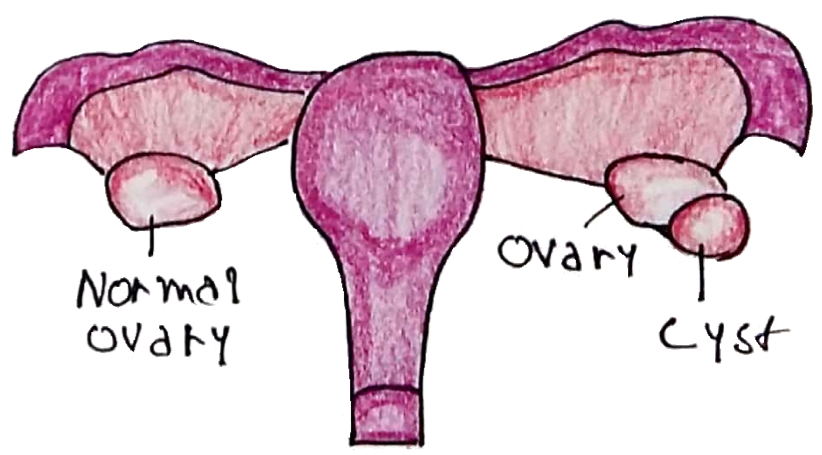
It is not uncommon to develop cystic masses on the ovaries.
– In premenopausal women, most ovarian masses are benign.
– The incidence of ovarian cancer increases with age, so postmenopausal women are at a higher risk of malignancy
– There are both non-neoplastic and neoplastic types of cysts which can occur naturally or be pathological:
a) Non-Neoplastic Cysts:
Physiological:
These cysts develop as part of the menstrual cycle. They are considered physiological and usually self-resolve over 2-3 menstrual cycles. They include:
–> Follicular cysts:
These occur when the dominant follicle does not rupture releasing the egg cell
–> Corpus luteum cyst:
This occurs when the corpus luteum fails to breakdown but persists in the ovary
Pathological:
You can also get pathological cysts which can be seen in Polycystic ovary syndrome (PCOS)
–> Theca luteum cyst:
This occurs secondary to conditions which cause high levels of hCG (e.g. multiple pregnancies, trophoblastic disease)
b) Benign Neoplastic Cysts
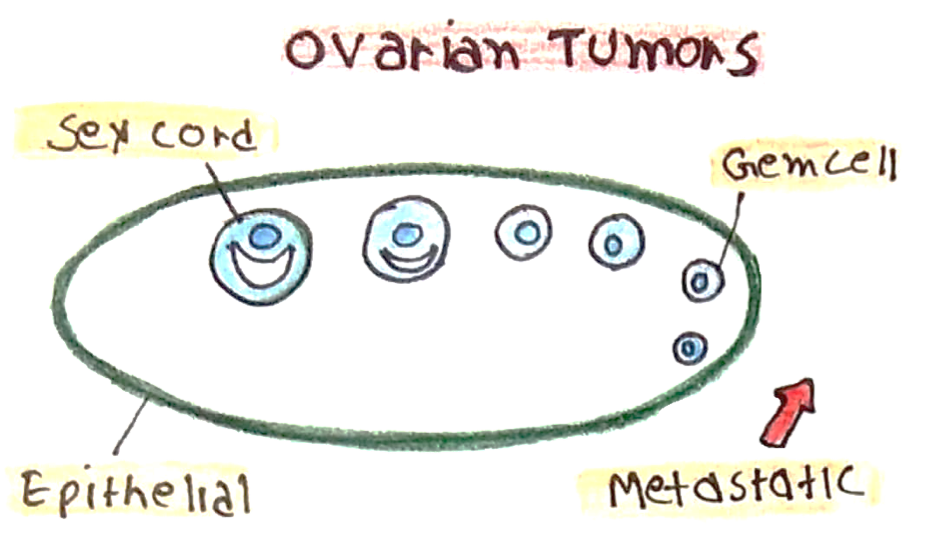
Epithelial:
This is the most common type (60%) of benig novarian tumours, including:
–> Serous cystadenoma:
This is most common in women age 40-50yr
–> Mucinous cystadenoma:
These can can be huge. They secrete mucus which can cause pseudomyxoma peritonei
Germ cell tumours:
These occur due to a proliferation of the germ cells, which are seen in younger women
–>Dermoid cysts:
These are most common in young women. They may contain differentiated tissues (e.g. hair, teeth, fat) which originate from different embryological layers like the ectoderm
– They contain a Rokitansky protuberance where the skin and hair is often found
Sex chord stromal tumour:
–> Fibroma:
These may present with Meig’s syndrome (ovarian tumour + ascites + pleural effusion)
–> Sertoli-Leydig cell tumour:
This secretes androgens which leads to masculinization
Endometrioma:
This is a cyst which develops in individuals with endometriosis
– Also known as ‘chocolate cysts’ because of their brown appearance
c) Malignant Neoplastic Cysts
Epithelial:
This is the most common type representing 90% of primary ovarian cancers, including:
–> Serous cystadenocarcinoma:
This is a malignant proliferation of the serous cells
–> Mucinous cystadenocarcinoma:
This is amalignant proliferation of the mucus producing cells
Germ cell tumours:
These are most common in younger women and are typically hormone secreting
–> Yolk sac tumours:
This is a proliferation of cells that resemble yolk sac elements + secretes AFP
–> Dysgerminomas
This is the most common type of germ cell tumour and it secretes LDH
–> Non-gestational choriocarcinoma:
This is a proliferation of cyto/syncitiotrophoblasts +secretes hCG
Sex-chord stromal tumour:
–> Granulosa cell tumour:
This is a malignant proliferation of granulosa cells which is oestrogen secreting
Metastatic tumours:
–> Krukenberg tumour:
