This describes the 28-day cycle which occurs in women around the ages of 14 to 51, which controls the synthesis and release of egg cells and the associated hormonal changes that go along with this.
– The cycle starts on the first day of the period (menstruation) and ovulation usually occurs on day 14.
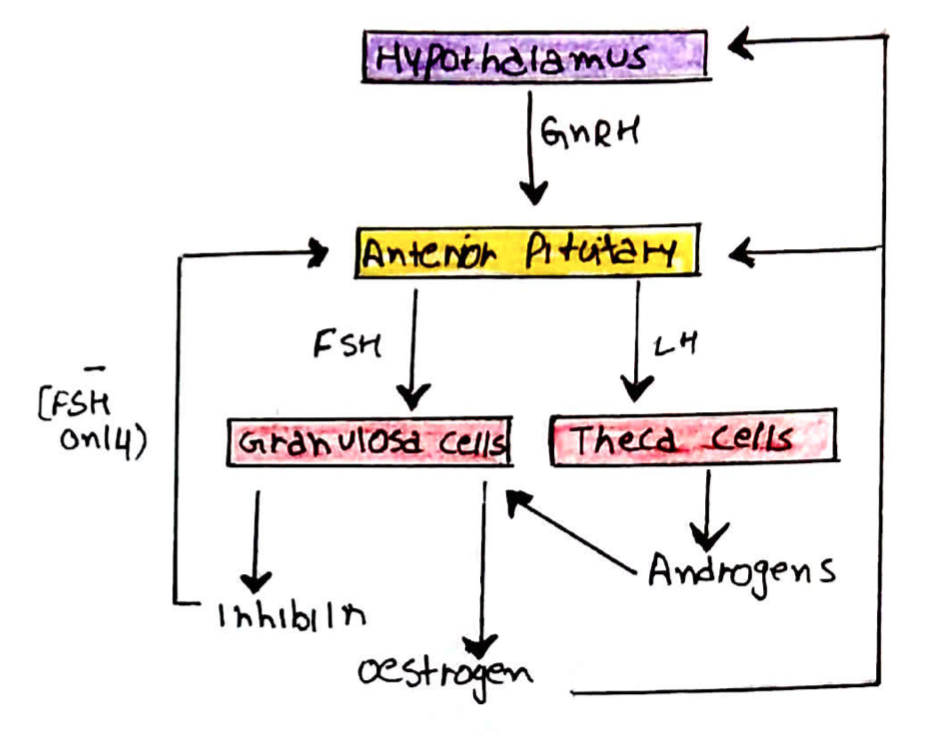
The changes that occur in the female reproductive system are coordinated by the hypothalamic-pituitary-ovarian axis:
– The hypothalamus produces gonadotrophin releasing hormone (GnRH)
– This stimulates the anterior pituitary to secrete follicular stimulating hormone (FSH) + luteinising hormone (LH)
– These hormones act on follicles within the ovaries:
LH = stimulates theca cells to produce androgens
FSH = stimulates growth of follicles, the conversion of the androgens to oestrogens by granulosa cells and stimulates inhibin production
This axis is under the influence of positive and negative feedback:
Negative feedback:
– Slowly rising oestrogen inhibits LH and FSH secretion
– Progesterone inhibits LH and FSH secretion
– Inhibin inhibits FSH secretion selectively
Positive feedback:
– Rapidly rising oestrogen stimulates LH and FSH secretion
The Ovarian Cycle
In the ovary, oocytes (eggs) develop within follicles.
