Introduction
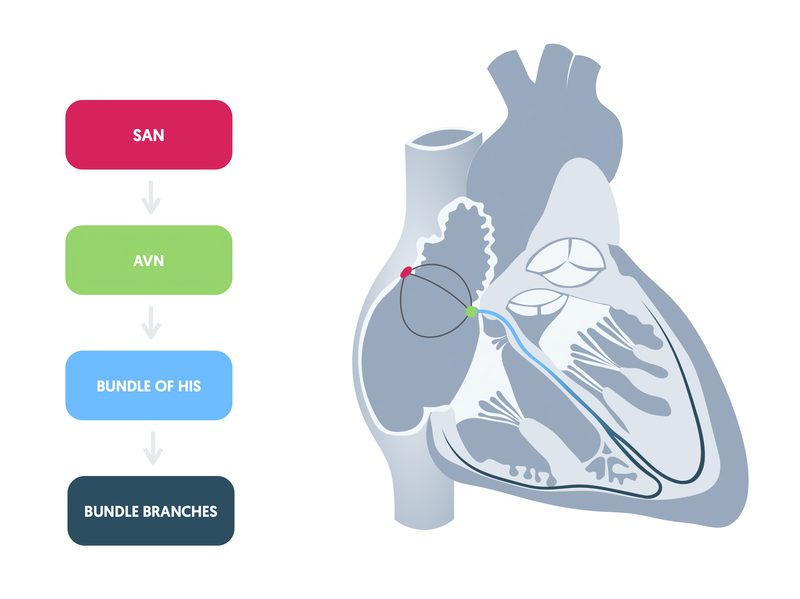
Normal cardiac conduction starts with electrical impulses that are initiated within the sinoatrial node.
The hearts pacemaker cells are organised into specialised structures including the sinoatrial node (SAN), atrioventricular node (AVN), bundle of His, the right and left bundle branches and Purkinje fibres. These are important for the coordinated spread of depolarisation (i.e. electrical impulses) that allows the heart to contract.
Hierarchy of spontaneous depolarisation
Each of the specialised structures involved in cardiac conduction has an intrinsic rate of autorhythmicity. This refers to the rate of spontaneous depolarisation, and therefore, the number of times the heart beats per minute.
- SAN: 60-100 bpm
- AVN: 40-60 bpm
- Ventricles: 20-40 bpm
The rate of autorhythmicity is highest in the SAN, which is why conduction is initiated here. If the SAN fails to undergo spontaneous depolarisation, electrical activity can be initiated lower down. This may occur in another part of the atrium, the AVN or the ventricles. When this happens, we call it an ‘escape’ rhythm.
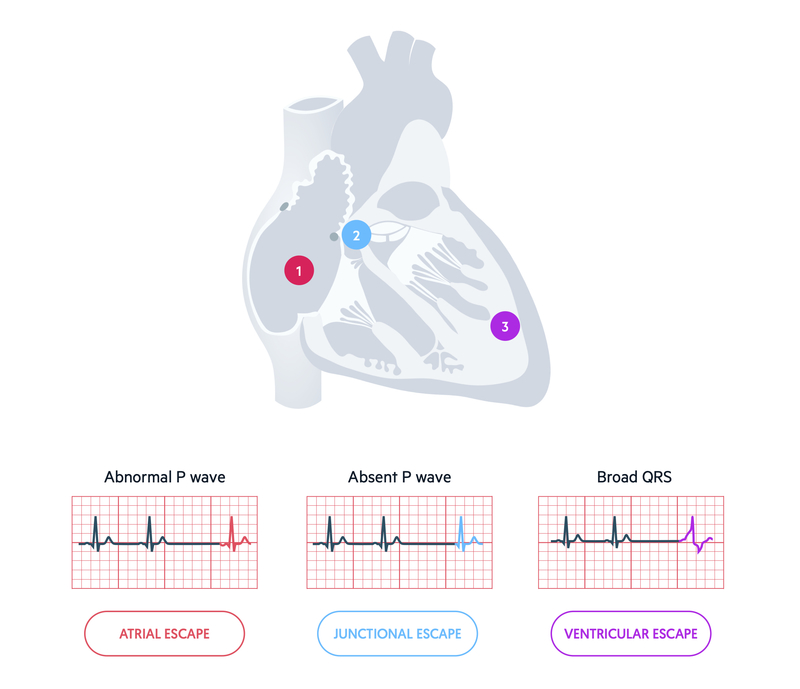
An escape rhythm may occur as a single beat or a sustained rhythm. A sustained escape rhythm is more likely to happen if there is complete failure of the conduction system above the level of the escape rhythm (e.g. AVN escape rhythm because SAN fails). Alternatively, it may occur if there is a disconnection between the atria and ventricles (e.g. complete heart block). A single beat may occur when part of the conduction system temporarily fails, then kicks back in (e.g. sinus pause).
