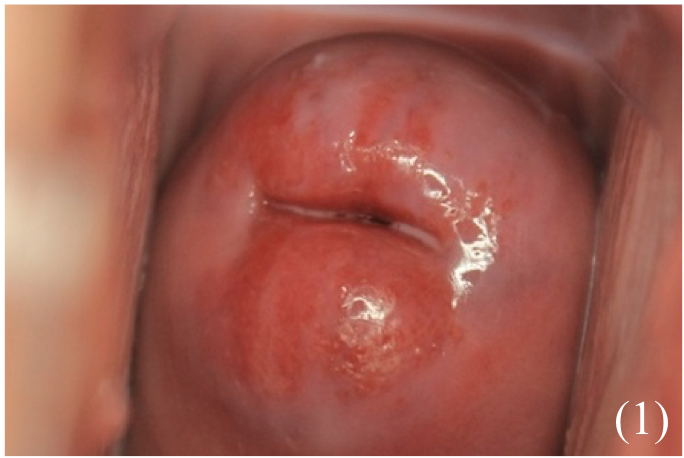
Cervical Ectropion
A condition in which simple columnar epithelium (lining the endocervix) is present on the ectocervix.
– This type of epithelium is more fragile than the stratified squamous epithelium that usually lines the ectocervix and may bleed after sexual intercourse
– Ectropion can also lead to increased vaginal discharge as simple columnar cells are mucus-producing
– It is diagnosed clinically after ruling out other more sinister pathologies like cervical cancer.
Causes:
– Raised oestrogen levels (e.g. pregnancy, COCP)
Symptoms:
Mostly asymptomatic but may cause: – Post-coital bleeding
– An increase in vaginal discharge
– Pain/bleeding during cervical screening
– On examination -> red, velvety area on the ectocervix
Investigations:
– Swabs and smear to rule out infection and CIN/cervical cancer
Management:
– Do not treat unless it is symptomatic
– If on COCP, consider switching to another COCP with a lower dose of oestrogen or to the POP
– Can do silver nitrate cauterisation or cold coagulation of the columnar epithelium
Cervical Polyps
These are benign growths on the cervix which result from hyperplasia of the columnar epithelium – Usually benign but carry a risk of malignant transformation and so must be removed
Symptoms:
– May be asymptomatic and found incidentally on speculum examination or may cause:
– Abnormal vaginal bleeding (menorrhagia, IMB, PCB, PMB)
– Abnormal vaginal discharge
– Difficulty taking smear sample
Investigations:
– Do swabs and smear to rule out infection/cervical cancer
Management:
– Remove polyp + send for histological evaluation to exclude malignancy
N.B. Some recommend only removing symptomatic polyps as risk of malignant change in asymptomatic polyps may be so low that removal is unnecessary
Cervical Cancer
This is an invasive carcinoma of the cervical epithelium, which usually present as post-coital bleeding
– It is usually seen in 30-year olds (more sexually active) and >50 years old (less immune surveillance)
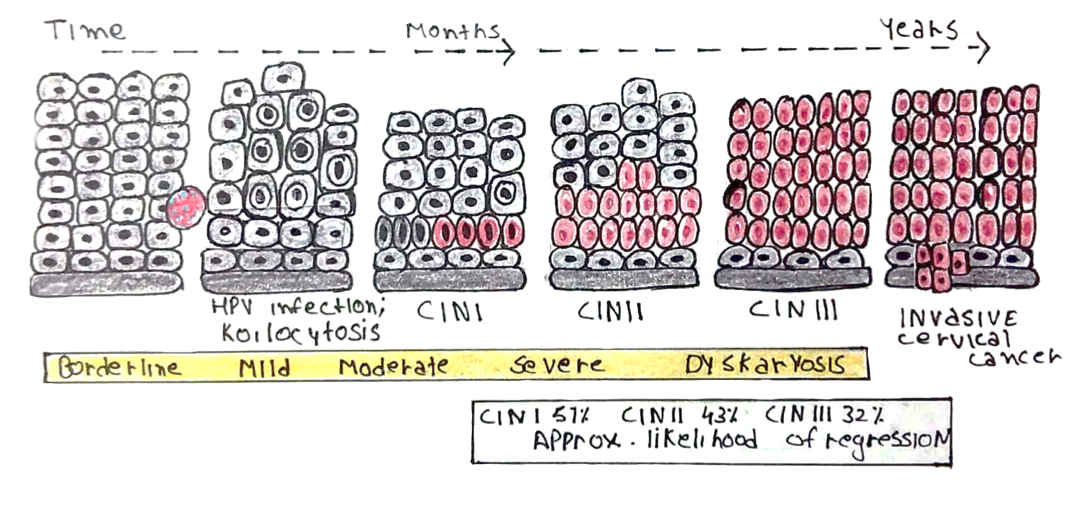
– CIN is characterized by nuclear changes and increased mitosis in the transformation zone (the junction between the endocervix and ectocervix)
Divided into 3 grades according thickness of dysplastic cells:
– CIN 1 < 1/3 thickness of epithelium
– CIN 2 < 2/3 thickness of epithelium
– CIN 3 < complete thickness of epithelium
– Carcinoma in situ (CIS) = involves entire thickness
– It can then become invasive when it begins to invade through the basement membrane.
– CIN classically progresses in stepwise fashion through the grades to full carcinoma, but can regress
Risk factors:
– The main risk factor is infection with Human Papilloma Virus (HPV) types 16 + 18
– These make proteins E6 (inhibits p53) and E7 (affect RB) increasing risk of cancer.
– Factors which increase HPV infection –> Many sexual partners, age at first sexual intercourse, condom use
– Factors which increase progression –> Smoking, COCP use, high parity, co-infection with other STIs
– Factors which increase both –> HIV or immunosuppressed patients
Symptoms:
Most are asymptomatic and detected on screening:
– Intermenstrual bleeding, postcoital bleeding, postmenopausal bleeding
– Blood-stained, mucoid or purulent vaginal discharge
– Pelvic pain/dyspareunia

Cervical Cancer Screening
Diagnosis:
Colposcopy and biopsy, used to definitively measure degree of CIN
Managament:
This depends on the extent of CIN
If CIN2/CIN3:
– Large loop excision of the transformation zone (LLETZ)
– This gives short term risk of bleeding, infection and pain
– Long term can result in dyspareunia and pre-term labour (as cervix is weaker) so women as given a progesterone pessary to keep the cervix more intact
If Full cervical carcinoma (confined to the cervix or only extending to the top of vagina):
– Surgery = Radical hysterectomy +/- removal of lymph nodes
– Warn the patient about damage to the obturator nerve as can affect adductors in legs
If advanced carcinoma:
– Options include chemotherapy, radiotherapy or palliative care
Other Management Options
Vaccination:
– To reduce the incidence of CIN, there is a school vaccination programme for HPV
– Offered to all 12- and 13-year olds (girls and boys) in School Year 8, given as 2 doses

