Bleeding in the first trimester of pregnancy is not an uncommon event but is a source of anxiety for mothers.
– The reasons for this can range from idiopathic to serious conditions like an ectopic pregnancy.
– In addition, it can also be due to gynaecological conditions like ectropion, trauma and polyps
If a woman has bleeding in the first trimester, management depends on the gestational age and her symptoms:
If <6 weeks gestation:
– Expectant management. Advise woman to repeat pregnancy test after 7-10 days
– If this is positive then return to the clinic
– If the test is negative this means that the woman has miscarried
If >6 weeks gestation or any pain/tenderness:
– Immediate referral for assessment for ultrasound scan
At assessment, it is likely that the woman will have her blood tests taken for b-hCG and an ultrasound scan
– The scan may reveal various things like an ectopic, miscarriage or a healthy viable pregnancy
Pregnancy of Unknown Location
If scan is inconclusive however, this is known as a pregnancy of unknown location.
– In this case, take 2 serum hCG measurements 48 hours apart.
If hCG decreases >50%:
– It is most likely is that pregnancy will miscarriage.
– Therefore, take urine pregnancy test after 14 days which will most likely come back negative
– If still positive, she needs review in assessment unit again
If hCG increases >63%:
– Most likely is that this is a healthy intrauterine viable pregnancy
– Therefore, offer transvaginal ultrasound between 7-14 days later
If hCG change is between <50% and >63%:
– This suggests could be due to ectopic pregnancy
– Therefore, refer to early pregnancy assessment service within 24 hours and repeat ultrasound scan
Miscarriage
This is a term used to describe expulsion of the products of conception before 24 weeks gestational age
– About 1/5 of diagnosed pregnancies will result in miscarriage in the early stages
– It should be suspected if there is a positive urine pregnancy test and bleeding in first trimester
Cause:
– During first trimester, usual cause is chromosomal abnormality (most common is trisomy 16)
– During second trimester, most common cause is an incompetent cervix (risk from cervical surgery)
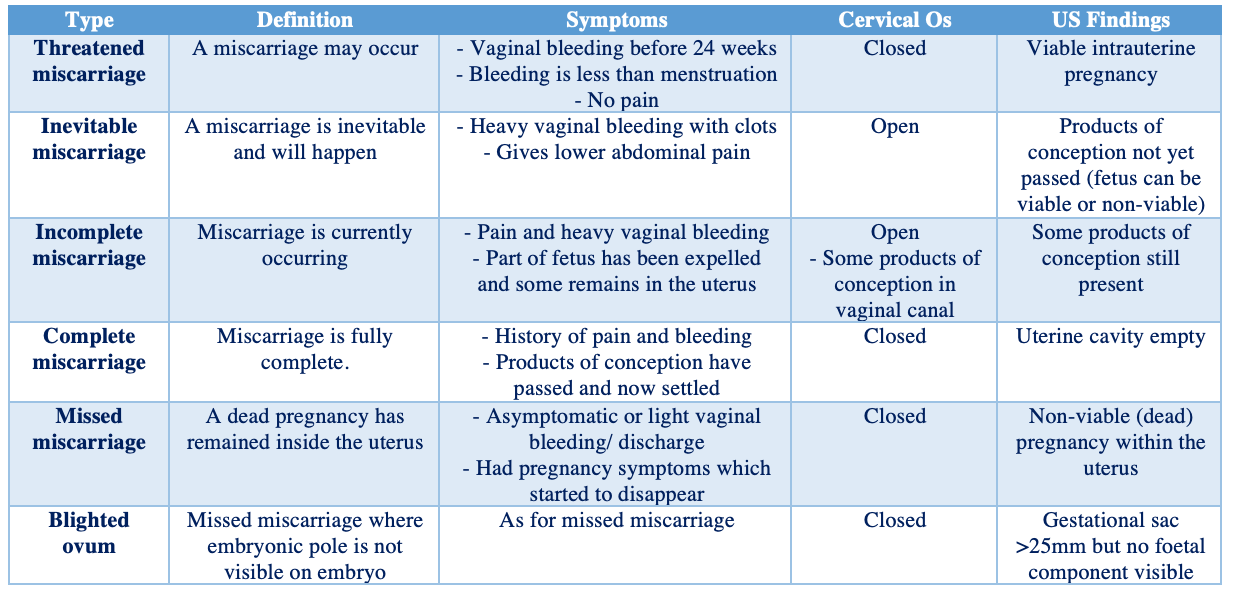
Miscarriage can be divided into several types:
Diagnosis:
Transvaginal ultrasound is used:
– If no heartbeat seen but there is a visible foetal pole, use the crown rump length (CRL) to estimate gestation:
– At a CRL of 7mm, you should normally be able to detect heartbeat.
– If CRL <7mm –> cannot diagnose miscarriage at this stage so repeat scan after 1 week, then diagnose
– If CRL >7mm and no heart rate –> suggests that miscarriage has occurred
If no heartbeat seen and no visible foetal pole, you can measure the gestational mean sac diameter (MSD):
– If MSD <25mm –> can’t diagnose miscarriage at this stage so repeat scan after 1 week, then diagnose
– If MSD >25mm –> diagnose miscarriag
Management:
This depends on the type of miscarriage:
i)Threatened:
– If heavy bleeding admit to hospital and observe
– If light reassure and refer back to midwife
– Take blood test for hCG (48 hours apart) to check status of the baby
ii) Inevitable, incomplete or missed:
– 1st line is expectant (watch and wait for 1-2 weeks)
– If infection, risk of haemorrhage or previous miscarriage, then do medical or surgical management
– Medical = Vaginal misoprostol (acts to contract and dilate cervix to expel the fetus)
– Surgical = Manual vacuum aspiration or surgical management in operating theatre
iii) Complete:
– Discharge to GP as the miscarriage has already occurred
N.B. You must give anti-D prophylaxis to women presenting at any stage of miscarriage who are:
– Rhesus negative with pregnancy >12 weeks or a pregnancy that is managed surgically
Recurrent miscarriage
This is the occurrence of 3 or more consecutive pregnancies that end in miscarriage of the fetus before 24 weeks
– This requires prompt investigation to search for an underlying cause. This can be split into 3 types of investigations used to detect chromosomal abnormalities, blood problems, and anatomical causes.
Investigations:
Blood tests:
– Thrombophilia screen
– Antiphospholipid antibodies (lupus anticoagulant, anticardiolipin/anti-B2 glycoprotein)
– Hormonal Profile
– Blood glucose tests
– Thyroid function tests
Imaging:
– Pelvic Ultrasound used to detect any structural abnormalities
Karyotyping:
– This is used to determine whether there are any chromosomal abnormalities:
Cytogenic analysis:
– This can be performed on the products of conception (POC)
Parental peripheral blood karyotyping:
– This can be performed when analysis of the POC shows an unbalanced structural chromosomal abnormality
Management:
– This involves managing the underlying condition
– If the underlying condition is irreversible, consider IVF or adoption
– Ensure that you also give psychological support to the couple