Abnormal conduction
Problems with conduction may arise due to failure to initiate, or transmit, conduction.
As discussed, failure to initiate electrical impulses can lead to an escape rhythm as part of the conduction system lower down takes over as the main pacemaker with its own intrinsic rate of autorhythmicity.
Failure to properly propagate electrical activity can also lead to abnormal conduction. This can occur within the SAN, AVN or bundle branches. When electrical activity is not transmitted along the normal pathway we typically refer to it as a ‘block’.
A block may occur at any level (e.g. SAN, AVN or bundle branches). However, in clinical practice when we refer to ‘heart block’ we are usually referring to a block occurring at the level of the AVN. Depending on the level and severity of the block, it may be associated with a missed beat followed by resumption of normal electrical activity or an escape rhythm.
Sinoatrial node
Conduction problems with the SAN may manifest in many different ways.
The SAN is the main pacemaker of the heart that initiates electrical activity. Dysfunction of the SAN may manifest as failed initiation of conduction (i.e. pauses/arrest) or failed transmission of electrical activity (i.e. sinoatrial exit block).
Collectively, these problems may be part of a more global disorder of the SAN known as ‘sinus node dysfunction’ (SND) or ‘sick sinus syndrome’. SND comprises a variety of disturbances affecting both generation of electrical activity from the sinus node and transmission within the atria.
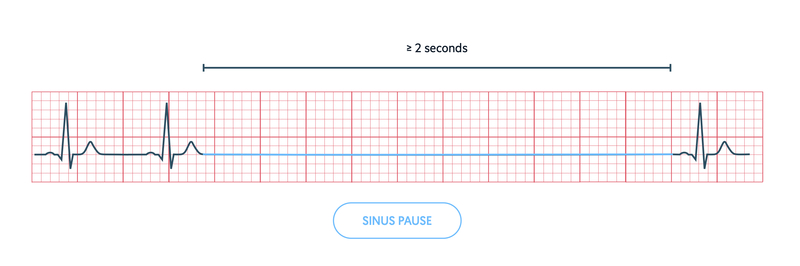
Sinus pause or arrest
Defined as a transient absence of P waves that lasts from 2 seconds to several minutes.
Due to failure of the SAN to initiate electrical activity. May be followed by resumption of normal electrical activity from the SAN or appearance of an escape rhythm (e.g. atrial or junctional escape).
Sinoatrial exit block
Defined as the interference of transmission of electrical activity from the SAN to neighbouring atrial tissue. This manifests as an absent P wave on the ECG.
Sinoatrial exit block can be further differentiated into multiple subtypes, each with different ECG appearances. However, this is beyond the scope of these notes.
Atrioventricular node
The AV node introduces a delay in conduction between the atria and ventricles to allow time to complete ventricular filling.
The time taken for depolarisation to pass from the SAN to the ventricular muscle is determined by the PR interval on the ECG. The normal PR interval is 3-5 small squares, which equates to 120-200 ms. The delay in conduction introduced by the AVN is important to allow time for ventricular filling to complete before ventricular contraction.
Interference of the normal transmission of conduction within the AVN can lead to varying degrees of block. These are commonly referred to as ‘heart blocks’ and may be differentiated into three types: first-degree, second-degree and third-degree.
- First-degree heart block: common. Seen in normal people. May indicate wider conduction problems. No specific action.
- Second-degree heart block: usually indicates underlying conduction disease. May require temporary or permanent pacing.
- Third-degree heart block: always indicates conduction disease. Requires temporary or permanent pacing.
First degree heart block
A delay in conduction of the normal wave of depolarisation from the SAN to the ventricles. This is manifested as a constant prolongation of the PR interval > 200 ms.
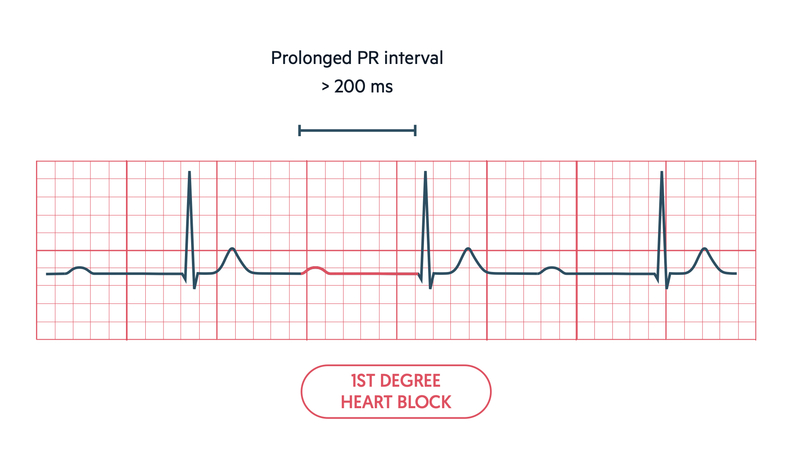
First degree heart block, by itself, is not clinically important. However, it may be a sign of more serious conduction abnormalities in the right clinical context (e.g. infective endocarditis and aortic root abscess) or when other blocks are seen on the ECG (e.g. bundle branch blocks).
