Labour can be defined as the onset of regular and painful contractions associated with cervical dilation and descent of the presenting part.
– It involves shedding of the cervical mucus plug, rupture of the amniotic sac and uterine contractions.
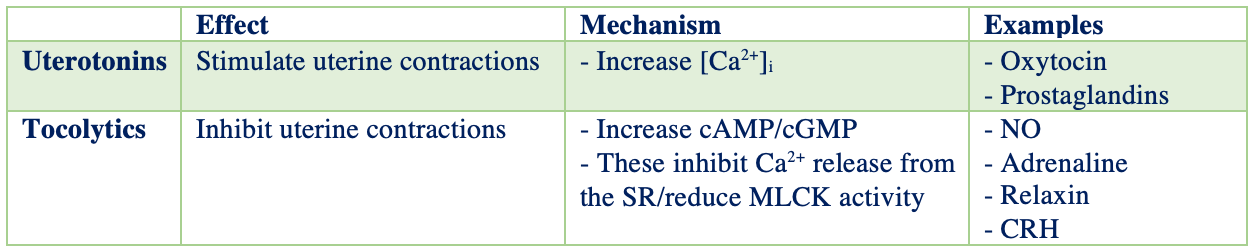
The shortening of the uterine myocytes causing Braxton-Hicks contractions is key to labour:
– [Ca2+]i increases by influx through Ca2+ channels and by release from the SR
– Ca2+ activates calmodulin (CAM) –> calmodulin activates myosin light chain kinase (MLCK)
– MLCK generates ATP for contraction of the filaments
Labour is divided into 3 stages:
Stage 1:
This describes the time from the onset of true labour to when the cervix if fully dilated
– Uterine contractions begin, pulling on thick tissues of cervix causing it to thin and dilate
– The cervix eventually dilates to 10cm allowing the fetus’ head to enter the birth canal
– Latent phase is 0-3cm cervical dilation
– Active phase is 3-10cm dilation
– Primigravida woman will take 10-16 hours
– Multigravida woman much shorter time
Stage 2
This describes the time from full cervical dilation to the delivery of the fetus, can last 1 hour
– Foetal head enters the pelvic inlet with the sagittal suture in the transverse plane
– Foetus rotates so that, at the pelvic outlet, the sagittal suture is in the ant-post plane
– Foetus rotates again by 90º as the shoulders are delivered
N.B. The ease of stage 2 labour depends a lot on the fetus and its anatomy:
– Size –> Large foetuses have more difficulty passing through the birth canal
– Presentation –> Cephalic (headfirst) presentation is ideal
– Attitude –> This refers to how the fetus is flexed.
Usually fetus is fully flexed (chin on chest)

Stage 3
This is the time from the delivery of the fetus to when placenta and membranes are delivered
– After the fetus is delivered, the uterus begins to contract down in size
– Uterine muscle fibres contract to compress the blood vessels formerly supplying the placenta, which shears away from the uterine wall (15mins) – it is normal to lose 500ml of blood.
– This stage is characterised by irregular contraction of low intensity, which forces the placenta out the vagina
Monitoring During Labour
Whilst the majority of labour in the world occurs naturally, there are times when humans must intervene:
Induction of Labour (IOL)
This describes a process where labour is started artificially to stimulate birth of the fetus
– The Bishop score is used prior to induction and uses to see how likely labour will progress naturally.
– If the Bishop Score <5, this suggests that the woman will require induction
Indications:
– Prolonged pregnancy, e.g., between 40+0 and 40+14 weeks
– Premature rupture of the membranes, where labour does not start
– Maternal health problems (hypertension, pre-eclampsia, diabetes >38 weeks)
– Rhesus incompatibility
Contraindications:
– These are generally the same as for vaginal delivery (hence requires a Caesarean)
– Cephalopelvic disproportion
– Vasa Previa
– Transverse lie
– Previous classical C-section
Methods:
– There are 3 main methods of induction:
i) Membrane sweep:
– Insert finger through cervix and rotating against foetal membranes
– It separates the chorionic membrane from the decidua releasing prostaglandins
– Offered at 40-41 weeks for 1st time mothers, and 41 weeks for multiparous women
ii) Vaginal Prostaglandins:
– These are used to ripen the cervix and stimulate uterine smooth muscle
iii) Amniotomy:
– This is where membranes are artificially ruptured releasing prostaglandins
– Only performed when cervix has been deemed ripe and given with Oxytocin
Instrumental Delivery
This describes a process where the baby is delivered using man-made instruments
– The decision to perform instrument delivery is based on the clinical scenario in the 2nd stage of labour.
– This includes foetal or maternal distress, or failure to progress during 2nd stage of labour
Contraindications:
– Incompletely dilated cervix, breech presentation, unengaged foetal head
Methods:
i) Ventouse:
– This attaches a cup to the foetal head via a vacuum.
ii) Forceps:
– These are inserted into the vagina and placed around a baby’s head
– Forceps have a lower risk of foetal complications compared to the ventouse but higher risk of maternal complications
Caesarean Section
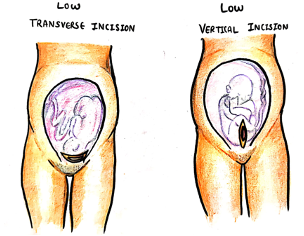
This is a surgery where an incision is made through the uterus and the baby is taken out
– Used if there is failure to progress or if there foetal/maternal compromise during labour
– Two main types of incision are lower segment caesarean (now 99% of cases) and the classic caesarean (longitudinal incision in upper segment of uterus)
Categories:
C-sections are classified based on their urgency:
1 – immediate threat to the life of woman or fetus
2 – maternal or foetal compromise not immediately life-threatening
3 – no maternal or foetal compromise but needs early delivery
4 – elective (delivery timed to suit the woman/other factors)
Complications:
– Fetus –> lacerations
– Mother –> emergency hysterectomy, damage to bladder or ureters
– Future pregnancies –> increased risk of uterine rupture, stillbirth, placenta previa and accreta
N.B. Most obstetricians recommend normal labour in women who have had a previous C-section
– However, women should have C-section if they had previous uterine rupture or a classical C-section scar

