Systemic lupus erythematosus (SLE)
This is a chronic systemic autoimmune disease, which is classically seen in middle-aged women, particularly in black and Hispanic demographic groups.
Whilst the exact cause is unknown, poorly cleared apoptotic debris activates autoimmune lymphocytes leading to the generation of immune complexes.
Inadequate clearance (due to deficient complement proteins) means that these immune complexes are deposited in multiple tissues, leading to inflammation.
It can also be drug induced, which is associated with higher anti-nuclear antibodies than anti-double stranded DNA antibodies.
It typically displays a relapsing and remitting pattern of disease.
Symptoms
Inflammatory signs – fever, weight loss, fatigue
Malar “butterfly rash” on exposure to sunlight
Oral/nasal ulcers
Polyarthritis (> 2 joints), pleurisy, pericarditis
Neurological symptoms – seizures, psychosis
Renal damage – lupus nephritis causes a glomerulonephritis and can cause renal failure
Lymphadenopathy

Key tests
Raised inflammatory markers e.g., ESR, CRP and low C3/C4 complement levels
Raised anti-nuclear (ANA), anti-extractable nuclear antigen (anti-ENA) antibodies
Anti-double stranded DNA antibodies (anti-dsDNA) are highly specific for SLE
Urinalysis should be performed to assess renal involvement
CXR to assess for any cardiopulmonary symptoms
Lymph node biopsy may be performed if diagnosis unclear
Management
Conservative measures – avoid exposure to sunlight, psychological therapies
1st line medical therapy is hydroxychloroquine.
If severe, requires immunosuppression, e.g., steroids, biologics
Sjogren’s syndrome
This is an autoimmune disorder which is characterised by lymphocyte infiltration and fibrosis of the exocrine glands, usually the lacrimal and salivary glands.
Primary – this occurs more in middle-aged females (around 40–50 years old)
Secondary – due to rheumatoid arthritis or other connective tissue disorders
The major risk of this condition is the development of non-Hodgkin’s lymphoma
Symptoms
Dry eyes (keratoconjunctivitis sicca)
Joint and muscle pain
Dry mouth (xerostomia)
Renal tubular acidosis
Raynaud’s phenomenon
Sensory neuropathy
Key tests
Blood tests show raised autoantibodies, including rheumatoid factor, ANA, anti-Ro (SSA) antibodies and anti-La (SSB)
Schirmer’s test uses filter paper to measure tear formation in eyes. The test is positive if less than 5 mm of paper is wetted after 5 minutes.
Management
1st line is symptom control, e.g., artificial tears drops and saliva stimulants
If severe with arthralgia, immunosuppressants (hydroxychloroquine) are considered
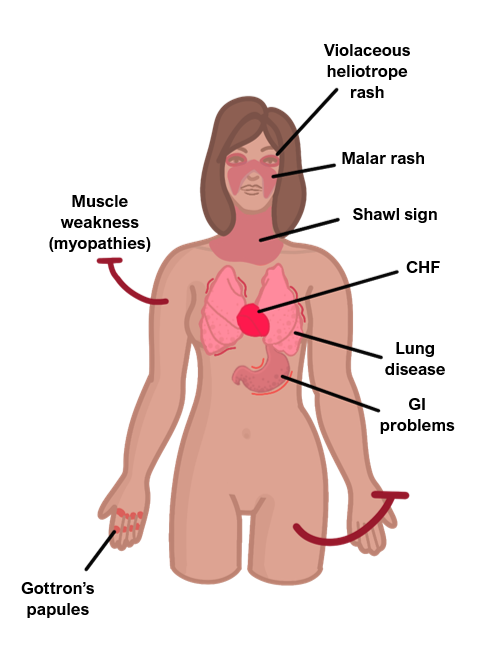
Dermatomyositis
This is an autoimmune condition which leads to inflammation of striated muscle as well as an involvement of the skin.
It can solely affect the musculature without skin involvement (polymyositis).
It can be associated with cancer and so it is important to investigate for an underlying malignancy.
Symptoms
Inflammatory signs – low grade fever, lethargy, weight loss
Progressive symmetrical proximal muscle weakness
Weakness is profound and maybe accompanied with mild pain (though not always)
Gottron papules – red marks on knuckles, elbows and knees
Heliotrope rash – rash of the upper eyelids
Associated with interstitial lung fibrosis and myocarditis
Key tests
Blood tests – raised creatinine kinase levels (up to 50Å~ upper limit of normal)
Muscle biopsy – shows endothelial hyperplasia in the intramuscular blood vessels and perifascicular atrophy
If diagnosis unclear, can also do electromyogram or imaging (MRI of the muscle)
Management
Acute flares are usually managed with steroids
Mainstay of treatment is immunosuppression, e.g., methotrexate
Screen for underlying cancer and organise investigations accordingly
Systemic sclerosis/scleroderma
This is an autoimmune disorder characterised by sclerosis (hardening) of the skin and fibrosis of visceral organs, which is more common in middle-aged females.
Fibroblast activation leads to deposition of collagen, causing progressive fibrosis and organ damage.
Limited type
In this type, skin involvement is limited to hands and face with later organ fibrosis.
This type is associated with anti-centromere antibodies.
Called CREST syndrome: Centromere antibodies, Raynaud’s, Esophagus dysmotility, Sclerodactyly (finger thickening), skin Telangiectasia (capillary dilation)
Diffuse type
In this type, there is early visceral involvement and widespread skin changes.
It can lead to pulmonary fibrosis/hypertension as well as Raynaud’s and GI problems.
It is associated with antibodies to DNA topoisomerase I.
Management
Immunosuppressants
Fibromyalgia
This is a condition which is characterised by chronic widespread pain and a heightened pain response to pressure stimuli, which is more common in women.
Its aetiology is not fully understood, and the pain appears to result from the way pain signals are processed by the central nervous system.
The condition is referred to as a “central sensitisation syndrome”.
It is a clinical diagnosis based on ruling out other pathologies. Investigations are typically normal, so the pain cannot be attributed to any other organic cause.

Symptoms
Pain that is chronic (>3 months) and widespread (bilateral, proximal and distal)
Profound fatigue, difficulty concentrating, poor sleep, low mood, headaches
Key tests
Diagnosis of exclusion as investigations will be normal
Management
Multidisciplinary approach to improve overall functioning.
CBT – psychological support
Neuropathic agents, e.g., amitriptyline, pregabalin, gabapentin etc.
Chronic fatigue syndrome
This is like fibromyalgia, but the prominent problem is fatigue, rather than pain.
It is characterised by persistent fatigue lasting > 6 months and present more than 50% of the time. It is also associated with poor sleep, low mood etc.
The management is similar to fibromyalgia with a MDT approach used, except from the use of pharmacological agents.

