Pregnancy-induced hypertension
This is defined as having a raised blood pressure which occurs after the 20th week of pregnancy without proteinuria.
– If a woman has hypertension before, then this is counted as pre-existing hypertension. Whereas, if she develops other symptoms like proteinuria and oedema, this points to a diagnosis of pre-eclampsia
– Gestational hypertension resolves after birth, but women have higher risk of pre-eclampsia in the next pregnancy
– The major risk to watch out for is progression to pre-eclampsia (High BP with proteinuria)
The hypertension is defined as two separate readings confirming either:
– Systolic >140mmHg or diastolic >90mmHg
– Or Increase above booking readings of >30mmHg systolic or >15mmHg diastolic
Tests:
These are done to monitor the blood pressure and check for progression to pre-eclampsia:
– Urine dipstick + 24hr urine collection
– Blood tests –> FBC, LFTs, U&Es
Management:
– Antihypertensive medication –> 1st line is labetalol, 2nd line nifedipine, 3rd methyldopa
– Maternal monitoring –> Monitor BP weekly (aim for <135/85) and monitor urine dipstick for proteinuria
– Foetal monitoring –> Foetal heart auscultation at every antenatal appointment + US from 28 weeks
Pre-eclampsia
This is a condition in pregnancy which is characterised by pregnancy induced hypertension with proteinuria
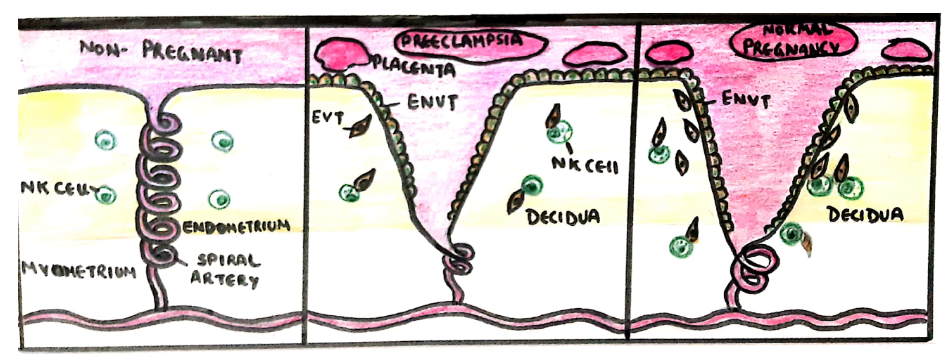
– In normal placentation, trophoblast cells invade the spiral arteries of the uterus
– Remodelling occurs resulting in spiral arteries that are dilated giving high flow, low resistance circulation
– In pre-eclampsia, there is poor remodelling of the spiral arteries giving low-flow and high-resistance
– The increase in blood pressure leads to a systemic inflammatory response and endothelial cell dysfunction
Risk Factors
Symptoms:
– Can be asymptomatic
– Headache with visual disturbances
– Papilledema
– Sudden onset non-dependent oedema
– Hyperreflexia
– RUQ/epigastric pain (due to hepatic capsule distension/infarction)
– Can lead to HELLP syndrome
Complications:
– Mother –> Eclampsia (seizures), HELLP syndrome and uncontrolled hypertension
– Fetus –> Prematurity, intrauterine growth restriction, placental abruption
Tests:
– BP measurement and urine dipstick with 24hr collection
– FBC –> may show low Hb, low platelets (progression to HELLP syndrome)
– U&Es –> elevated urea and creatinine (different ranges from normal population as plasma is diluted)
– LFTs –> elevated ALT and AST (used to assess for HELLP syndrome)
Diagnosis:
– For a diagnosis of pre-eclampsia, three criteria should be met:
i) Gestation >20 weeks
ii) Hypertension: systolic >140 or diastolic >90 on two occasions 4 hour apart
iii) Proteinuria: Protein: creatinine ratio >30mg/mmol
Grading Pre-eclampsia
Management:
– It is important monitor maternal BP and urine and fetus regularly
– Antihypertensive medication –> 1st line is labetalol, then nifedipine or hydralazine
– Delivery of baby –> This is the only definitive cure for pre-eclampsia
– Induce delivery by latest 37-37 weeks (or 34 weeks if severe symptoms)
– Must monitor post-delivery as mother has highest risk of seizures 24hrs post-partum
Before the baby can be delivered, you will need to stabalise the mother before she goes into labour
– This is because unstable mothers who develop eclampsia will require general anaesthetic to terminate seizures
– This gives a significant risk of rebound hypertension
– It also increases the risk of haemorrhagic stroke and makes intubation very difficult
Therefore, activate severe pre-eclamptic protocol –> 1st give oral labetalol, 2nd line is IV infusion
– Also give magnesium sulphate (prevents development of seizures).
– Then you should deliver the baby
Prevention:
– To mitigate the risk of pre-eclampsia, give prophylaxis if 1 high risk or 2+ moderate factors:
– Give aspirin 75mg/day from 12 weeks to 36 weeks
Eclampsia
This is the development of seizures in association with pre-eclampsia.
– It occurs due to the failure of cerebral autoregulation leading to seizures and haemorrhagic stroke.
– The biggest complication is AKI which leads to pulmonary oedema (leading cause of eclampsia death)
– It can occur any time after the 20th week of pregnancy but the highest risk if 24 hours post delivery
Symptoms:
– Background of Pre-eclampsia –> Pregnancy induced hypertension and proteinuria
– Failure of cerebral autoregulation –> seizures and haemorrhagic stroke
Management:
This involves stabilising the mother followed by immediate delivery of the fetus (if not yet born)
– Give magnesium sulphate (used to prevent and treat seizures)
– Mother is given an IV bolus, followed by a continuous infusion
– This infusion is continued for 24 hours after last seizure or delivery (whichever is later)
– It can lead to respiratory depression, but this can be reversed with calcium gluconate
– Fluid restrict to prevent pulmonary oedema
– One mother is stabilised, attempt delivery (continue magnesium sulphate infusion for 24 hours after)
HELLP syndrome
This is a condition which stands for Haemolysis, Elevated Liver enzymes and Low Platelet count.
– It shares features with pre-eclampsia but is separate condition
– Pre-eclampsia is a risk factor for the development of HELLP syndrome, which is an obstetric emergency
Risk factors:
– Pre-eclampsia/eclampsia
– Mother >25 ages
– Previous history
– Being Caucasian
Symptoms:
– Haemolysis –> gives low Hb and lethargy
– Elevated liver enzymes –> Gives raised LFTs, RUQ pain and nausea/vomiting
– Low platelet count –> Bleeding (e.g. haematuria)
– Can lead to DIC, placental abruption and kidney failure
Diagnosis:
– Blood tests –> Shows high LFTs, low platelet, low Hb, raised LDH and bilirubin
– Blood smear –> Shows schistocytes
Management:
Delivery of the baby as soon as possible

