Achondroplasia
This is the most common cause of dwarfism, which occurs due to a gene mutation in the receptor that converts cartilage to bone during development.
It is due to an activating mutation (usually sporadic) in FGF3 (autosomal dominant).
This gene is found in chondrocytes and inhibits growth favouring differentiation.
Whilst endochondral ossification is affected, there is normal intramembranous bone formation meaning that patients have a normal skull and torso but short limbs.
It leads to dwarfism with short limbs but a normal head and chest size.
Symptoms
Short limbs with normal head and chest
Management
Growth hormone therapy (somatotropin)
Osteogenesis Imperfecta
This is a congenital defect of bone formation due to an autosomal dominant mutation in collagen type 1 synthesis.
This results in very weak bones structurally, which predisposes to fracture.
Symptoms
Multiple fractures in bones
Skin that bruises easily
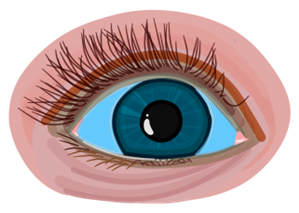
Blue sclera
Hearing loss due to inner ear bone fractures
Management
No cure, but fractures are managed and lifestyle changes
Osteopetrosis
This is an inherited defect of bone resorption which causes abnormally thick, heavy bone which often fractures
Mutations in genes lead to poor osteoclast function, shift balance to bone formation
It is often caused by mutation of carbonic anhydrase II, leads to decreased resorption of bicarbonate, leading to renal tubular acidosis type II
Symptoms
Multiple fractures
Anemia, leukopenia – due to bone marrow being replaced with hard bone
Vision and hearing impairment – due to pressure on cranial nerves
Hydrocephalus – due to narrowing of the foramen magnum which occurs with skull enlargement
Management
Bone marrow transplant can be used to regenerate functioning osteoclasts
Paget’s Disease of Bone
This is a condition due to an imbalance between osteoclast and osteoblast function.
There is increased bone turnover due to higher numbers of osteoblasts and osteoclasts leading to bone remodeling, often caused by mutations in RANK ligand.
This gives rise to a thick, sclerotic bone that fractures easily.
It is usually seen in late adulthood and is more common in cooler climates.
It usually involves one or more bones, rather than the entire skeleton.
Symptoms
Deep, bone pain caused by microfractures
Enlargement of pelvis, femur, tibia and skull – increases hat size and can cause hearing loss
Can lead to osteosarcoma and high output heart failure – due to AV shunts within bone
Key tests
Normal Calcium, phosphate and PTH, but ALP is markedly raised
X-ray shows bone enlargement and cortex thickening with sclerosis and deformity
Management
Medical management includes bisphosphonates (e.g., alendronate to inhibits osteoclasts) and calcitonin (inhibits osteoclast functioning)
Osteoporosis
This is a reduction in overall bone mass, which increases the risk of bone fracture.
Women lose trabecular bone with age, but men have more stable trabeculae during their lifetime, reducing the risk of osteoporosis.
Osteoporosis leads to the majority of fragility fractures in the elderly, e.g., vertebrae, hip and distal radius.
Causes
Can by primary (age-related) or secondary to other conditions or drugs. A useful mnemonic to remember is (SHATTERED)
Causes (SHATTERED)
Key tests
Blood tests show normal Ca2+, PO43-, PTH and ALP levels
DEXA scan measures bone density to give a T-score, a statistical score of how many standard deviations bone density is away from normal
T score between -2.5 and -1 is suggestive of osteopenia
T score < -2.5 suggests osteoporosis
Management
Lifestyle – stop smoking and drinking and increase weight bearing exercises
Ensure levels of vitamin D and calcium are optimised
Medical management is bisphosphonates (e.g., alendronate)
If unsuitable, options include denosumab, strontium ranelate (stimulates osteoblasts) or raloxifene (if post-menopausal).
Hormone replacement therapy can be used in younger postmenopausal women.
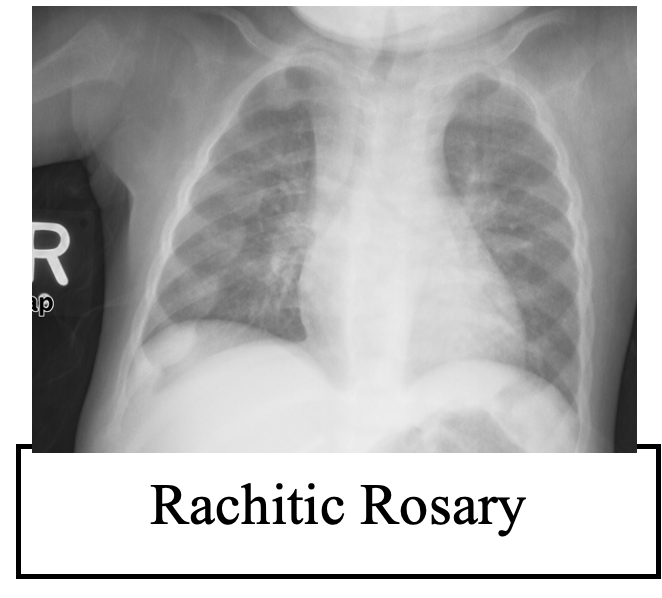
Rickets/Osteomalacia
This is a disease which occurs due to defective mineralisation of osteoid with calcium.
It occurs due to low levels of vitamin D resulting in low serum Ca2+ and PO43-.
In children, it causes the disease rickets, which causes symptoms like growth retardation and bowing of the legs.
Causes
Decreased sun exposure, poor diet, malabsorption (coeliac disease) and renal failure
Vitamin D-resistant rickets – due to low renal 1a-hydroxylase activity or receptor resistance
X-linked hypophosphateaemic rickets – dominantly inherited, defect in renal phospate handling
Symptoms
Bone pain and weak bones increasing risk of fracture
Key tests
Blood tests show low Ca2+, low Phosphate, high PTH and ALP levels
X-ray show loss of cortical bone and partial non-displaced fractures on the scapulaand femoral shaft (Looser’s zones)
Management
Vitamin D supplements
Osteomyelitis
This refers to inflammation of bone tissue, usually due to an infection of the bone.
Bacteria can enter the bone from the blood, from local skin infections (cellulitis) or from trauma (such as surgery/fractures).
The most common pathogen is Staphylococcus aureus, but others include Pseudomonas, E. coli as well as N. gonorrhoeae (in sexually active adults).
Causes
Staph Aureus (90%)
N gonorrhoeae (sexually active adults)
Pseudomonas (diabetes)
Symptoms
Bone pain with systemic signs of infection (High WBC and fever)
Key tests
Bloods show raised inflammatory markers. Blood cultures to assess for bacteraemia
X-ray and CT can be used, but MRI is the best imaging modality
Management
IV antibiotics (often prolonged course). May require surgery in severe cases.