Second degree heart block
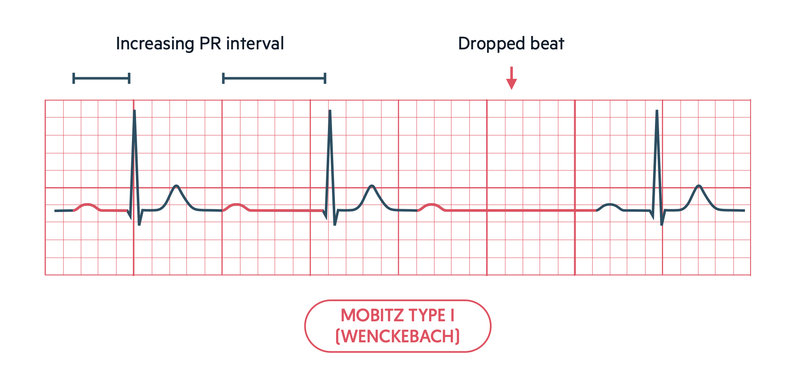
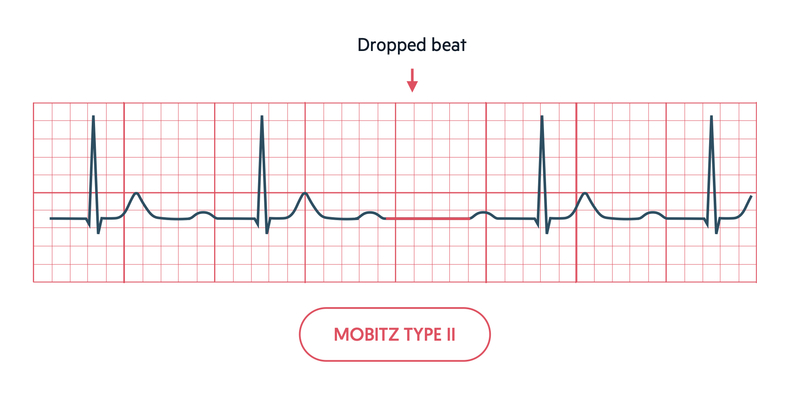
Occasionally, conduction may fail to pass through the AVN or His bundle to the ventricles. Intermittent failure of conduction is referred to as second degree heart block. This can broadly be divided into two types: Mobitz type I (Wenckebach) and Mobitz type II.
In Mobitz type I or Wenckebach, there is progressive lengthening of the PR interval, which is followed by failed conduction of an atrial beat. After the non-conucted beat, a normal conducted beat occur with a shorter PR interval and the cycle is continued
In Mobits type II there is a constant PR interval but occasionally atrial conduction is not transmitted to the ventricles leading to random ‘missed’ beats. This is seen as a P wave without a corresponding QRS.
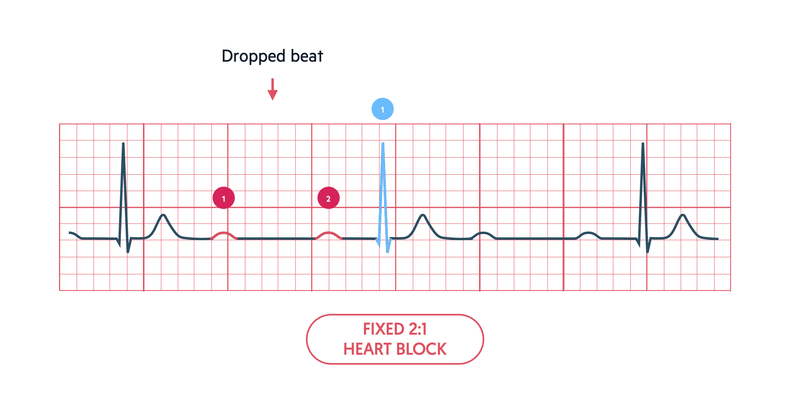
There may be evidence of a fixed ratio block due to alternating conducted and non-conducted atrial beats. We look at the number of P waves in the R-R interval and compare this to the distant R wave. If two P waves occur for every R wave, it is a 2:1 block. If three P waves occur for every R wave it is a 3:1 block.
