Endometrial Cancer
A uterine cancer usually seen in post-menopausal women, in 2 types:
i) Uterine sarcoma:
A malignant proliferation of muscles of the uterus
ii) Adenocarcinoma:
A malignant proliferation of the endometrial glands
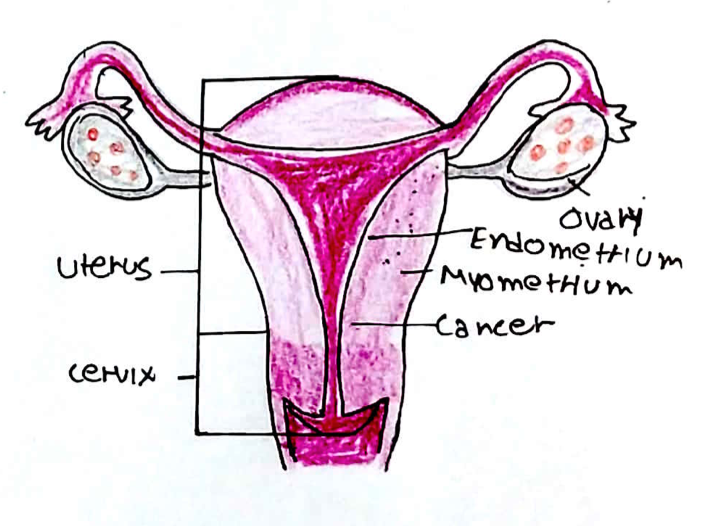
It is the most common invasive carcinoma of the female genital tract which is further divided into two subtypes:
Type 1:
– This is called an endometroid carcinoma where the tumours look like normal endometrial glands
– Associated with high oestrogen levels and often preceded by endometrial hyperplasia
Type 2:
– This has multiple subtypes, is a rarer and not linked to oestrogen exposure
Full adenocarcinoma is usually preceded by hyperplasia of the glands, which occurs due to oestrogen.
– Oestrogen stimulates endometrial growth whereas progesterone stimulates shedding of this tissue
– The hyperplasia of the glands is subdivided into two types, one which is more dangerous:
i) Endometrial hyperplasia without atypia –> low risk of progression to cancer
ii) Endometrial hyperplasia with atypia –> abnormal cell with higher risk of progression to cancer
Risk factors:
– Most are related to unopposed oestrogen exposure
– Early menarche + late menopause
– Obesity
– Infertility with anovulatory cycles
– Nulliparity
– Oestrogen only HRT
– Tamoxifen
– Polycystic Ovarian Syndrome
– Lynch syndrome (HNPCC)
Protective Factors:
– COCP, later pregnancy, Breastfeeding, Smoking
Symptoms:
– Post-menopausal bleeding (bleeding 1 year after the last menstrual period)
– In premenopausal women it can present as a change in menstrual bleeding or intermenstrual bleeding
Diagnosis:
– Bimanual examination to assess uterus, ovaries
– 1st line is transvaginal ultrasound used to measure the endometrial thickness
– Also looks for free fluid, heterogeneity and invasion of endo/myometrium
–> If thickness <4mm, no further investigations required
–> If thickness > 4mm (post-menopause) or >7 (premenopausal) –> proceed to 2nd step
– Also do Pipelle biopsy –> thin blind biopsy which the GP uses to get a sample of the endometrium
– 2nd step is hysteroscopy + biopsy –> Diagnostic test which indicates severity of disease.
Management:
Hyperplasia without atypia (low risk of cancerous progression):
– 1st line is discharge and manage risk factors (e.g. obesity)
– If this persists –> progesterone treatment with Mirena coil or LNG-IUS to reduce hyperplasia
Hyperplasia with atypia (high risk of cancerous progression):
– If post-menopausal or does not want childrena –> hysterectomy
– If wants children –> progesterone treatment quickly, have baby and then hysterectomy after
Full adenocarcinoma:
The FIGO1 staging system is used to decide treatment
Stage | Description | Treatment |
I | Carcinoma confined within the uterine body | Total abdominal hysterectomy with bilateral salpingo-oophorectomy (+ post- op radiotherapy) |
II | Carcinoma may extend to the cervix but not beyond the uterus | |
III | Carcinoma extends beyond the uterus but is confined to the pelvis | |
IV | Carcinoma involves bladder/bowel or has distant metastases | Probably palliative progestogen therapy |
Adenomyosis
A condition in which endometrial tissue is present within the myometrium (muscle layer) of the uterus
– Thought to result from abnormal healing of damaged endometrium in which the endometrium aberrantly invaginates into the myometrium
Risk factors:
– Uterine damage: childbirth, previous C-section or surgery
Symptoms:
– Typically seen in multiparous women age 40-50yrs
– Dysmenorrhoea
– Menorrhagia
– Enlarged, boggy uterus
Diagnosis:
– Transvaginal Ultrasound or MRI
Management:
– Non-hormonal –> mefenamic/tranexamic acid to relieve menorrhagia
– Hormonal –> Low dose COCP, high-dose oral progestogens, Mirena
– Surgical = uterus-conserving (e.g. endometrial ablation, uterine artery embolization), or hysterectomy

