In the uterus, there are 3 variables that we monitor concerning the baby’s position.
Lie:
– This is the relationship between the long axis of the fetus and that of the mother
– It can be longitudinal, transverse or oblique
Presentation:
– This describes the part of the fetus that first enters the maternal pelvis
– Can be cephalic vertex (headfirst), breech, shoulder, face and brow
Position:
– This describes the position of the foetal head as it exits the birth canal
– Can be occipito-anterior (ideal), occipito-posterior or occipito-transverse
Abnormal lies, presentations and positions all increase the chances of complications during delivery:
Breech Presentation
This is a situation when the caudal end of the fetus is the first part to enter the maternal pelvis.
– This is problematic as it can lead to complications for both the fetus and the mother during delivery.
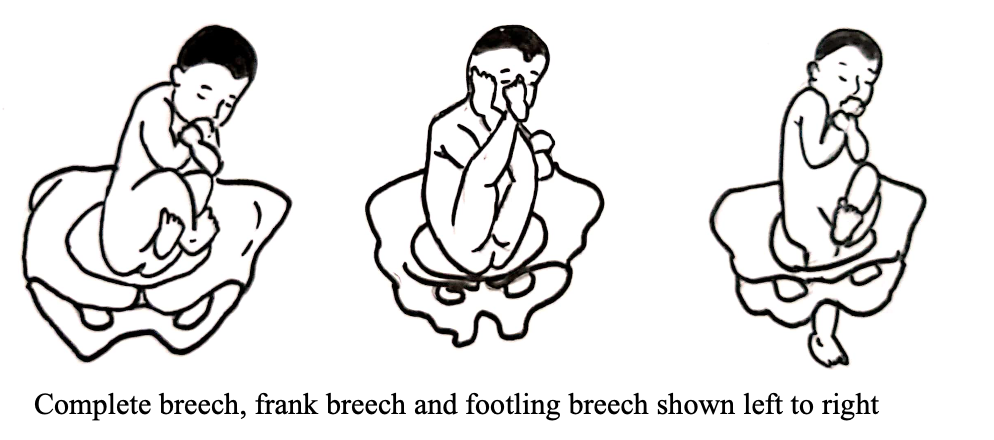
It is split into 3 types:
– Frank –> this is the most common where buttocks occupy the lower segment
– Complete –> this is where the complete caudal end of the fetus is in the lower segment
– Footling –> this is the most dangerous form where the foot is in the pelvis
Risk factors
– Mother –> Malformations of the uterus, large fibroids, previous uterine surgery
– Pregnancy –> Placenta Praevia, poly/oligohydramnios, prematurity
Complications:
– Higher rate of cord prolapse, PPROM and birth asphyxia
– Entrapment of the foetal head, intracranial haemorrhage
Diagnosis:
– Ultrasound is the investigation of choice
Management:
If <36 weeks:
– No action is required yet as many foetuses will turn spontaneously to cephalic presentation
If >36 weeks:
– 1st line is external cephalic version (ECV) to turn baby into cephalic presentation
– It is offered at 36 weeks for 1st time mothers and 37 weeks for multiparous women
– However, this cannot be offered if there are multiple pregnancies or ruptured membranes
– In addition, do not perform is worry about the fetus with abnormal CTG
If unsuccessful:
– Offer elective Caesarean section or vaginal breech delivery
– In reality most mothers nowadays will opt for an elective caesarean section rather than attempt a vaginal breech delivery
Transverse Lie
This describes a fetus whose long axis lies transversely across the mother’s lower abdomen
– It increases the risk of premature rupture of membranes and cord prolapse
Management:
C-section if baby is transverse at term

Foetal Size/position abnormalities
It is important to monitor the size of the baby, as both small and large babies are associated with complications
– Babies are measured during the antenatal scans using ultrasound, which measures certain variables
– These include abdominal and head circumference and femur length to calculate estimated foetal weight (EFW)
– In addition, you can use Doppler ultrasound to measure the flow through the vessels like the umbilical artery
– The EFW is plotted on a growth chart to see the trend and assess if the baby is following a steady trajectory.
Small for gestational age (SGA)
This term is used to describe a fetus/infant which is exceptionally small for its age compared to the average
– Infant SGA –> this is an infant born with a weight < 10th centile
– Foetal SGA –> fetus with estimated foetal weight (EFW) or abdominal circumference (AC) < 10th centile

It is helpful to divide SGA babies into 2 subtypes, as the management is very different:
Constitutionally small:
These infants are small without a pathological reason
– This is usually due to inherited genes and characteristics from the parents
– Therefore, their size is what is expected of them
Growth restriction:
This is a term which is used to describe pathological restriction of the genetic growth potential, and so it is called pathological SGA
– Foetal or maternal features stop the fetus achieving its genetic growth potential
– It is this subtype which has higher risk of postnatal complications
Causes:
– The causes can be divided into maternal and foetal factors:
Maternal:
– Maternal anaemia, under-nutrition (gives poor diffusion of substances across placenta)
– Pre-eclampsia, hypertension, diabetes, maternal substance abuse (reduced blood flow to the placenta)
Fetus:
– Chromosomal abnormalities, infection, errors of metabolism, genetic disorders
Types:
i) Asymmetrical:
– This is a type of restriction where the head grows normally out of proportion of the body
– It is usually seen when baby grows normally in first 2 trimesters and then has problems in the third
– This leads to a compensatory mechanism to preserve flow and nutrients to the brain at the expense of other less important tissues
– This is usually due to maternal (placental) factors that’s affects the baby at later gestational ages
ii) Symmetrical:
– This is called global growth restriction and it where the baby is small proportionately
– This will occur if the baby is affected at a very early stage and so has always developed slowly
– These babies are more likely to have permanent neurological damage
– This is usually due to foetal factors (infections, genetic disorders) but also chronic maternal issues (long term anaemia, or substance abuse)
Management:
All women are assessed at booking and again at 20 weeks for risk factors for SGA
– If high risk factors for SGA –> Serially assess foetal size and umbilical artery Doppler from weeks 26-28
– If SGA detected –> Serially assess of foetal size and umbilical artery Doppler every 2 weeks
– If the baby continues to be small, it is likely that they will be delivered early by C-section
Large for Gestational Age (LGA)
This term is used to describe a fetus which is exceptionally large for its age compared to the average
– Infant LGA –> this is an infant born with a weight > 90th centile
– Foetal LGA –> fetus with estimated foetal weight (EFW) or abdominal circumference (AC) > 90th centile
Causes:
– Maternal diabetes (Type 1 or gestational)
– Genetics –> Beckwith-Wiedemann syndrome
Complications:
The main problem is that it leads to increased problems during delivery
– Birth trauma (especially shoulder dystocia)
– Polyhydramnios
Management:
Monitor growth, if very large maybe induced early or opt for elective caesarean section