Third degree heart block
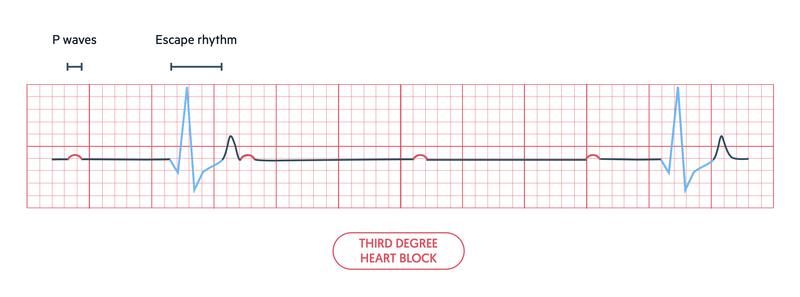
If there is complete failure to conduct atrial impulses to the ventricles via the AVN, we call this complete heart block. We say there is AV dissociation, because the atria and ventricles are not communicating with one another.
On an ECG, we can see this as P waves that have no association with the QRS complexes. The atria are being conducted normally so we see P waves. However, the ventricles are being conducted by a slow ventricular escape rhythm so we see broad (> 120 ms) QRS complexes.
Bundle branches
Following conduction via the AVN and His bundle, electrical impulses travel down the right and left bundle branches.
Disturbance to normal conduction down the right or left bundle branches leads to a delay in depolarisation of the corresponding ventricular muscle.
The time taken to depolarise the ventricles increases as the wave of depolarisation must travel from the opposite ventricle to depolarise muscle supplied by the bundle branch that is blocked. This is seen as a wide QRS on the ECG. Both left and right bundle branch blocks have characteristic patterns on the ECG. Blockage of both bundle branches is equivalent to blocking the AVN/His bundle and leads to complete heart block.
We can determine the origin of a broad QRS by its relationship with P waves. In bundle branch block and sinus rhythm, P waves are present, the PR interval constant and each P wave is in a 1:1 ratio with a QRS complex. In a ventricular escape rhythm or complete heart block, P waves may be absent or in no association with the QRS complex.
Right bundle branch block (RBBB)
In RBBB, there is a block in the right bundle branch leading to an absence of conduction. Depolarisation occurs down the left bundle branch as normal. Depolarisation of the right ventricle occurs after the left as the wave of depolarisation spreads from the left side of the heart to the right.
RBBB leads to a characteristic pattern in the QRS morphology in the chest leads V1 and V6 due to the direction of conduction. This is sometimes remembered as MaRRoW. This means an ‘M’ pattern in V1 and ‘W’ pattern in V6 is suggestive of RBBB.
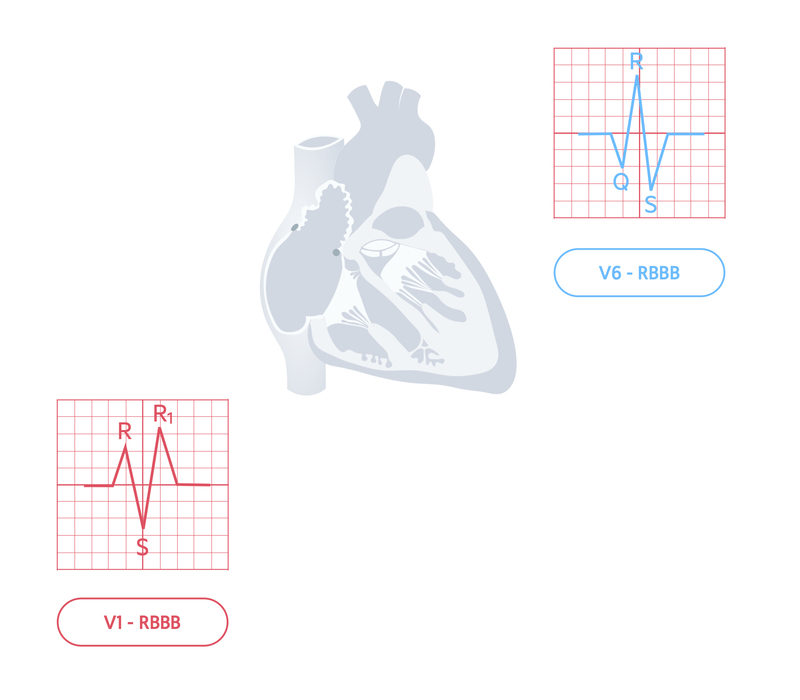
However, the easiest way of determining RBBB is just by looking at V1. If the QRS complex has a predominantly positive deflection, in other words the R wave is pointing up, it is a RBBB.

RBBB may indicate disease in the right side of heart. This can be seen with pulmonary pathology or pulmonary embolism. Alternatively, RBBB may be a normal variant in some healthy individuals
Left bundle branch block (LBBB)
In LBBB, there is a block in the left bundle branch leading to the absence of conduction. Depolarisation occurs down the right bundle branch as normal. Depolarisation of the left ventricle occurs after the right as the wave of depolarisation spreads from the right side of the heart to the left.
LBBB leads to a characteristic pattern in the QRS morphology in the chest leads V1 and V6 due to the direction of conduction. This is sometimes remembered as WiLLaM. This means an ‘W’ pattern in V1 and ‘M’ pattern in V6 is suggestive of LBBB.