Fibroids (leiomyomas)
These are benign tumours of the uterine wall composed of smooth muscle and fibroblasts.
Risk factors
– Age, early puberty, obesity, ethnicity (more common in black and Asian women)
Fibroids are classified according to their wall position:
i) Intramural:
These develop completely within the myometrium and do not extend into the uterine or peritoneal cavity
ii) Submucosal:
These develop in the inner aspect of myometrium (under the inner mucosa) and extend into the uterine cavity
iii) Subserosal:
These develop in the outer aspect of the myometrium (under the serosa) and extend into the peritoneal cavity

Symptoms:
Can be asymptomatic
– Most common symptom is heavy menstrual bleeding
– Pelvic pain
– Subfertility
– Pressure symptoms –> urinary frequency, bloating, constipation
– Firm, large, irregularly shaped uterus on bimanual exam
– Can cause red degeneration –> a haemorrhage into the tumour that usually occurs during pregnancy, giving heavy bleeding and acute pelvic pain
Diagnosis:
Transvaginal ultrasound is the diagnostic test
Management:
First medical approaches are used, but if uncontrolled then surgical options:
i) Reducing bleeding:
–> 1st line is insertion of a Mirena (progesterone coil)
– If not suitable: COCP, cyclical oral progestogen, mefenamic acid, tranexamic
ii) Shrink Fibroids
—> Selective progesterone modulator (Ulipristal)
– GnRH analogues (Zolidex), can only be used for 6 months due to osteoporosis risk
iii) If uncontrolled, surgical options:
-Hysteroscopic resection of fibroids -> can be used for submucosal fibroids
– Hysterectomy -> most effective way of preventing recurrence
– Myomectomy -> alternative to hysterectomy if the woman wishes to preserve her fertility
iv) Non-Invasive procedures provide an alternative option to surgery and include:
– Uterine artery embolization -> risk of early miscarriage and placenta misplacement
– Endometrial ablation -> can be used for small fibroids in the uterine lining
Asherman Syndrome
This is the development of intrauterine adhesions
– It is caused by damage to the basal layer of the endometrium leading to formation of adhesions
– Amenorrhoea may occur in this condition as the adhesion tissue does not respond to oestrogen
– Mostly caused by procedures performed on the uterus -> typically surgical management of miscarriage/termination of pregnancy (but also endometrial biopsy, fibroid surgery)
Symptoms:
Secondary amenorrhea or little/infrequent menstrual bleeding and infertility
Diagnosis:
Hysteroscopy is the gold standard
Management:
Surgical excision of the adhesions
Endometriosis
This is a condition in which there is growth of endometrial tissue outside the uterine cavity
– The deposits are mostly found within the pelvis (e.g. ovaries, pouch of Douglas, bladder, rectum) but in rare cases may be seen in extra-pelvic locations like the diaphragm and pleural cavity
– As endometrial tissue responds to oestrogen, symptoms vary with the menstrual cycle
– At the time of menstruation there may be bleeding at the location of the ectopic tissue which can lead to pain and inflammation at these sites occurring in a cyclical fashion
– The chronic inflammation reduces fertility, but with treatment women can become fertile again
Symptoms:
– Pain –> chronic pelvic pain (>6 months), dysmenorrhea
– Deep dyspareunia
– GI symptoms –> painful bowel movements
– Urinary symptoms –> dysuria, haematuria
– Subfertility
– On examination there may be reduced organ mobility, enlargement and tender nodules in posterior vaginal fornix.
– Endometriotic lesions may be visible.
Diagnosis:
– Laparoscopy is used to identify ectopic lesions

Management:
Pain can be managed with:
– 1st line is NSAIDs and/or paracetamol
– 2nd line is COCP, progestogens (pill, implant or injection), Mirena
If these are ineffective, not tolerated or contraindicate, refer to gynaecology
– Treatment may involve laparoscopic excision/ablation of endometriosis
– GnRH agonists may be given as an adjunct before surgery
N.B. Subfertility in endometriosis should be managed by an MDT team involving fertility specialists. Surgical interventions can improve the chance of spontaneous pregnancy.