Follicles contain 2 important types of cell:
i) Theca cells:
Express LH receptors and are stimulated by LH to produce androgens
ii) Granulosa cells:
Express FSH receptors and are stimulated by FSH to:
– Convert the androgens produced by theca cells to oestrogens
– Secrete inhibin which suppresses FSH production -> negative feedback
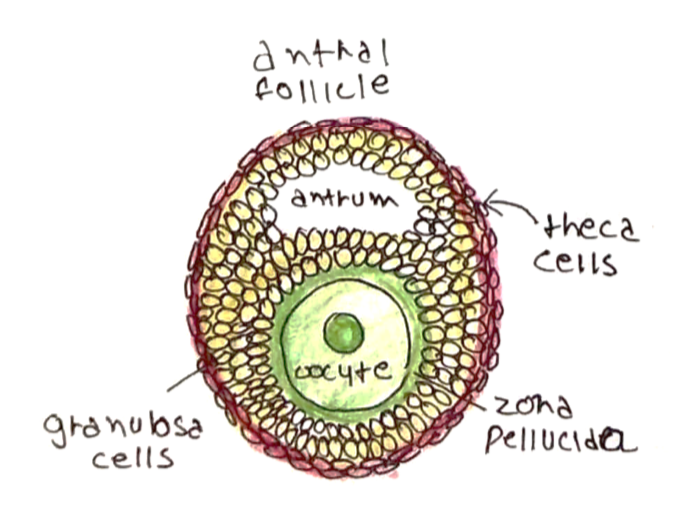
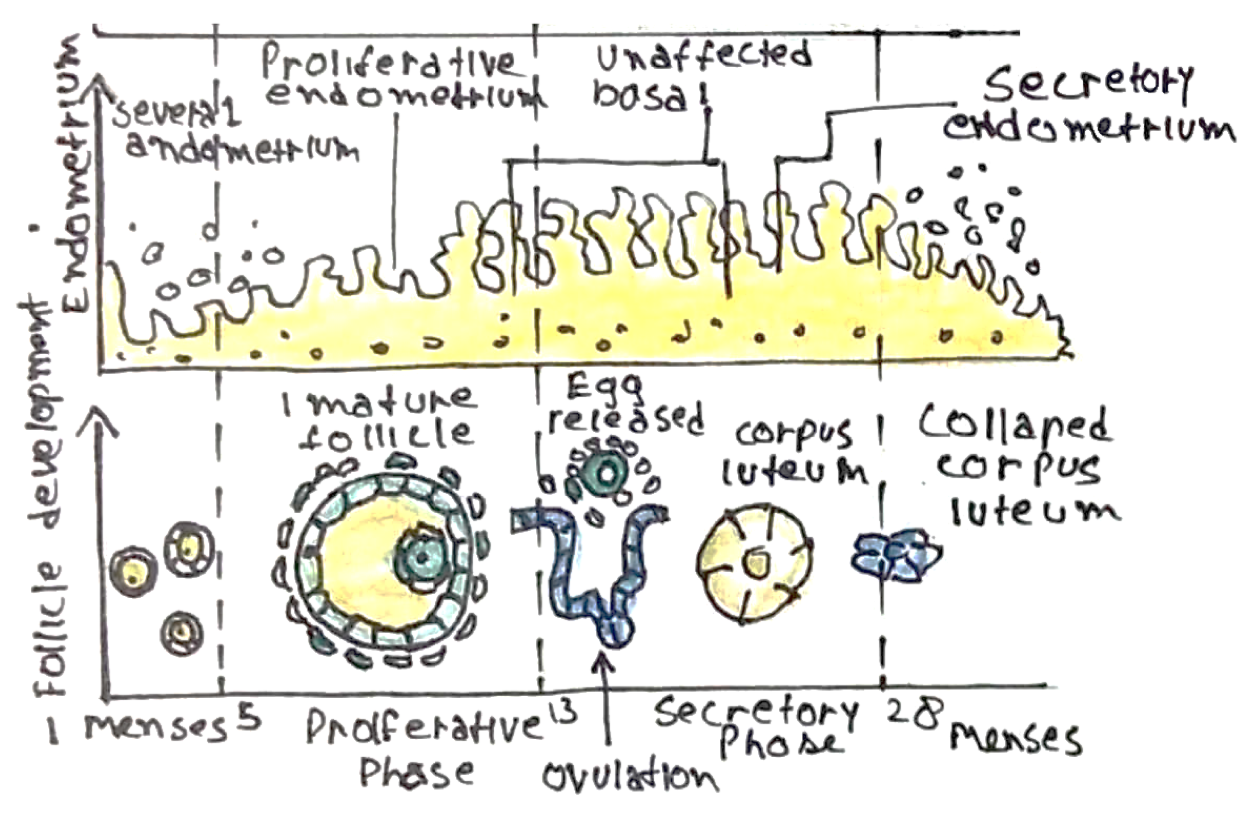
During the ovarian cycle, follicles progress through a series of development phases:
Primordial follicle -> preantral follicle -> antral follicle -> rupture (ovulation) -> corpus luteum -> corpus albicans
– Follicles are able to progress to preantral phase in the absence of exogenous hormones
– However, to develop to the antral stage, follicles require the influence of FSH/LH
– Follicles that are not stimulated by FSH/LH will undergo atresia
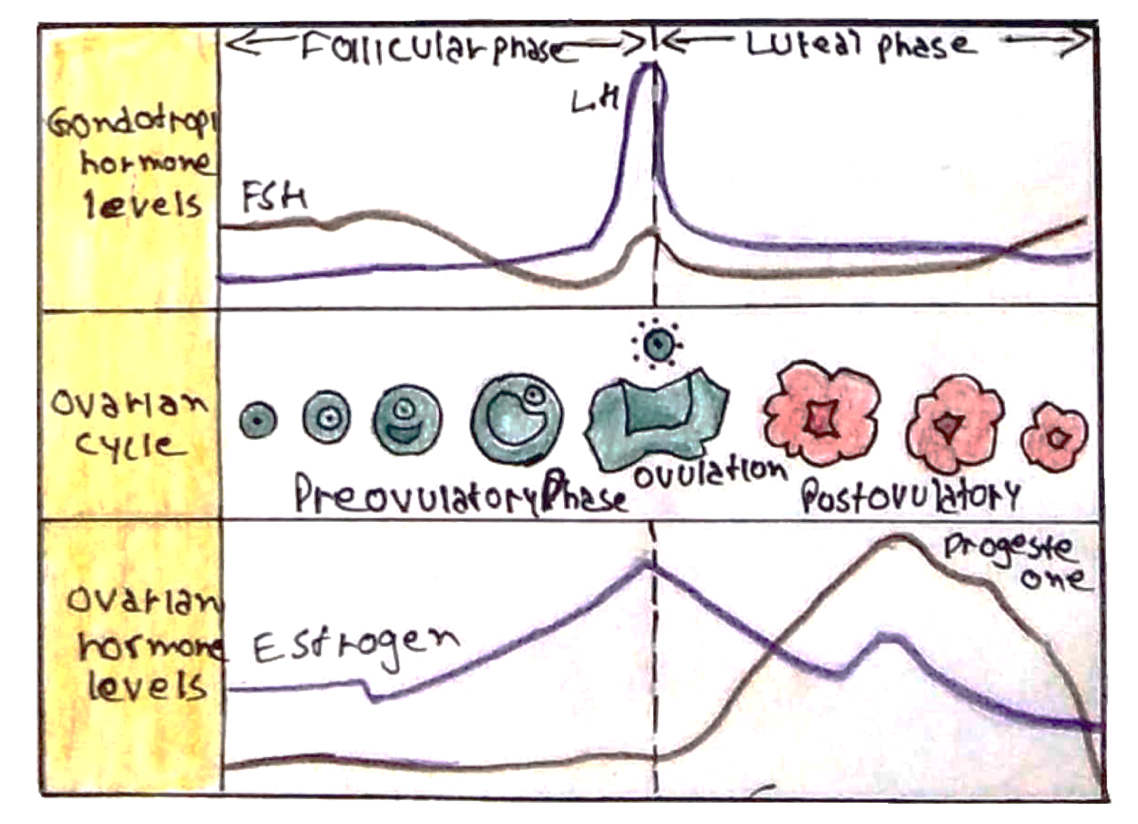
The ovarian cycle is divided into two phases, follicular (early and late) and luteal:
The Follicular Phase:
i) Early-mid follicular phase:
At the start of a cycle oestrogen, progesterone and inhibin levels are low
– As such, they exert little negative feedback and so LH and FSH levels rise
– These allow progression of follicles from the preantral to antral stage
– In turn, the developing follicles then begin to secrete oestrogen and inhibin
– These exert negative feedback resulting in a plateau in LH and a fall in FSH
(FSH declines because it is inhibited by both oestrogen and inhibin)

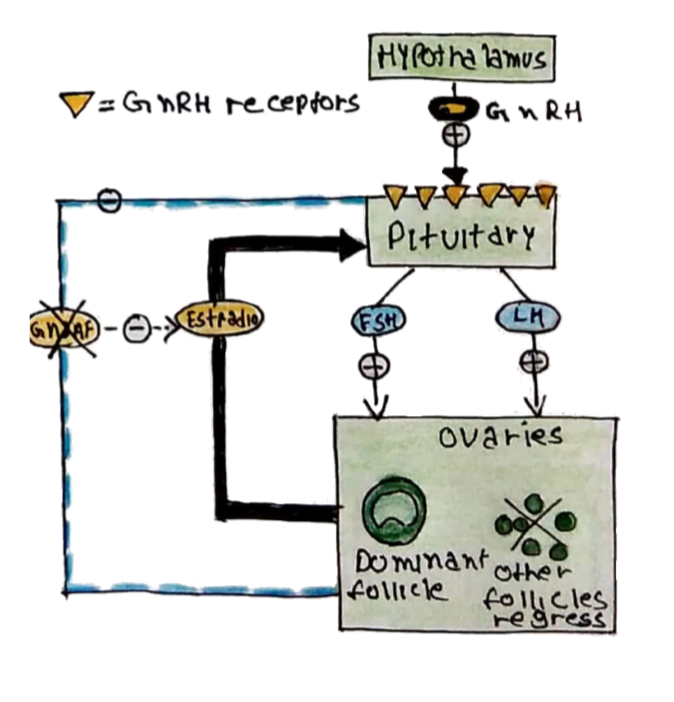
