Post-partum Haemorrhage (PPH)
This is defined as blood loss of >500mls after delivery and it is divided into two subtypes:
Primary:
– This is blood loss which occurs within 24 hours of delivery:
– The causes can be remembered by thinking of the 4 T’s
Causes:
Tone (uterine atony most commonly)
Trauma (large baby)
Thrombus (clots)
Tissue (fibroids)
– In addition, it can be caused by abnormalities of the placenta (placenta previa/accrete)
Management:
– 1st line –> Apply bimanual compression (pressure aims to compress uterine arteries) with fundal massage
– 2nd line is medical management –> IV syntocinon (oxytocin) 10 units or IV ergometrine 500ug
– You can also use IM Carboprost (prostaglandin which aids uterine contraction)
If still bleeding take to operating theatre for surgical approaches.
– 1st line is Bakri balloon tamponade –> used if uterine atony is main cause
– If uncontrolled, B-lynch suture or uterine artery embolism
– If still not controlled –> ligate internal branch of the internal iliac artery
– Last resort is hysterectomy
Major Obstetrics Haemorrhage Protocol
Secondary:
– This is blood loss which occurs 24 hours – 12 weeks after delivery
– It is usually due to placental tissue remaining in the uterus or infection of the uterus (endometritis)
Management:
– Treating the underling condition
Perineal tears
This is a laceration/tear of the skin and soft tissues which separate the vagina from the anus.
– As the child is expelled out of the vagina, the pressure causes the skin and tissue to tear away
– It is the most common form of injury caused by childbirth and is seen in varying severity.
Risk factors:
– Macrosomia (large baby) causes increased pressure on the tissues
– Instruments used in delivery e.g., forceps
– Delivery complications –> shoulder dystocia, cord prolapse
Types:
These are graded by the extent and depth of underlying structures affected
1 –> This is where there is only damage to the skin and subcutaneous tissue, but no muscle
2 –> This includes injury to the pelvic floor muscles but does not involve any of the anal sphincters
3a –> There is a <50% thickness tear of the external anal sphincter
3b –> There is a >50% tear of the external anal sphincter
3c –> The tear extends to the internal anal sphincter
4 –> Injury to both sphincters and the mucosa of the rectum

Management:
– 1st degree tears do not require treatment and heal spontaneously
– Grade 2 tears can be repaired under local anaesthetic with sutures
– If there is involvement of the sphincters (grade 3 and above), this will require surgical management
Cord Prolapse
This is when the umbilical cord comes out of the uterus before the presenting part of the fetus.
– This can lead to cord compression, as the fetus compresses cord occluding blood flow to fetus
– Exposure to cold can also cause cord arterial spasm, reducing flow to fetus giving hypoxia
Risk factors
– Artificial rupture of the membranes (most common cause), long umbilical cord
– Associated with polyhydramnios and abnormal lies and presentations of the fetus

Symptoms
– Cord is palpable vaginally or visible out of the vagina
– Foetal distress –> bradycardia, late decelerations on CTG
Management:
The definitive management in an emergency C-section
– In the meantime, however, procedures are used to reduce pressure on the cord:
– Pushing the head of the fetus back into the vagina
– Elevating the presenting part of the fetus
– Put mother in knee-chest position to relieve pressure on cord
– You can also use tocolytics (terbutaline) to pause uterine contractions
Shoulder Dystocia
This is a complication of vaginal delivery where there is inability to deliver the body of the fetus after the head is delivered out of the vagina.
– In normal labour, the foetal head is delivered first via extension out of the pelvic outlet
– This is followed by rotation of the fetus so that the foetal shoulders now lie in an anterior-posterior position
– Shoulder dystocia occurs when there is either impaction of the anterior foetal shoulder behind the maternal pubic symphysis (more common) or posterior shoulder on the sacral promontory (less common)
– This delay in delivery can lead to complications for the fetus including hypoxia
– In addition, applying excessive force can result in damage to foetal tissues and nerves (brachial plexus)
Risk factors:
Macrosomia
Induction of labour
Gestational diabetes
Symptoms:
– Failure of restitution (the foetal head remains in the occipital anterior position after delivery whereas the body remains in the vaginal canal)
– Turtle neck sign (the foetal head retracts slightly back into the pelvis)