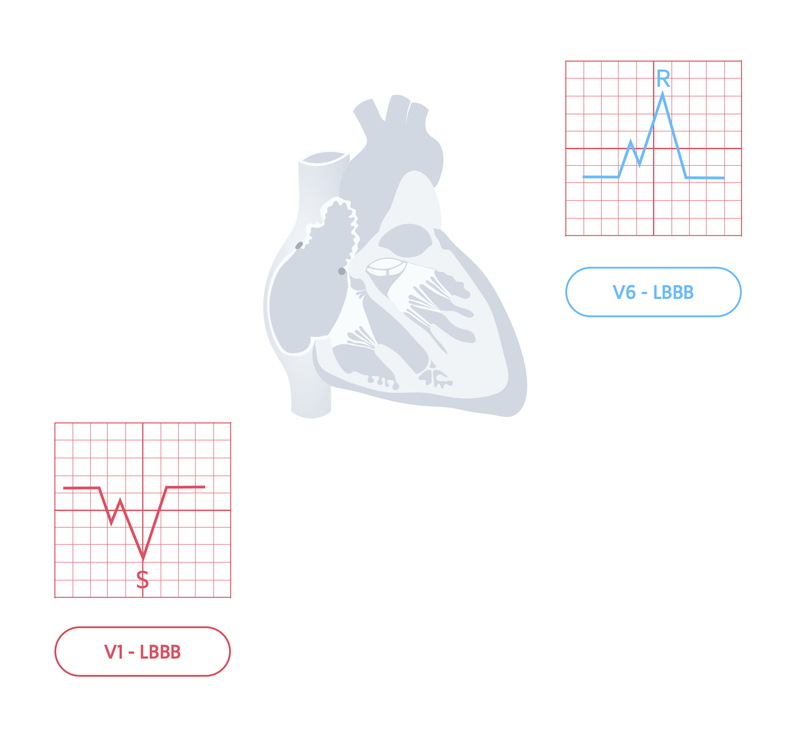
However, the easiest way of determining LBBB is just by looking at V1. If the QRS complex has a predominantly negative deflection, in other words there is mainly an S wave pointing down, it is LBBB.

LBBB always indicates underlying cardiac disease. New LBBB may be a sign of acute myocardial infarction and should be treated like an ST elevation myocardial infarction (STEMI) until proven otherwise. LBBB prevents further detailed interpretation of an ECG.