ii) Late follicular phase:
The levels of FSH are insufficient to maintain all the developing follicles and so a single dominant follicle is selected (the others undergo atresia)
– Selection of a dominant follicle leads to a rapid rise in oestrogen
– This has a positive feedback effect, leading to a surge in LH
– The LH surge triggers ovulation: rupture of the follicle with release of the oocyte into the fallopian tube
– Follicular rupture results in a fall in oestrogen and LH
The Luteal Phase:
The ruptured follicle undergoes some cellular changes to form a corpus luteum
– Theca cells -> become small luteal cells
– Granulosa cells -> become large luteal cells
– The corpus luteum secretes progesterone, oestrogen and inhibin
– These exert negative feedback on LH/FSH secretion, resulting in low levels of LH and FSH throughout the luteal phase
– The corpus luteum has a lifespan of about 14 days
The next stage is dependent on whether fertilisation occurs or not:
– If no fertilisation –> The corpus luteum breaks down (luteolysis)
– Luteolysis leads to a decline in luteal progesterone, oestrogen and inhibin
– This allows the rise in LH/FSH to occur marking the beginning of the next cycle
– If fertilisation occurs –> the embryo secretes hCG which prevents luteolysis and maintains the corpus luteum
– The placenta eventually takes over the role of the corpus luteum (from 8 weeks).
The Uterine Cycle
Structural changes in the uterus occur alongside those occurring in the ovary. These changes are also divided into phases:
