to the cervical opening means that it is more susceptible to bleeding and haemorrhage
Placenta Praevia can be graded according to the extent by which it covers the internal os.
– Grade 1 –> Placenta occupies the lower segment but does not reach the internal os
– Grade 2 –> Placenta reaches the internal os but doesn’t cover it
– Grade 3 –> Before dilation the placenta covers the os, but not after dilation
– Grade 4 –> Placenta completely covers the internal os
Risk factors:
– Previous C-section, high parity, smoking, twins
Symptoms:
These are usually seen between week 24 and delivery
– Painless vaginal bleeding ranging from spotting or haemorrhage
– Hypovolaemic shock in proportion to visible loss (unlike abruption)
– Non-tender uterus
– Fetus –> Abnormal foetal lie and presentation, but foetal heart is normal
Diagnosis:
– Step 1 –> Foetal anomaly scan is used to assess placental location. If <20mm from internal os, go to step 2
– Step 2 –> Transvaginal ultrasound at 32 weeks is diagnostic
Management:
– If Grade 3/4 –> C-section delivery as normal vaginal delivery gives too high risk of PPH
Vasa Praevia
This is a condition which is similar to placenta praevia. However, rather than the placenta being near to the internal os, it is the foetal blood vessels that run close to the internal opening of the uterus
– These vessels may rupture when the membranes rupture at term, as they are unsupported by the umbilical cord or the placental tissue. This leads to vaginal bleeding which contains foetal blood.
Risk factors:
– Placenta praevia, IVF
Symptoms:
– Painless vaginal bleeding (similar to placenta praevia) after the membranes rupture
– However, the key is foetal distress –> bradycardia or death
Diagnosis:
– Ultrasound shows proximity of foetal vessels to internal os
– If unclear –> detection of foetal haemoglobin in vaginal bleeding is diagnostic
Management:
– Elective caesarean surgery is used to prevent risk of bleeding at delivery
Placental Abruption
This is a condition where part or all of the placenta prematurely separates from the uterine wall.
– It usually occurs at the start of the 3rd trimester and can lead to significant bleeding in the space between placenta and uterus, leading to both maternal and foetal compromise.
It is divided into two main types:
– Revealed –> blood tracks down from the site of placental separation and drains through the cervix
– Concealed –> bleeding remains within the uterus and typically forms a clot behind the placenta
Risk factors:
– Hypertension with proteinuria, Hypertension
– High maternal age, twins
– Cocaine use
Symptoms:
– Painful vaginal bleeding (Revealed)
– Signs of shock out of keeping with the volume of visible bleeding (concealed)
– Tender, woody uterus
– Can lead to severe maternal haemorrhage and DIC
– Fetus –> Normal lie and presentation, but foetal heart rate is abnormal
Diagnosis:
– Ultrasound is required to rule out placenta praevia
– It cannot rule out placental abruption due to the low negative predictive value
– It is a diagnosis of exclusion once the other conditions have been ruled out
Management:
– This is dependent on the gestational age and whether there is maternal/foetal compromise
– If maternal/foetal compromise (at any point) –> emergency delivery
– If no maternal/foetal compromise (before term) –> conservative management with monitoring
– If no maternal/foetal compromise (at term) –> Start induction of labour
Preterm prelabour rupture of membranes (PPROM)
This describes rupture of foetal membranes (chorion and amnion) occurring <37 weeks’ gestation
– They are strengthened by collagen and normally become weaker at term in preparation for labour
– When the membranes rupture, amniotic fluid is released which contains prostaglandins.
– This stimulates the uterine muscle to contract and so most women will go into labour within 24-48 hours
Risk factors:
– Previous pregnancies, invasive procedures (amniocentesis)
– Maternal factors –> smoking, cervical insufficiency, lower genital tract infection
– Foetal factors –> polyhydramnios, multiple foetuses
Symptoms:
– Classic ‘breaking of waters’ (painless popping sensation followed by gush of watery fluid from vagina)
– Change in colour/consistency of vaginal discharge
– Amniotic fluid pooling into the posterior vaginal fornix)
– Can lead to premature labour and chorioamnionitis
Diagnosis:
– 1st Perform a sterile speculum exam to look for amniotic fluid pooling:
– If pooling in seen –> no need for further diagnostic tests
– If no pooling seen –> need to sample the vaginal fluid
– 2nd is vaginal fluid sampling:
– Test for Insulin-like growth factor binding protein-1 (IGFBP-1)
– Test for Placenta alpha-microglobulin-1 (PAMG-1)
– If these are positive, confirms diagnosis of PPROM

Management
– Admit the patient to hospital and monitor regularly for chorioamnionitis
– Gives antibiotics
– Give antenatal corticosteroids –> reduces the risk of respiratory distress syndrome
– Consider induced delivery at 34 weeks’ gestation