Distal left bundle branch disturbances
The left bundle branch further divides into two fascicles: anterior fascicle and posterior fascicle. The right bundle branch has no major divisions.
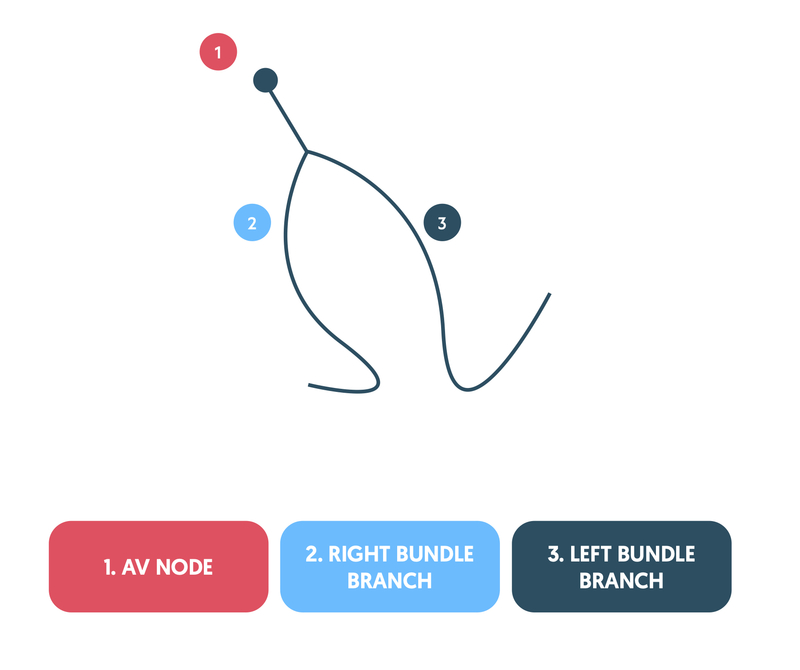
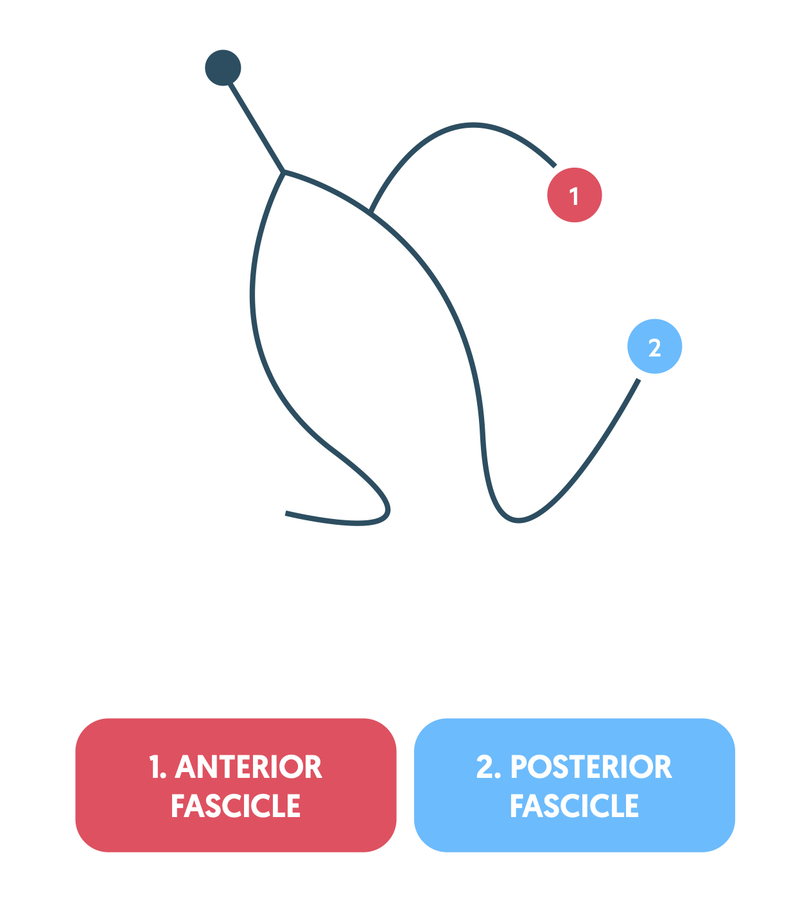
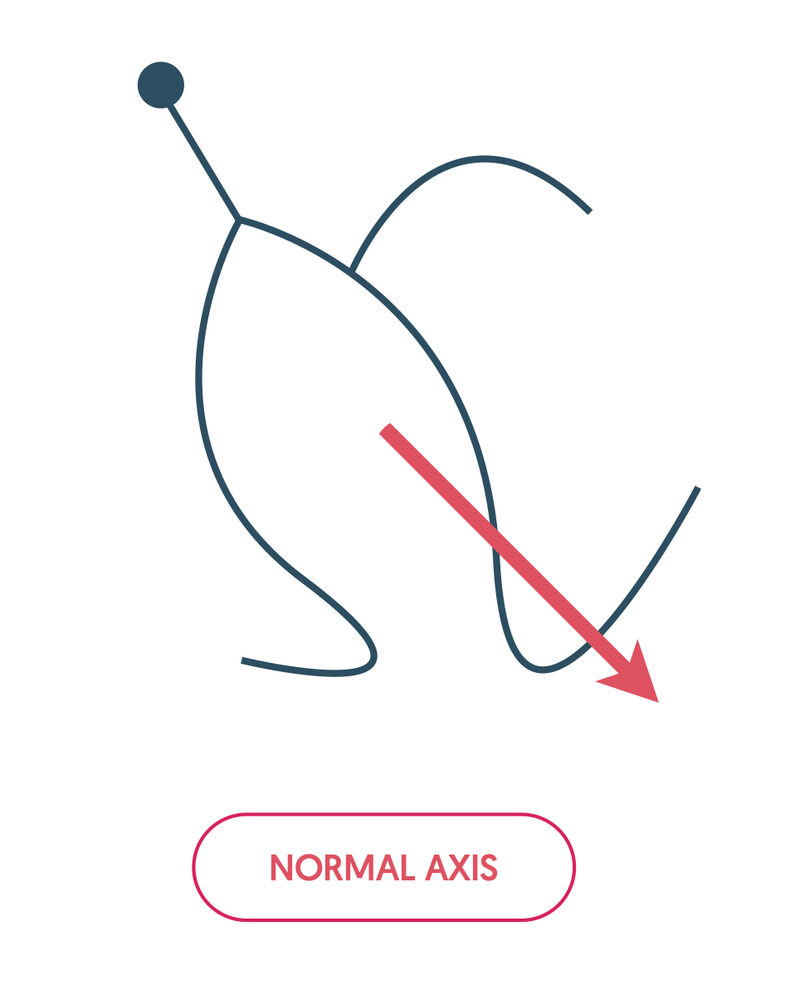
The cardiac axis refers to the average spread of depolarisation and it is influenced by the direction of the right bundle branch, anterior fascicle and posterior fascicle.