Complications:
– Foetus –> Hypoxia, brachial plexus injury or humerus fractures
– Mother –> Perineal tears, risk of postpartum haemorrhage
Management:
– This involves performing manoeuvres to aid delivery
– 1st line is McRoberts’ manoeuvre
–> Flex and abduct the maternal hips, bringing thighs towards abdomen and apply suprapubic pressure
–> This helps to angle the shoulders out of the pelvis by increasing the anterior-posterior diameter
– If fails, there are other manoeuvres possible like the Rubin II or woodscrew manoeuvre
– If the baby still cannot be delivered, you can push the baby’s head back (Zavanelli’s manoeuvre) followed by an emergency caesarean section to immediately delivery the baby.
Uterine Rupture
This describes a full thickness disruption of the uterine muscle during pregnancy and childbirth
– It most commonly occurs during labour, due to the pressure caused on the wall as the woman tries to deliver the baby. However, it can occur anytime during the third trimester too.
– Divided into incomplete (peritoneum over uterus intact) and complete (peritoneum also torn allowing uterine contents into the peritoneal cavity)
Risk factors:
Previous uterine surgery (C-section, fibroids)
Macrosomia
Induction of labour
Symptoms:
– This gives non-specific symptoms of shock and abdominal pain
– Sudden abdominal pain which persists in-between the contractions, with a feeling that something “gave-way”
– Vaginal bleeding
– Maternal shock –> tachycardia, hypotension
– Foetal distress –> late decelerations on CTG, absent foetal heart sounds
Tests:
– Ultrasound
– CTG shows changes in foetal heart rate, prolonged foetal bradycardia, late decelerations
Management:
– Emergency C-section and uterine repair/hysterectomy
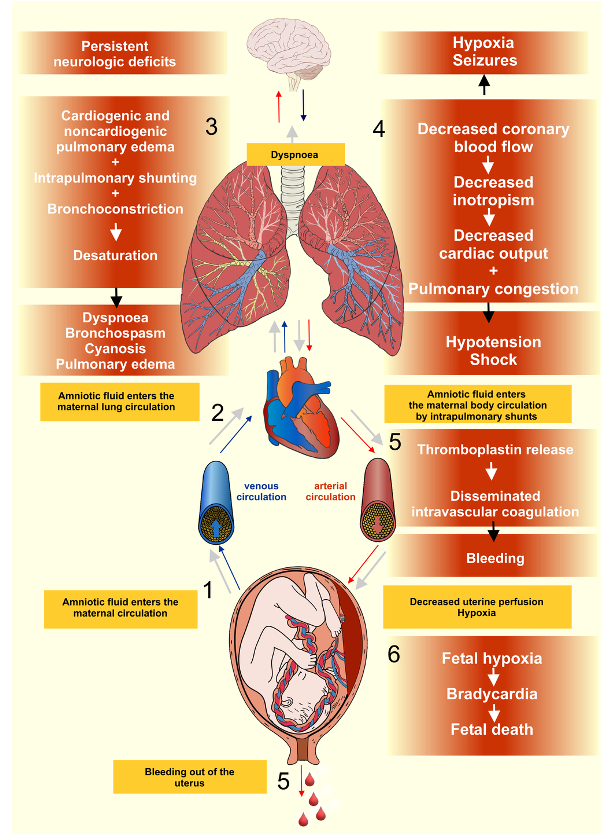
Amniotic fluid embolism
This is an obstetric emergency in which amniotic fluid enters the blood stream of the mother
– The embolism travels to the lungs where foetal cells the amniotic fluid react with maternal blood cells triggering a hyper-immune reaction
– This results in cardiorespiratory collapse (heart and lung) and disseminated intravascular coagulation
– Most cases occur during labour, but they can also occur during a C-section or immediately after birth
Symptoms:
– This gives signs of cardiorespiratory collapse and DIC
– DIC –> Profuse bleeding
– Respiratory collapse –> Tachypnoea, shortness of breath, cyanosis
– Cardiovascular collapse –> Tachycardia, hypotension, loss of consciousness
Diagnosis:
It is a clinical diagnosis of exclusion
Management:
Supportive ABCDE management in intensive care unit