i) The proliferative phase = coincides with the follicular phase of the ovarian cycle
ii) The secretory phase = coincides with the luteal phase of the ovarian cycle
iii) Menses = initiated by luteolysis
Phase | Main Hormone | Uterine Changes |
Proliferative phase | Oestrogen | These are changes that enhance the chance of fertilisation: – Endometrium = endometrial thickening and development of simple tubular glands –> secrete a fluid that aids sperm transport – Cervical mucus = thin and alkaline –> to enhance sperm penetration
|
Secretory phase | Progesterone | These are changes that prepare for implantation of an embryo: – Endometrium = endometrial thickening and further development of glands to become branched and more complex – Cervical mucus = thick and acidic -> to prevent sperm penetration
|
Menses
Menses marks the beginning of a new cycle, which involves the shedding of the uterine lining via the vagina
– It occurs when the corpus luteum breaks down (hence the absence of menstruation when fertilisation has occurred, as the corpus luteum is maintained)
– According to the NHS website:
– Menstrual bleeding usually lasts 3-8 days (average = 5 days)
– Blood loss is usually between 30-72ml (equivalent of 5-12 teaspoons)
A cycle usually starts on the first day of a woman’s period and ends the day before her next period
– The average length of a complete cycle is 28 days, but this can vary (the NHS1 considers a normal menstrual cycle as any lasting between 21 and 40 days)
– Ovulation occurs 10-16 days before a woman’s next period