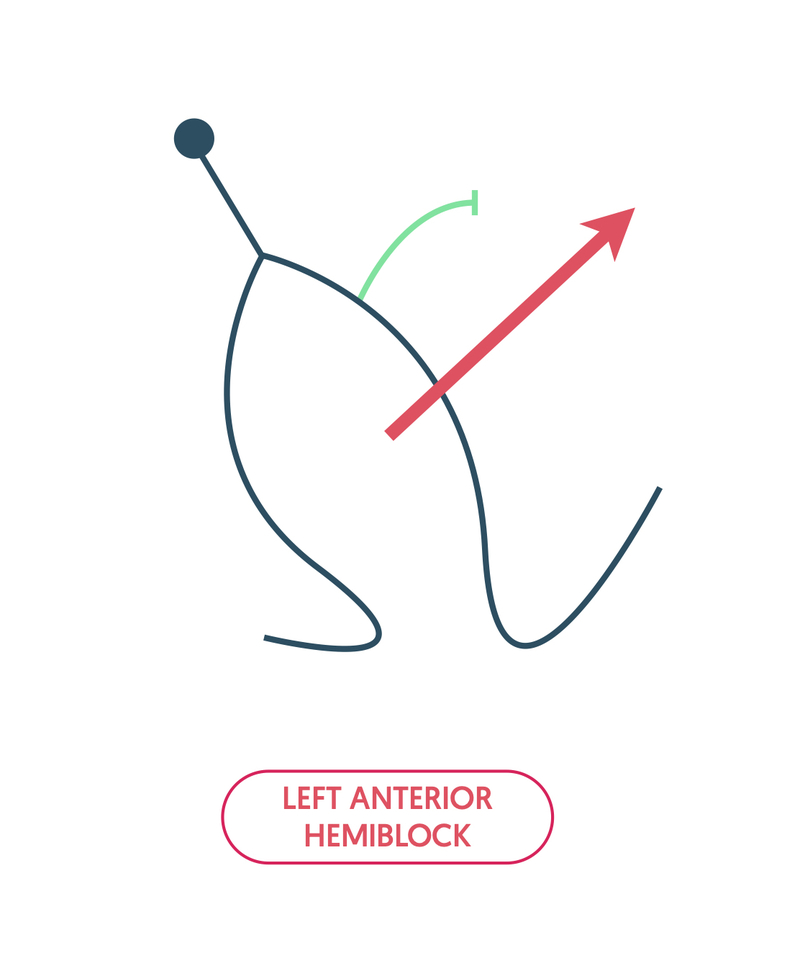
A common conduction abnormality is left anterior hemiblock, which is due to block of the anterior fascicle. This moves the average spread of depolarisation to the left, leading to left axis deviation (LAD) on the ECG.
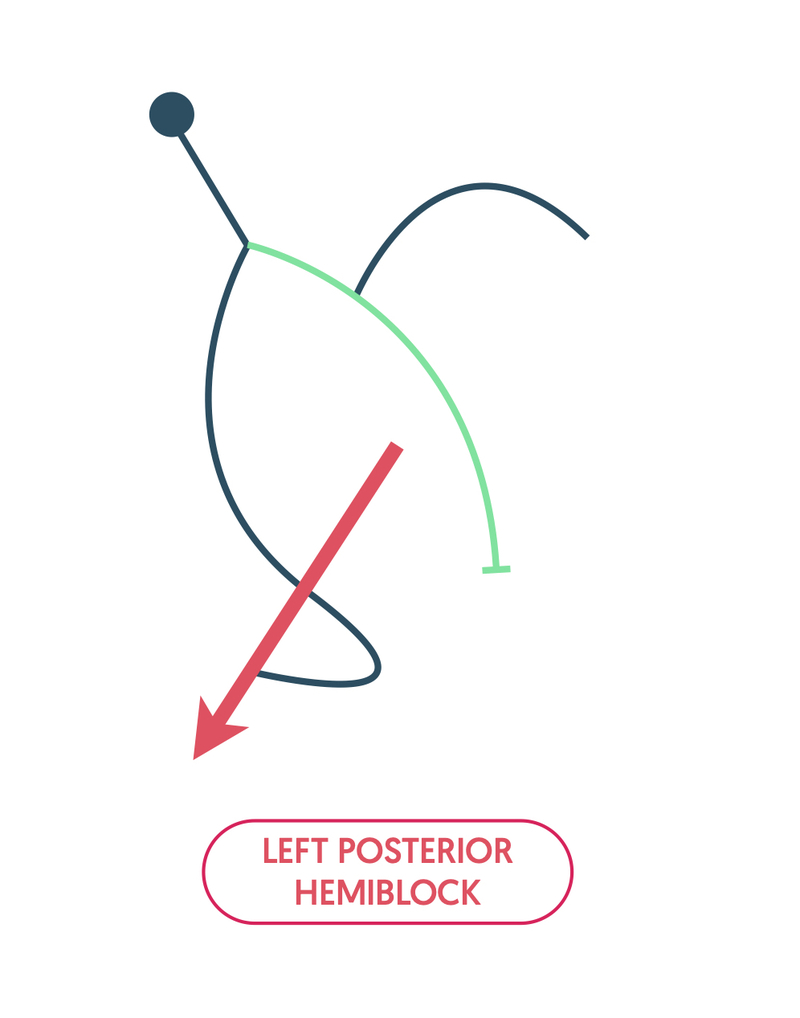
An uncommon conduction abnormality is left posterior hemiblock, which is due to block of the posterior fascicle. This moves the average spread of depolarisation to the right, leading to right axis deviation (RAD) on the ECG.