This is a metastatic lesion which occurs in the ovaries. Usually due to breast, endometrial or GI tumours
Ovarian Cysts (Benign)
This refers to benign masses which can be fluid filled found on the ovaries.
– Many of these are asymptomatic but can give very similar symptoms to ovarian cancer.
– Can have acute complications –> rupture, haemorrhage, torsion, infection
Diagnosis (RCOG2):
Uses the same tests as for ovarian cancer: USS and CA-125 used to calculate RMI
RMI – Risk of Malignancy Index
– If premenopausal woman has simple cyst on US –> CA-125 is not needed
– This is because CA-125 can give false positives as it is raised in fibroids, pelvic infection, endometriosis
– If postmenopausal, there is a greater risk of malignancy so both CA-125 and USS are always carried out
Management (RCOG2 guidelines):
– If RMI indicates high risk of malignancy, management is as ovarian cancer (see below)
Premenopausal:
– Small (<50mm) cysts –> no follow-up (most likely functional cysts which usually self-resolve)
– Large (>50-70mm) simple cysts –> yearly follow-up
– Very large (>70mm) simple cysts –> further imaging (MRI) or surgical intervention
– Cysts that persist or increase in size –> surgical intervention (cystectomy or oophorectomy)
Post-menopausal (RCOG3 guidelines):
– If asymptomatic, simple and <5cm –> Reassess the cyst in 4-6 months (CA-125+ TVUS)
– If symptomatic, non-simple or >5cm –> Surgical removal using laparoscopic bilateral laparoscopic salpingo-oopherectomy
Ovarian Cancer (Malignant)
This is a malignant proliferation of cells originating from one of the cell types of the ovary.
– It is usually seen in postmenopausal women around 60 years and is often diagnosed quite late.
Risk factors:
Age, high number of ovulatory cycles (nulliparity, early menarche, late menopause), HRT
– BRCA1 or 2 genes, Lynch syndrome
Symptoms:
– Abdominal distension (bloating)
– Pelvic or abdominal pain
– Early satiety or loss of appetite
– Increased urinary urgency and/or frequency
– Women >50yrs with IBS symptoms
Diagnosis (NICE1):
At GP: 1st is CA-125 –> if >35IU/ml perform transvaginal ultrasound scan
– If USS appearance suggestive of cancer urgent 2-week referral to gynaecology
– Women who have ascites or pelvic/abdominal mass should get 2-week referral ASAP (without scan)
At gynaecology:
– In women <40yrs, measure AFP and beta-hCG (to check for germ cell tumours)
– Calculate the risk of malignancy index (RMI) which gives you indication of the malignancy risk.
Management:
– If RMI of 250+ refer to specialist MDT team and do CT CAP for staging of disease.
– If stage 1 cancer –> debulking surgery = full hysterectomy + removal of omentum (site of usual metastasis)
– If stage 2/3 cancer –> 1st is chemotherapy (cisplatin + taxol) follow by debulking surgery, then chemo again
– Can give PARP inhibitors (Olapurib) –> prevents DNA repair mechanisms so the cancerous cells which already have bad DNA repair are futile and die