Block to the right bundle branch and anterior fascicle can lead to bifascicular block. This is seen as a characteristic RBBB pattern and LAD. Block to the right bundle branch, anterior fascicle and delayed conduction through the AVN (seen as first degree heart block), is collectively referred to as trifascicular block. This conduction abnormality is high risk for deteriorating into complete heart block.
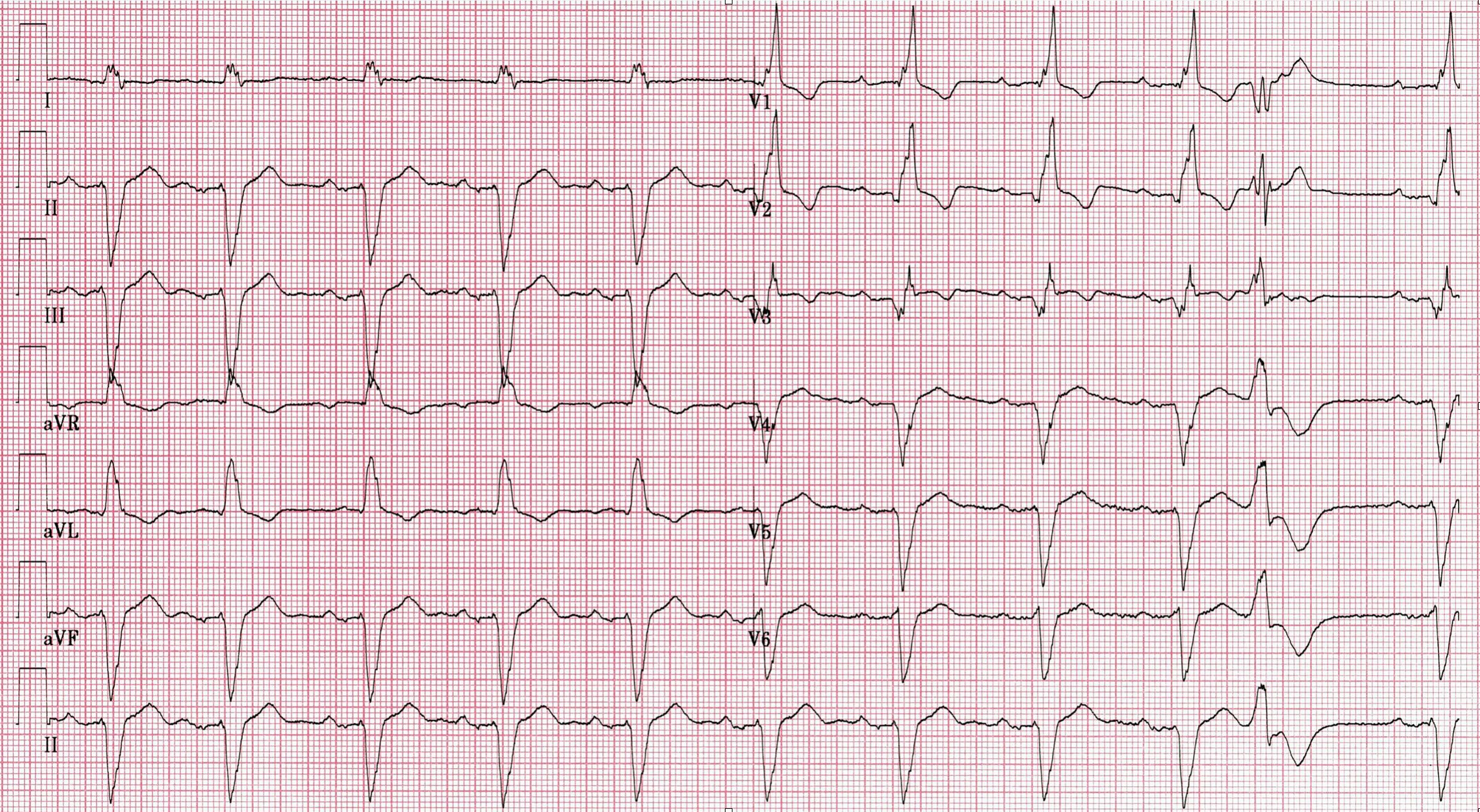
12 Lead ECG showing trifascicular block.